Medication
Medicine. There are various kinds you can take. Calcium channel or beta blockers can help correct heart rhythm. If you have SVT only 1 or 2 times a year, you may take beta-blockers or calcium channel medicines by mouth (orally) as needed. If your SVT is more frequent, you may need to take medicine every day. Some people may need to take several medicines to prevent episodes of SVT.
Procedures
- Treatment of dystonia begins with proper diagnosis and classification, an appropriate search for underlying etiology, and an assessment of the associated functional impairment.
- The therapeutic approach must be tailored to the individual needs of the patient.
- Physical therapy and occupational therapy can be useful in many patients.
Therapy
Specimen validity testing (SVT) is performed on a urine drug screen specimen to detect substitution, adulteration, or dilution. See the Drugs of Abuse Reference Guidefor additional information on SVT.
Nutrition
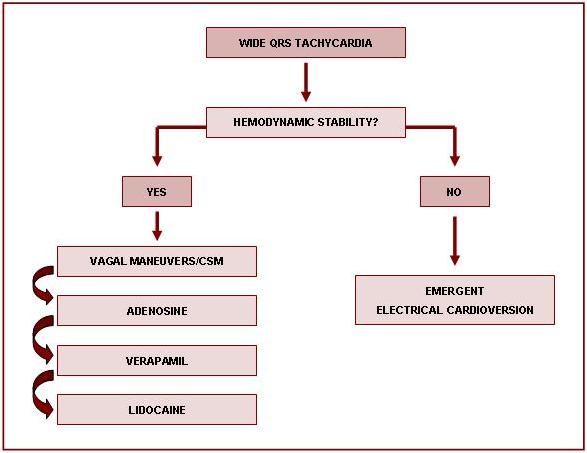
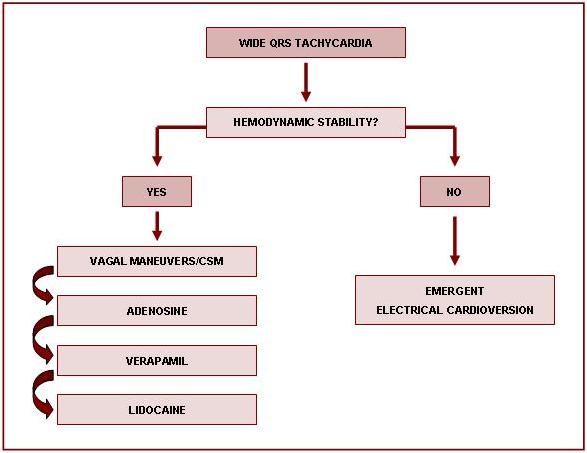
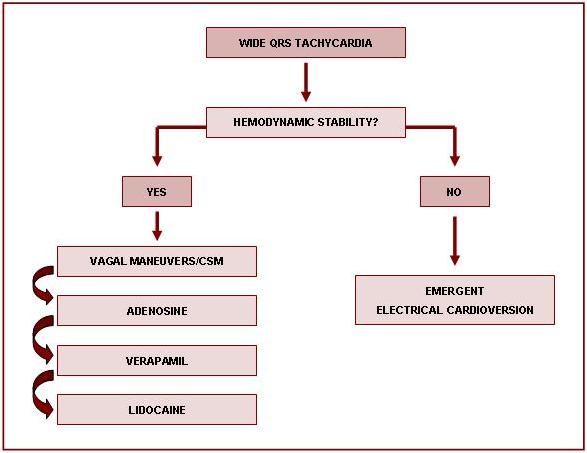
Treatment of Supraventricular Tachycardia
- Unstable Supraventricular Tachycardia. The initial steps a healthcare provider should take in caring for a conscious adult patient with a pulse are to complete the ACLS Primary and Secondary Assessments, ...
- Stable Supraventricular Tachycardia. ...
- Next Steps and Considerations. ...
See more
How long do you have to take medication for SVT?
Which medications are used to treat tardive dystonia?
What does SVT stand for in drug?
How to treat SVT with adenosine?
What is the best medication for SVT?
In most patients, the drug of choice for acute therapy is either adenosine or verapamil. The use of intravenous adenosine or the calcium channel blocker verapamil are considered safe and effective therapies for controlling SVTs.
Which emergency drug is used for the immediate management of SVT?
Intravenous adenosine is a safe and efficacious treatment for the emergent treatment of supraventricular tachycardia, including unstable patients (with hypotension and/or chest pain).
What is first-line treatment for PSVT?
Catheter ablation: This outpatient procedure is used to treat or cure many types of heart arrhythmia, including PSVT. Catheter ablation is a mature technique known to be safe and effective. Therefore, it is considered a first-line therapy for PSVT.
What drug is recommended for acute treatment in patients with regular supraventricular tachycardia?
Intravenous diltiazem, verapamil, or metoprolol is recommended for control of heat rate in patients with hemodynamically stable atrial flutter (moderate-quality evidence) and for the treatment of hemodynamically stable focal atrial tachycardia (low-quality evidence).
Is atropine given for SVT?
Atropine is the first-line treatment for symptomatic bradycardia, except for patients with a heart transplant. The first-line treatment for stable patients with supraventricular tachycardia (SVT) is a vagal maneuver. Adenosine is used for narrow complex, regular SVT if vagal maneuvers do not work.
Which of the following is the drug of choice for a patient with stable ventricular tachycardia?
Amiodarone is the drug of choice for acute VT refractory to cardioversion shock. After recovery, oral medications are used for long-term suppression of recurrent VT. Current evidence favors class III antiarrhythmic drugs over class I drugs.
Which drugs is the most preferred for the treatment of PSVT?
At this time, adenosine is the drug of choice of treatment. Verapamil and diltiazem are the most commonly used calcium channel blockers (CCBs). This review aimed to compare the efficacy of both drugs in the treatment of PSVT.
Is digoxin used for SVT?
Medications to Treat Supraventricular Tachycardia (SVT) These medications include: Beta-blocking agents. Calcium channel agents. Digoxin.
Is diltiazem used for SVT?
Diltiazem is given at a dose of 20 mg IV, with another 25-35 mg given if SVT persists. As with adenosine, transient arrhythmias may be seen, although hypotension occurs more commonly in patients receiving calcium channel blockers, especially if SVT persists after administration.
Is Cardizem used to treat SVT?
Pharmacological Use Diltiazem has a COR I, LOE-b classification, used for rate control of atrial arrhythmias, predominantly Atrial Fibrillation, and COR IIa, LOE-b for treatment of SVT with a reentry pathway mechanism.
Which beta-blocker is best for tachycardia?
Arrhythmias: bisoprolol and metoprolol succinate are often preferred. Beta-blockers are the first-line treatment for long-term symptomatic rate control in patients with a range of cardiac arrhythmias, including atrial fibrillation and ventricular tachycardia.
Does amiodarone treat SVT?
Background— Intravenous amiodarone and procainamide are both used as therapies for refractory supraventricular tachycardia (SVT).
Drugs used to treat Supraventricular Tachycardia
The following list of medications are in some way related to, or used in the treatment of this condition.
Further information
Always consult your healthcare provider to ensure the information displayed on this page applies to your personal circumstances.
How to treat SVT?
The Valsalva maneuver Tightly close your mouth, pinch your nose shut, and try to breathe out as hard as you can for 10 to 15 seconds. The Valsalva maneuver is always the first-line treatment for an attack of SVT. Cold water Apply ice water to the face for about five seconds.
What are the symptoms of supraventricular tachycardia?
The most common symptoms of supraventricular tachycardia include: Rapid heart rate. Palpitations. Chest discomfort.
How to treat rapid heartbeat?
An attack of rapid heartbeats is typically treated with physical maneuvers or a self-administered, as needed “pill-in-the-pocket” approach to restore a slower heartbeat. For emergency and unstable situations, an adenosine injection or electrical cardioversion will rapidly restore a normal heartbeat.
What is the vagal maneuver?
Vagal maneuvers. The vagus nerve slows down the two central nerve nodes in the heart. When the vagus nerve is stimulated, then , the heart rate decreases. It goes to work whenever blood pressure rises in the aorta, the main artery leaving the heart.
Is SVT a health problem?
Most people with SVT have structurally normal hearts, and the condition is usually not a health threat. A person with atrial fibrillation often has structural problems with their heart and patients are at increased risk for blood clots, stroke, heart failure, or heart attack.
Does adenosine help with SVT?
When taken as an injection, adenosine slows down the AV node, the primary cause of SVT symptoms. If intravenous adenosine does not work, the next step will be intravenous calcium-channel blockers ( diltiazem or verapamil ), beta-blockers ( esmolol or metoprolol ), or antiarrhythmic medications (procainamide or amiodarone ). All of these drugs slow down the AV node.
Is SVT a tachycardia?
SVT should not be confused with atrial fibrillation or atrial flutter. Technically, both are types of supraventricular tachycardias. SVT is characterized by a fast but regular heartbeat.
What is the best treatment for tachycardia?
The treatment of choice to prevent tachycardia recurrences in WPW patients is catheter ablation , which is successful in over 95% of cases and with a low risk for adverse events depending on AP location. Prophylactic antiarrhythmic drug treatment (propafenone, flecainide, sotalol, amiodarone) is justified when awaiting such an ablation procedure or in patients not accepting the procedure, if the patient is symptomatic with frequent and long lasting episodes. A combination of a class 1C agent (propafenone or flecainide) and a β-blocking agent is the most effective drug regimen. 12 Class I antiarrhythmic drugs and amiodarone prolong the anterograde refractory period of the AP but have minor effect in the retrogradely conducting AP. The data on efficacy of sotalol are limited 13 and no study has yet shown that amiodarone is superior to class Ic antiarrhythmic agents or sotalol. In a prospective study of azimilide, a novel class III agent, the time to recurrence of symptoms related to SVT did not differ significantly from the placebo group, indicating that azimilide did not confer a beneficial effect compared with placebo. 14 β-blocking agents have no effect on APs and their ability to prevent tachycardia recurrences in patients with the WPW syndrome is unknown. Digitalis and calcium channel blocking agents (verapamil, diltiazem) may facilitate the development of VF during AF in patients with WPW syndrome, and should therefore not be used. 15 Long term antiarrhythmic drug treatment is not recommended in WPW patients with high risk profiles (occupations or lifestyles), or in those with severely symptomatic episodes.
Where does supraventricular tachycardia originate?
Supraventricular tachycardia (SVT) is characterised by a rapid impulse formation, that emanates from the sinus node, from atrial tissue (focal or macro-reentrant atrial tachycardia (AT)), from the atrioventricular (AV) no de, or from anomalous muscle fibres that connect the atrium with the ventricle (accessory pathways (APs)).
What medicine can be given to prevent SVT?
For emergent cases, calcium channel or beta blockers can be given through IV (intravenously) for more rapid correction of the heart rhythm. Adenosine is another medicince that can be given through IV as well that can work in a matter of seconds.
How to prevent SVT?
Your healthcare provider might suggest other ways to help prevent SVT, such as the following: 1 Have less alcohol and caffeine 2 Don't smoke 3 Lower your stress 4 Eat foods that are healthy for your heart 5 Don't take recreational drugs, especially stimulants that can over-excite the heart muscle. Some herbs and supplements can have this same effect. Always check with your healthcare team before you take any non-prescribed medicines. 6 Stay well hydrated and get enough sleep
How does a SVT catheter work?
Your healthcare provider puts a thin, flexible tube (catheter) into a blood vessel in the groin. He or she then gently pushes it up into your heart. The area of your heart that causes your SVT is then either cauterized with heat or scarred with freezing energy.
What is the treatment for recurring SVT?
Ongoing treatment of recurring SVT. If you have recurring episodes of SVT, you may need to take medicines, either on an as-needed basis or daily. Medicine treatment may include beta-blockers, calcium channel blockers, or other antiarrhythmic medicines.
How to treat sudden onset SVT?
Your doctor will teach you how to do these safely. These are things such as bearing down or putting an ice-cold wet towel on your face.
How to tell if you have SVT?
SVT is usually treated if: 1 You have symptoms such as dizziness, chest pain, or fainting that are caused by your fast heart rate. 2 Your episodes of fast heart rate are occurring more often or do not return to normal on their own.
How is supraventricular tachycardia treated?
How is supraventricular tachycardia (SVT) treated? Your treatment for SVT depends on a few things. They include what type of SVT, how often you have episodes, and how severe your symptoms are. The goals of treatment are to prevent episodes, relieve symptoms, and prevent problems.
What are the symptoms of SVT?
SVT is usually treated if: You have symptoms such as dizziness, chest pain, or fainting that are caused by your fast heart rate. Your episodes of fast heart rate are occurring more often or do not return to normal on their own.
Drugs used to treat Ventricular Tachycardia
The following list of medications are in some way related to, or used in the treatment of this condition.
Further information
Always consult your healthcare provider to ensure the information displayed on this page applies to your personal circumstances.
What is the long term treatment for SVT?
Long-term pharmacologic therapy for patients with SVT depends on the type of tachyarrhythmia that is occurring and the frequency and duration of episodes, as well as the symptoms and the risks associated with the arrhythmia (eg, heart failure, sudden death). These medications are used to treat or prevent arrhythmia.
What are the best treatments for paroxysmal SVT?
Beta-blockers that are effective in treating paroxysmal SVT include propranolol, esmolol, metoprolol, atenolol, and nadolol. Beta-blockers abolish reentry-induced paroxysmal SVT by increasing the refractory period of the AV node.
What is Class IV calcium channel blocker?
Class IV calcium channel blockers decrease the conduction velocity and prolong the refractory period. Calcium channel blockers prevent calcium influx into the slow channels of the AV node, decrease the conduction velocity, and prolong the refractory period, which effectively terminates reentrant conduction.
Does propafenone help with ventricular arrhythmias?
Propafenone is indicated for the treatment of documented, life-threatening ventricular arrhythmias, such as sustained ventricular tachycardia. It appears to be effective in the treatment of SVTs, including atrial fibrillation and flutter.
Is adenosine effective in AVNRT?
Adenosine is effective in terminating AVNRT and AVRT. More than 90% of patients convert to sinus rhythm with adenosine at 12mg. As a result of its short half-life, adenosine is best administered in an antecubital vein as an intravenous bolus, followed by rapid saline infusion.
Is flecainide safe for ventricular arrhythmias?
In addition, Flecainide is indicated for the prevention of documented, life-threatening ventricular arrhythmias, such as sustained ventricular tachycardia. It is not recommended for less severe ventricular arrhythmias, even if patients are symptomatic. Propafenone (Rythmol) View full drug information.