- Squamous Metaplasia in Endometrium is caused by various conditions. The treatment depends upon the underlying cause of the metaplasia
- In many cases, the treatment involves hormonal manipulation (restoring any hormonal imbalance in the body)
- No specific treatment may be necessary for some forms of uterine metaplasias, unless abnormalities are noted
- Also, if the underlying cause is not associated with any signs and symptoms, then treatment may not be required
What are the treatment options for squamous metaplasia of uterine cervix?
No specific treatment is necessary for Squamous Metaplasia of Uterine Cervix, since the condition is not associated with any signs and symptoms, unless any abnormalities are noted. How can Squamous Metaplasia of Uterine Cervix be Prevented?
What is squamous metaplasia of the endometrium?
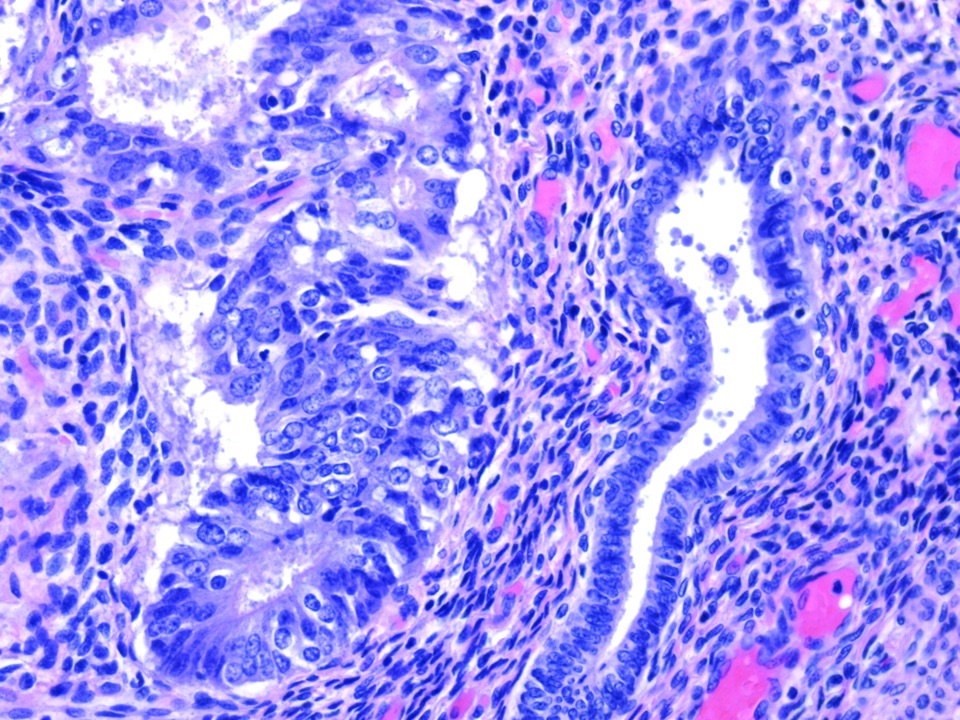
There is squamous metaplasia of the endometrium with cellular debris in the uterine lumen and a few associated inflammatory cells. Uterus, Endometrium - Metaplasia, Squamous in a female Sprague Dawley rat from a chronic study.
What are the symptoms of squamous metaplasia of the uterus?
The condition is benign, but the zone of transformation of this metalastic change has increased risk of contracting human papilloma virus (HPV) infection, a sexually transmitted disease. Untreated HPV infection increases risk of cervical cancer. Squamous metaplasia of uterine cervix does not produce any symptoms.
What is metaplasia of uterine cervix?
A metaplasia is defined as the change of one type of epithelium to another type of epithelium. Squamous Metaplasia of Uterine Cervix is a benign condition and there is no risk for a malignant transformation
Should I be worried about squamous metaplasia?
There is no risk of malignant transformation for squamous metaplasia. Nevertheless, the metaplastic change within the endocervix may increase the risk for human papilloma virus infection (Hwang et al., 2012), which is a risk factor for cervical cancer.
What causes squamous metaplasia in the cervix?
Factors in the initiation and promotion of squamous metaplasia are chronic irritation of a physical nature, such as that caused by an intrauterine contraceptive device (IUD), chemical irritants, inflammation with cell destruction, and endocrine changes at the beginning of, during, and after reproductive age.
Is squamous metaplasia of cervix precancerous?
Changes to epithelial cells that line organs, glands and skin cause squamous metaplasia. It may be a noncancerous or precancerous condition. In women with HPV, squamous metaplasia raises the risk of cervical dysplasia and cervical cancer.
What is squamous metaplasia uterus?
Squamous metaplasia in the cervix refers to the physiological replacement of the everted columnar epithelium on the ectocervix by a newly formed squamous epithelium from the subcolumnar reserve cells. The region of the cervix where squamous metaplasia occurs is referred to as the transformation zone.
Is squamous metaplasia reversible?
Metaplasia is reversible when the stimulus for it is taken away. Dysplasia: a disordered growth and maturation of an epithelium, which is still reversible if the factors driving it are eliminated.
Is metaplasia benign or malignant?
When cells are faced with physiological or pathological stresses, they respond by adapting in any of several ways, one of which is metaplasia. It is a benign (i.e. non-cancerous) change that occurs as a response to change of milieu (physiological metaplasia) or chronic physical or chemical irritation.
Should I get a hysterectomy if I have precancerous cells?
If the precancerous disease is more extensive or involves adenocarcinoma in situ (AIS), and the woman has completed childbearing, a total hysterectomy may be recommended. 1 During a total hysterectomy, the entire uterus (including the cervix) is removed.
What does squamous metaplasia on a Pap smear mean?
The phrase “endocervical cells present” simply means that your doctor sampled cells from the inside of your cervix during the Pap smear. The phrase “squamous metaplastic cells present” means that the pathologist who examined your Pap smear found cells that were growing and repairing themselves regularly.
How serious are precancerous cells?
Often, precancerous lesions are not invasive and a person will not develop cancer. In some cases these precancerous cells, if left alone, may go on to become “invasive” cancer cells. Sometimes, it may take these cells a few years, or even decades to progress.
Is squamous metaplasia caused by HPV?
The area of manifest or potential squamous metaplasia, referred to as transformation zone, is the site where most squamous cancers occur after a transforming HPV infection of proliferating reserve cells and/or metaplastic epithelium.
What is endocervical polyp with squamous metaplasia?
Endocervical polyps (ECPs) are routine and common specimens in gynecologic pathology. Microscopically, these benign proliferations show a fibrovascular stalk and endocervical glands, and are on occasion accompanied by squamous metaplasia, chronic inflammation, or ulceration if irritated.
What squamous means?
Definition of squamous 1a : covered with or consisting of scales : scaly. b : of, relating to, or being a stratified epithelium that consists at least in its outer layers of small scalelike cells.
How is Squamous Metaplasia of Uterine Cervix Treated?
No specific treatment is necessary for Squamous Metaplasia of Uterine Cervix, since the condition is not associated with any signs and symptoms , unless any abnormalities are noted.
What are the Signs and Symptoms of Squamous Metaplasia of Uterine Cervix?
No significant signs and symptoms are associated with Squamous Metaplasia of Uterine Cervix.
What is a mature squamous metaplasia?
Mature squamous metaplasia: It is a condition where the squamous epithelium is well-formed and mature. Immature squamous metaplasia: It is a condition where the change from glandular epithelium to squamous epithelium is actively occurring .
What is squamous metaplasia of the cervix?
What is Squamous Metaplasia of Uterine Cervix? (Definition/Background Information) Squamous Metaplasia of Uterine Cervix is a common, benign condition, wherein the glandular epithelium of cervix changes into squamous epithelium of cervix. It is a physiological condition.
What is a squamous epithelium?
The squamous epithelium shows immature features , which means that there is a combination of glandular features and squamous features within the cells. Atypical squamous metaplasia: In this condition, the squamous epithelium shows atypical features such as abnormal nucleus and mitotic activity.
What is the most common cancer in the cervix?
A vast majority of cancers arising from the cervix (almost 70 %) are squamous cell carcinomas. The second most common type is adenocarcinoma.
Is atypical squamous metaplasia premalignant?
Atypical squamous metaplasia could potentially be a premalignant stage to squamous cell carcinoma of cervix. Many clinical conditions may have similar signs and symptoms. Your healthcare provider may perform additional tests to rule out other clinical conditions to arrive at a definitive diagnosis.
How is Squamous Metaplasia in Endometrium Diagnosed?
Squamous Metaplasia in Endometrium is diagnosed by a pathologist on examination of endometrial tissue under a microscope . This is established through the following procedures:
What are the Signs and Symptoms of Squamous Metaplasia in Endometrium?
Generally, there are no significant signs and symptoms directly associated with Squamous Metaplasia in Endometrium
What is the term for a change in cell type in the endometrium?
Metaplasia in endometrium is a common benign condition that occurs in the glands of the endometrial lining (of the uterus). Metaplasia is defined as a change of one cell type to another cell type
What are the risk factors for squamous metaplasia?
The risk factors for Squamous Metaplasia in Endometrium may include the following conditions: It is important to note that having a risk factor does not mean that one will get the condition. A risk factor increases ones chances of getting a condition compared to an individual without the risk factors.
What is endometrial biopsy?
An endometrial tissue biopsy is performed and sent to a laboratory for a pathological examination. A pathologist examines the biopsy under a microscope. After putting together clinical findings, special studies on tissues (if needed) and with microscope findings, the pathologist arrives at a definitive diagnosis.
What is the term for the period when the endometrium sheds?
Menstruation, where periodic shedding of the endometrium takes place
How are the fallopian tubes studied?
In this procedure, the structure of the uterus and fallopian tubes are studied by using a dye and X-ray images. Many clinical conditions may have similar signs and symptoms. Your healthcare provider may perform additional tests to rule out other clinical conditions to arrive at a definitive diagnosis.
Why does squamous metaplasia occur?
Most often squamous metaplasia of uterine cervix is known to develop as a result of hormonal changes occurring particularly during puberty period. Imbalance of hormones during puberty is common phenomenon. This physiological state of cervix is present in women all over the world.
What is metaplasia in medicine?
In medicine metaplasia is a defined as a change wherein one form of epithelium changes or transforms into other form. In this case the mucus secreting glandular cells into squamous cells. The condition is benign, but the zone of transformation of this metalastic change has increased risk of contracting human papilloma virus (HPV) infection, ...
Is squamous metaplasia a complication?
Symptoms & Complications Of Cervical Squamous Metaplasia. As such squamous metaplasia of uterine cervix does not present with any particular symptom. There is as such no complication from the condition. But during the epithelial cell replacement (metaplasia), the point at which or the zone around which the change takes place is vulnerable ...
Does squamous metaplasia of the uterus produce symptoms?
Squamous metaplasia of uterine cervix does not produce any symptoms. No treatment is necessary for squamous metaplasia of uterine cervix, unless HPV is detected.
Is squamous metaplasia of the uterine cervix a sexually?
Squamous metaplasia of uterine cervix in itself does not require any specific treatment, unless any other cellular abnormality is detected. The condition is considered to be benign. However, in view of more vulnerability towards contracting HPV infection which is a sexually transmitted disease, safe sexual practices is necessary. Use of condoms, avoiding multiple partners, is helpful in preventing HPV infection. HPV infection in cervical region increases risk of cervical cancer.
What is immature squamous metaplasia?
Immature squamous metaplasia represents the morphologic spectrum of epithelial changes from a single or multiple layers of reserve cells to an epithelium composed of three or more layers of cells with features of mature nonkeratinizing squamous epithelial cells ( Figs 8.23 to 8.25; see also Fig. 8.30 ). Unlike reserve cells, cells derived from areas of immature squamous metaplasia are more often isolated ( Figs 8.26 to 8.28 ). Their tendency to occur as single cells is correlated with the degree of maturation of the parent epithelium. The majority of cells are round to oval, with the number of polygonal cells increasing with maturation. The cytoplasm of immature squamous metaplasia cells is dense, homogeneous but sometimes vacuolated, and cyanophilic in staining reaction ( Fig. 8.29 ). Cytoplasmic vacuolation is frequently observed in the presence of inflammation or as a consequence of degeneration. Nuclei, particularly in the more immature cells, are large, creating a high nucleocytoplasmic ratio (see Fig. 8.28 ). In cervical smears, cells from immature squamous metaplasia changes often demonstrate some degree of atypia. Cells and nuclei show a slight irregularity in size and shape, which is understandable because most metaplastic changes occur under the influence of some irritating factor ( Fig. 8.30; see also Fig. 8.29 ). Differential diagnosis with dysplastic changes should be made on the basis of the evenly distributed, finely granular, nonhyperchromatic chromatin.
Which type of hyperplasia is transformed into mature squamous metaplasia?
Reserve cell hyperplasia is transformed in immature squamous metaplasia, which with increasing differentiation gradually evolves into mature squamous metaplasia. The maturation of immature squamous metaplasia tends to be more pronounced in the distal part of the endocervical canal.
What is the difference between atypical squamous metaplasia and nucleus?
Absolutely, the nuclei in atypical squamous metaplasia are much smaller than nuclei in dysplastic changes. In squamous metaplasia, hyperchromasia is generally absent. Hyperchromasia in nuclei of dysplastic cells reflects an abnormality in DNA synthesis, for example, an abnormal number of chromosomes in that particular nucleus.
What is the mature squamous epithelium?
Mature squamous epithelium encompasses the classic three layers of nonkeratinizing squamous epithelium, making mature squamous metaplastic epithelium virtually indistinguishable from the original ectocervical squamous epithelium. Foci of mature squamous metaplasia may be indistinguishable from the normal ectocervical mucosa. The only clue to its metaplastic origin is underlying endocervical glands ( Fig. 8.31 ).
What is the most common protective mechanism of the endocervical epithelium of the uterine?
The most common protective mechanism of the endocervical epithelium of the uterine cervix is squamous metaplasia. The term metaplasia implies the transformation of one cell type into another type of cell, the latter being of a lower organizational order. As applied to the uterine cervix, the term refers to the process of replacement of simple columnar epithelium lining the endocervical canal and glands by a stratified squamous epithelium.
What percentage of cervical smears show squamous metaplasia?
The presence of squamous metaplasia in cervical smears was reported by von Haam and Old to be 41.5%. 16 Howard and co-workers reported an 83% incidence, 17 and Carmichael and Jeaffreson found it to be present in 41% of cervices examined histologically. 18
Where is squamous metaplasia found?
Squamous metaplasia and regenerative change in the ducts occurs in rats afflicted with sialodacryoadenitis. 116 It can also be located in the ducts of the sublingual glands in the Wistar rat in the absence of obvious sialodacryoadenitis or evidence of any specific disease. Similar regenerative hyperplastic duct changes are also seen in necrotic and inflammatory conditions in the dog salivary gland. 128
What modifier should be included in the diagnosis of uterus, endometrium, and metaplasia?
recommendation: Uterus, Endometrium - Metaplasia, Squamous should be diagnosed and given a severity grade whenever present. The modifier "squamous" should be included in the diagnosis to clearly define the lesion and eliminate potential confusion.
What is the cause of squamous metaplasia?
Vitamin A deficiency also causes squamous metaplasia. The lesion is characterized by the replacement of the normally columnar endometrial epithelium by squamous epithelium. In some cases, the endometrial glands can also be affected ( Figure 7.
Is the endometrium squamous?
Uterus Endometrium - Metaplasia, Squamous in a female Harlan Sprague-Dawley from a chronic study. There is squamous metaplasia of the endometrium.
Is squamous metaplasia of the endometrium focal?
There is squamous metaplasia of the endometrium with cellular debris in the uterine lumen and a few associated inflammatory cells. Uterus, Endometrium - Metaplasia, Squamous in a female Sprague Dawley rat from a chronic study. There is focal squamous metaplasia of the endometrium.
Is squamous epithelium in the uterus?
There are cellular debris and squames in uterine lumen, which is lined by squamous epithelium.
Is uterus metaplasia squamous?
Uterus - Metaplasia, squamous in a female Harlan Sprague-Dawley rat from a chronic study. There is squamous metaplasia of the endometrial glands.
What are the essential features of squamous epithelium?
Stratified squamous epithelium replacing overlying preexisting endocervical glands in the stroma. Absence of nuclear abnormalities and brisk mitotic activity. Physiological change due to estrogenic milieu and vulnerable to HPV infection.
Can cervical stroma be identified on endocervical biopsy?
May be identified on endocervical biopsy or curettage, particularly in case of cervical stroma involvement
How to treat cervical metaplasia?
Particular attention should be paid to the treatment of cervical metaplasia with celandine. Use infusion celandine: half a glass of dry leaves celandine pour a liter of boiling water and take inside two teaspoons twice a day.
What causes metaplasia of the cervix?
Causes of metaplasia of the cervix are definitely difficult to establish, but to date, one of the proven etiological factors is infection with the human papillomavirus, which plays a key role in the further progression of changes within the cell.
How does cervical metaplasia develop?
The pathogenesis of the development of cervical metaplasia begins with a trigger factor, which can be a viral agent. In this case, the virus penetrates into the cell, where its nucleic acid enters the nucleus by disrupting the integrity of the nuclear envelope.
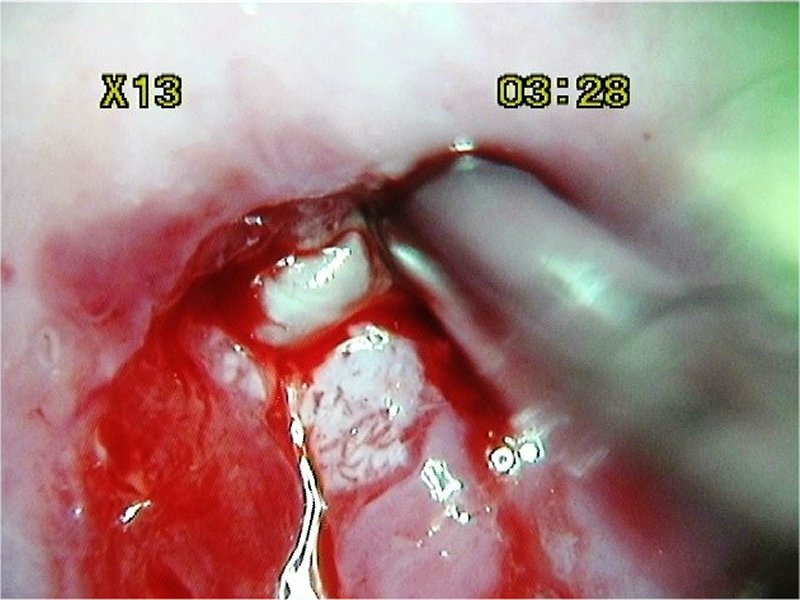
How to diagnose metaplasia?
Colposcopy is the diagnosis of the cervix by a special device that has a magnifying power of 2 to 32 times, depending on the power. This increase allows you to see those areas of metaplasia, which are not determined by routine examination in the mirrors. In addition to simple colposcopy, an extended one is also performed. In this case, the site of the examined epithelium of the cervix is colored with trichloroacetic acid, iodine or Lugol solution, and look at the degree of coloration. The sites of metaplastic epithelium will be pale against a normally colored epithelium. Such a diagnosis can confirm the presence of metaplasia, even if visually nothing can be found.
Why is metaplasia dangerous?
Metaplasia of the cervix is a dangerous condition for the very reason that often the morphological changes that develop are much faster than the development of at least a minimal clinical symptomatology. This is one of the reasons for introducing mandatory screening for this pathology.
Which type of metaplasia is the most differentiated?
Squamous cell metaplasia of the cervix is the most differentiated variant, since the epithelium has all the characteristics of normal cells, with the exception of location. Thus, in squamous cell metaplasia of the cervix, the flat multilayered epithelium is determined beyond the intermediate zone in the region of the cervical canal among the cylindrical epithelium.
What are the nonspecific and specific preventions of metaplasia?
Prevention of metaplasia may be specific and nonspecific. Nonspecific prevention is a modification of the way of life with the exception of risk factors. Such risk factors that are subject to modification are the exclusion of bad habits, proper nutrition, exclusion of the work of women in industry with hazardous substances. It is also necessary to monitor the hygiene of sexual activity, because its early onset and frequent change of sexual partners is a risk factor not only for metaplasia of the cervix, but for cervical cancer and breast cancer. Sexual life should be safe in terms of possible infections - avoid infection with the human papilloma virus as much as possible.