
Most outpatients with community-acquired pneumonia do not require microbiologic testing of sputum or blood and can be treated empirically with a macrolide, doxycycline, or a respiratory fluoroquinolone. Patients requiring hospitalization should be treated with a fluoroquinolone or a combination of beta-lactam plus macrolide antibiotics.
What are the most common causes of community acquired pneumonia?
Most adults with community-acquired pneumonia are treated as outpatients. Despite this, the majority of studies regarding community-acquired pneumonia have been in hospitalized patients only and may not be applicable to an ambulatory population. This review critically examines the literature regarding the diagnosis, cause, appropriate patient selection, and treatment of …
How to treat community acquired pneumonia?
· Cochrane Database Syst Rev 2014; :CD002109. File TM, Goldberg L, Das A, et al. Efficacy and Safety of Intravenous-to-oral Lefamulin, a Pleuromutilin Antibiotic, for the Treatment of Community-acquired Bacterial Pneumonia: The Phase III Lefamulin Evaluation Against Pneumonia (LEAP 1) Trial.
What is the first line treatment for pneumonia?
Pneumonia is a leading cause of morbidity and mortality in the US and a primary cause of hospitalization nationwide. A recent guideline update from the American Thoracic Society and Infectious Diseases Society of America provides evidence-based recommendations for managing adults with community-acquired pneumonia in the outpatient setting.
What are the treatments for MRSA pneumonia?
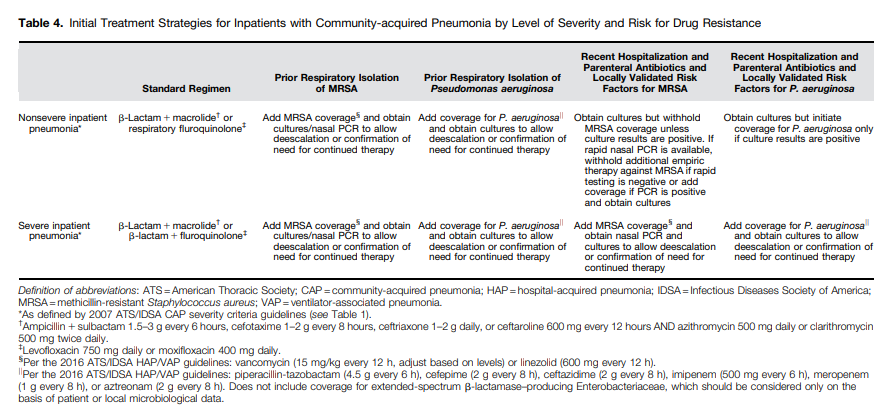
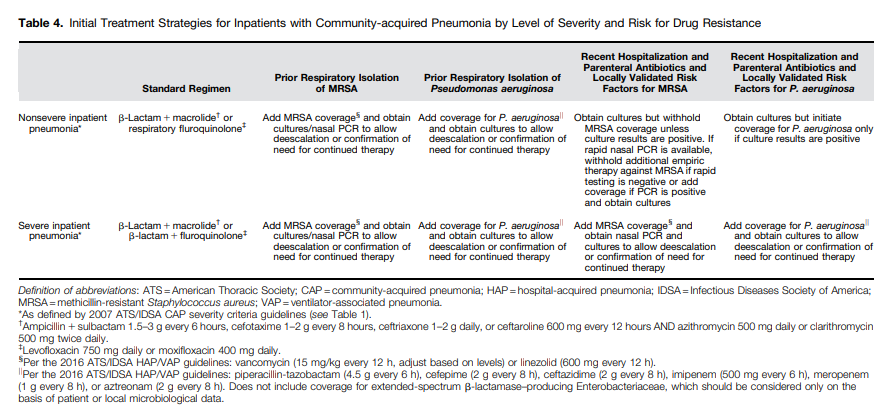
· The Pneumonia Severity Index (mdcalc.com/psi-port-score-pneumonia-severity-index-cap) is recommended over the CURB-65 (mdcalc.com/curb-65-score-pneumonia-severity). Corticosteroids are not recommended routinely in adults with nonsevere or severe CAP. Patients should be treated with antibiotics for at least 5 days and 7 days for MRSA orPseudomonas. …
What is the best treatment for community-acquired pneumonia?
The initial treatment of CAP is empiric, and macrolides or doxycycline (Vibramycin) should be used in most patients.
What is the first line treatment for pneumonia in adults?
The first-line treatment for pneumonia in adults is macrolide antibiotics, like azithromycin or erythromycin. In children, the first-line treatment for bacterial pneumonia is typically amoxicillin.
How is community-acquired pneumonia treated in the elderly?
The treatment should include a respiratory fluoroquinolone (levofloxacin or moxifloxacin) as monotherapy or the combination of a β-lactamic (third-generation cephalosporin, ertapenem or ampicillin/sulbactam) medication and a macrolide (azithromycin or clarithromycin).
Which drug is the best choice for monotherapy treatment of community-acquired pneumonia CAP?
Fluoroquinolones, especially respiratory fluoroquinolones (moxifloxacin, gemifloxacin, and levofloxacin) act against the major causative agents of CAP (including major causative bacteria, MP, CP and Legionella Pneumophila) and they are widely used as a monotherapy for patients with CAP.
How is pneumonia outpatient treated?
Initial outpatient therapy should include a macrolide or doxycycline. For outpatients with comorbidities or who have used antibiotics within the previous three months, a respiratory fluoroquinolone (levofloxacin, gemifloxacin, or moxifloxacin), or an oral beta-lactam antibiotic plus a macrolide should be used.
What's the best antibiotic to treat pneumonia?
In otherwise uncomplicated pneumonia, azithromycin is the initial drug of choice, as it covers most of the potential etiologic agents, including Mycoplasma species.
How is pneumonia treated in adults?
The options include:Antibiotics. These medicines are used to treat bacterial pneumonia. ... Cough medicine. This medicine may be used to calm your cough so that you can rest. ... Fever reducers/pain relievers. You may take these as needed for fever and discomfort.
What is the most important action an older adult can take to prevent pneumonia and the flu )?
Pneumococcal pneumonia is an example of a serious flu-related complication that can cause death. You can get the pneumococcal vaccine your provider recommends when you get a flu vaccine.
Can you take azithromycin and doxycycline together for pneumonia?
No interactions were found between azithromycin and doxycycline. However, this does not necessarily mean no interactions exist. Always consult your healthcare provider.
What is the first line treatment for hospital acquired pneumonia?
In general, for both hospital-acquired pneumonia (HAP) and VAP, 7 days of treatment with appropriate antibiotics/antibiotics is recommended. This duration may be shortened or lengthened depending on the clinical response of the individual.
Does vancomycin treat pneumonia?
Vancomycin remains the mainstay treatment for methicillin-resistant Staphylococcus aureus (MRSA) infections, including pneumonia.
Can Augmentin and doxycycline be taken together?
doxycycline amoxicillin Combining these medications may reduce the effectiveness of amoxicillin. Your doctor may be able to prescribe alternatives that do not interact. It is important to tell your doctor about all other medications you use, including vitamins and herbs.
Is CAP a serious illness?
CAP is a common and potentially serious illness [ 1-3 ]. It is associated with considerable morbidity and mortality, particularly in older adult patients and those with major comorbidities. (See "Prognosis of community-acquired pneumonia in adults" .) The treatment of CAP in adults in the outpatient setting will be reviewed here.
What is CAP in medical terms?
Community-acquired pneumonia (CAP) is defined as an acute infection of the pulmonary parenchyma in a patient who has acquired the infection in the community, as distinguished from hospital-acquired (nosocomial) pneumonia (HAP).
What is the psi score for pneumonia?
The Pneumonia Severity Index (mdcalc.com/psi-port-score-pneumonia-severity-index-cap) is recommended over the CURB-65 (mdcalc.com/curb-65-score-pneumonia-severity). Corticosteroids are not recommended routinely in adults with nonsevere or severe CAP. Patients should be treated with antibiotics for at least 5 days and 7 days for MRSA orPseudomonas.
How much did pneumonia cost in 2013?
In 2013, pneumonia had an aggregate cost of nearly $9.5 billion for 960,000 hospital stays. 1. The American Thoracic Society (ATS) and the Infectious Disease Society of America (IDSA) recently updated clinical practice guidelines previously published in 2007. 2 The guidelines focus on patients in the United States who are not immunocompromised ...
How to manage CAP?
The following recommendations were published by the ATS and IDSA in October 2019 for the management of CAP: 2 1 Sputum gram stain and cultures are not recommended in adults with CAP managed in an outpatient setting. 2 Blood cultures are not recommended in adults with CAP managed in an outpatient setting. 3 Routine testing urine forPneumococcusorLegionellais not recommended. 4 If influenza is circulating in the community, testing with rapid molecular assay rather than an antigen test is recommended. 5 Serum procalcitonin levels are not recommended to determine the need for initial empiric antibiotic therapy. 6 When deciding the need for hospitalization, clinical judgment plus the results of a validated prognostic tool should be used. The Pneumonia Severity Index (mdcalc.com/psi-port-score-pneumonia-severity-index-cap) is recommended over the CURB-65 (mdcalc.com/curb-65-score-pneumonia-severity). 7 Corticosteroids are not recommended routinely in adults with nonsevere or severe CAP. 8 Patients should be treated with antibiotics for at least 5 days and 7 days for MRSA orPseudomonas. The duration should be guided by validated measures of clinical stability, including ability to eat, blood pressure, heart rate, normal mentation, oxygen saturation, respiratory rate, and temperature. 9 In adults whose CAP symptoms resolve within 5 to 7 days, follow-up chest imaging does not have to be obtained.
What is CAP in healthcare?
Antibiotic recommendations for the treatment of community-acquired pneumonia (CAP) include coverage for the traditional pathogens Chlamydia pneumonia, Haemophilus influenza, Legionella, Moraxella catarrhalis, Mycoplasma pneumonia, Staphylococcus aureus, and Streptococcus pneumonia. Widespread use of the pneumococcal conjugate vaccine has caused ...
Is serum procalcitonin needed for antibiotics?
Serum procalcitonin levels are not recommended to determine the need for initial empiric antibiotic therapy. When deciding the need for hospitalization, clinical judgment plus the results of a validated prognostic tool should be used. The Pneumonia Severity Index (mdcalc.com/psi-port-score-pneumonia-severity-index-cap) is recommended over ...
What antibiotics are used for pneumonia?
Patients requiring hospitalization should be treated with a fluor oquinolone or a combination of beta-lactam plus macrolide antibiotics.
Do corticosteroids help with pneumonia?
For patients with severe community-acquired pneumonia, corticosteroids decrease the risk of adult respiratory distress syndrome and modestly reduce intensive care unit and hospital stays, duration of intravenous antibiotic treatment, and time to clinical stability without increasing major adverse events.
What are the risk factors for pneumonia?
Community-acquired pneumonia is a leading cause of death. Risk factors include older age and medical comorbidities. Diagnosis is suggested by a history of cough, dyspnea, pleuritic pain, or acute functional or cognitive decline, with abnormal vital signs (e.g., fever, tachycardia) and lung examination findings.
What is HCAP in nursing home?
HCAP was defined for those patients who had any one of several potential risk factors for antibiotic-resistant pathogens, including residence in a nursing home and other long-term care facilities, hospitalization for ≥2 days in the last 90 days, receipt of home infusion therapy, chronic dialysis, home wound care, or a family member with a known antibiotic-resistant pathogen. The introduction of HCAP was based on studies identifying a higher prevalence of pathogens that are not susceptible to standard first-line antibiotic therapy, in particular MRSA and P. aeruginosa, in some subsets of patients with CAP ( 123 ). Since then, many studies have demonstrated that the factors used to define HCAP do not predict high prevalence of antibiotic-resistant pathogens in most settings. Moreover, a significant increased use of broad-spectrum antibiotics (especially vancomycin and antipseudomonal β-lactams) has resulted, without any apparent improvement in patient outcomes ( 124 – 133 ).
How long does it take to stop antibacterial therapy?
Randomized controlled studies are needed to establish whether antibacterial therapy can be stopped at 48 hours for patients with CAP who test positive for influenza and have no biomarker (e.g., procalcitonin) or microbiological evidence of a concurrent bacterial infection.
What are the arguments for trying to determine the etiology of CAP?
Arguments for trying to determine the etiology of CAP are that 1) a resistant pathogen may be identified; 2) therapy may be narrowed; 3) some pathogens, such as Legionella, have public health implications; 4) therapy may be adjusted when patients fail initial therapy; and 5) the constantly changing epidemiology of CAP requires ongoing evaluation.
How long should you take antibiotics for CAP?
The recommended duration of antibiotic therapy has not changed from previously published guidelines. Patients with CAP should be treated for a minimum of 5 days, with antibiotic therapy continued until the patient achieves clinical stability.
Can procalcitonin be used for CAP?
The use of procalcitonin is not recommended to determine the need for initial antibiotic therapy in patients with CAP, and empirical antibiotic therapy should be initiated in adults with clinically suspected and radiographically confirmed CAP regardless of serum procalcitonin levels. 4.
What is CAP in pharmacy?
Community-acquired pneumonia (CAP), an infection of the lung parenchyma that occurs in persons outside ...
Can a rapid diagnostic test confirm a patient's illness?
The basis for this recommendation is that no rapid and specific diagnostic test exists to confirm that a patient’s illness is due solely to a virus at the time of presentation, and patients with CAP caused by a virus often have a bacterial coinfection.
What is CAP in healthcare?
ABSTRACT: In 2019, guidelines for the management of immunocompetent adults with community-acquired pneumonia (CAP) were published jointly by the American Thoracic Society and the Infectious Diseases Society of America. Different treatment regimens are recommended depending on whether the patient is receiving treatment in ...
Key Points
- For healthy outpatient adults, treat community-acquired pneumonia (CAP) with amoxicillin or doxycycline or a macrolide (if local pneumococcal resistance to macrolides is less than 25%)
- For patients with comorbidities or risk factors for resistant organisms, treat CAP with a combination of [amoxicillin/clavulanate or cephalosporin] AND [macrolide or doxycycline]; alternatively, tr...
- For healthy outpatient adults, treat community-acquired pneumonia (CAP) with amoxicillin or doxycycline or a macrolide (if local pneumococcal resistance to macrolides is less than 25%)
- For patients with comorbidities or risk factors for resistant organisms, treat CAP with a combination of [amoxicillin/clavulanate or cephalosporin] AND [macrolide or doxycycline]; alternatively, tr...
- Continue antibiotics until the patient becomes clinically stable and for a minimum of 5 days.
Healthy Adults
- For healthy outpatient adults without comorbidities or risk factors for resistant organisms, the guideline outlines three options: 1. Amoxicillin 1 g three times daily is a strong recommendation backed by a moderate quality of evidence 2. Doxycycline 100 mg twice daily is a conditional recommendation based on low quality evidence 3. A macrolide is acceptable if other options ar…
Patients with Comorbidities Or Risk Factors For Antibiotic Resistance
- Patients with comorbidities or risk factors for resistant organisms would benefit from a broader spectrum of antimicrobial coverage. 1. Combination therapy with [Amoxicillin/clavulanate or cephalosporin] AND [macrolide or doxycycline]. The doses are amoxicillin/clavulanate 500 mg/125 mg three times daily or 875 mg/125 mg twice daily or 2,000 mg/125 mg twice daily; cefp…
Duration of Treatment
- The guidelines recommend continuing antibiotics until the patient becomes clinically stable as determined by vital signs, ability to eat, and mental status. The minimum duration of treatment should be 5 days.