Can I Bill a nebulizer treatment with 94640 instead of 94664?
Mar 12, 2020 · The code for the nebulizer treatment is, "94640 Pressurized or nonpressurized inhalation treatment for acute airway obstruction for therapeutic purposes and/or for diagnostic purposes such as sputum induction with an aerosol generator, nebulizer, metered dose inhaler or intermittent positive pressure breathing (IPPB) One may also ask, does CPT code 94640 need …
What medications can you use with a nebulizer?
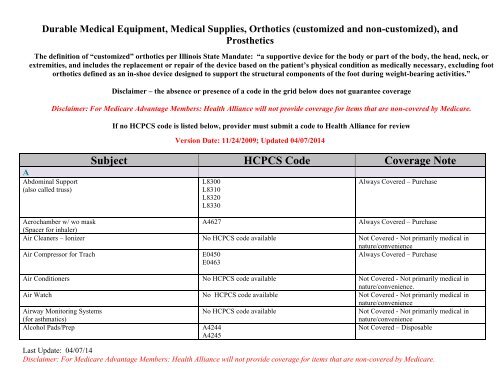
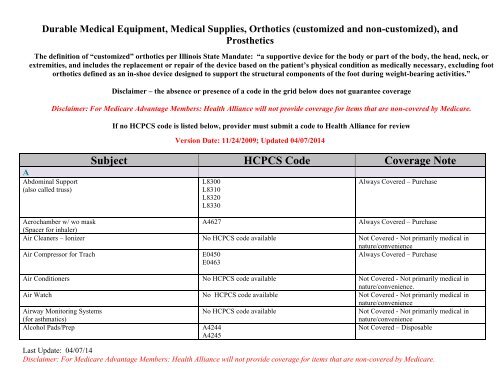
Nov 15, 2017 · Nebulizer cpt code list - A7017, A7018, A7007. For a DME item to be covered by Medicare, it must 1) be eligible for a defined Medicare benefit category, 2) be reasonable and necessary for the diagnosis or treatment of illness or injury or to improve the functioning of a malformed body member, and 3) meet all other applicable Medicare statutory and regulatory …
What are the medical records requirements for a nebulizer with compressor (e0570)?
Oct 02, 2017 · If the patient receives a nebulizer treatment of less than 1 hour (CPT code 94640) during an episode of care and subsequently returns on the same date of service to the urgent care to receive another nebulizer treatment of less than 1e hour, then you would bill CPT code 94640 and append modifier -76, “Repeat procedure or service by same physician or other qualified …
What is the NOC nebulizer drug code for j7699?
Dec 20, 2018 · Can you advise on how to bill an in office nebulizer treatment? I know the correct code is 94640 although some payers are no longer paying for this service. Can 94664 be billed by the office nurse or is this code only to be used by respiratory therapy? Last edited: Mar 20, 2018.
What does "appropriate" mean in medical terms?
Appropriate, including the duration and frequency that is considered appropriate for the service, in terms of whether it is: Furnished in accordance with accepted standards of medical practice for the diagnosis or treatment of the patient’s condition or to improve the function of a malformed body member.
Why do contractors specify bill types?
Contractors may specify Bill Types to help providers identify those Bill Types typically used to report this service . Absence of a Bill Type does not guarantee that the policy does not apply to that Bill Type.
What are reasonable and necessary services?
Contractors shall consider a service to be reasonable and necessary if the contractor determines that the service is: 1 Safe and effective. 2 Not experimental or investigational (exception: routine costs of qualifying clinical trial services with dates of service on or after September 19, 2000, which meet the requirements of the clinical trials NCD are considered reasonable and necessary). 3 Appropriate, including the duration and frequency that is considered appropriate for the service, in terms of whether it is:#N#Furnished in accordance with accepted standards of medical practice for the diagnosis or treatment of the patient’s condition or to improve the function of a malformed body member.#N#Furnished in a setting appropriate to the patient’s medical needs and condition.#N#Ordered and furnished by qualified personnel.#N#One that meets, but does not exceed, the patient’s medical need.#N#At least as beneficial as an existing and available medically appropriate alternative.
What does "furnished" mean?
Furnished in a setting appropriate to the patient’s medical needs and condition. Ordered and furnished by qualified personnel. One that meets, but does not exceed, the patient’s medical need. At least as beneficial as an existing and available medically appropriate alternative.
What is compound inhalation solution?
Compound Inhalation Solution: A product produced by a pharmacy that is not an FDA-approved manufacturer and involves the mixing, combining or altering of ingredients for an individual patient. Compounded drugs are not considered interchangeable with FDA-approved products.
What are the requirements for DME?
For a DME item to be covered by Medicare, it must 1) be eligible for a defined Medicare benefit category, 2) be reasonable and necessary for the diagnosis or treatment of illness or injury or to improve the functioning of a malformed body member, and 3) meet all other applicable Medicare statutory and regulatory requirements. For the items addressed in this local coverage determination, the criteria for "reasonable and necessary", based on Social Security Act §1862(a)(1)(A) provisions, are defined by the following coverage indications, limitations and/or medical necessity.
What is Medicare Advantage Policy Guideline?
The Medicare Advantage Policy Guideline documents are generally used to support UnitedHealthcare Medicare Advantage claims processing activities and facilitate providers’ submission of accurate claims for the specified services. The document can be used as a guide to help determine applicable:
What is the code for chest wall manipulation?
Manipulation of the chest wall is for mobilization of secretions and improvement in lung function. Use code 94667 or 94668 for “hands on” manipulation of the chest wall, per session. CPT code 94669 is used when a mechanical device is used to achieve high-frequency chest wall oscillation (HFCWC), such as a HFCWC device.
What is CPT code 2020?
These are Evaluation and Management CPT codes that are associated with services provided by physicians and other qualified healthcare professionals (NPs and PAs) that can bill Medicare directly. The descriptions and requirements are lengthy and are listed in CPT® Professional 2020, published by the AMA. The term “clinical staff” as used by the AMA refers to professionals who do not bill patients independently such as respiratory therapists and nurses.
Why is standardized coding important?
Standardized coding is essential for Medicare and other health insurance programs to pay claims for medically necessary services in a consistent manner. The Healthcare Common Procedure Coding Set (HCPCS), which is divided into two principal subsystems, is established for this purpose.
What are the two types of outpatient services?
Hospitals provide two distinct types of services to outpatients: services that are diagnostic in nature and services that aid the physician in the treatment of the patient. With a few exceptions, hospital outpatient departments are paid under an outpatient prospective payment system (OPPS), although there are some services that can be paid under a fee schedule. While inpatient services are paid under the IPPS as noted above, outpatient services are bundled into what are called Ambulatory Payment Classification (APC) groups. Services within an APC are similar clinically and with respect to hospital resource use. Each HCPCS Code that can be paid separately under OPPS is assigned to an APC group. The payment rate and coinsurance amount calculated for an APC apply to all services assigned to the APC.
How often can you use the PEP code?
The following code is appropriate for demonstration and/or evaluation of inhaler techniques and includes demonstration of flow-operated inhaled devices such as Positive and Oscillating Expiratory Pressure (PEP/OPEP) devices. The code may only be used once per day. For example, it cannot be billed at the same time/same visit as 94640. The code should not be reported for patients who
What is incident to respiratory therapy?
In a physician office or clinic setting, respiratory therapy services are furnished “incident to” the care provided and ordered by a physician (or placed in an approved protocol). The physician bills Medicare directly as appropriate, not the RT. To be covered, “incident to” services must be: 1) commonly furnished in a physician’s office or clinic (not an institutional setting); 2) an integral part of the patient’s treatment course; 3) commonly rendered without charge or included in the physician’s bill; and, 4) furnished under the supervision of a physician or other qualified health care professional.
Does Medicare cover pulmonary rehabilitation?
Medicare covers pulmonary rehabilitation (PR) programs (i.e., those consisting of components set forth in law ) for patients who have been diagnosed with moderate, severe, or very severe COPD as established by the GOLD guidelines, stages II-IV. No more than two one-hour sessions may be billed in a single day and the services are only covered if provided in a physician’s office or hospital
What is a nebulizer?
Summary. A nebulizer is a piece of medical equipment that can help deliver medication directly to the lungs and the respiratory system where it is needed. While the device is simple to operate, it is essential to use, clean, and maintain it correctly.
How to use a nebulizer?
In general, a nebulizer is very easy to use, with only a few basic steps: 1 Wash the hands. 2 Add the medicine to the medicine cup, according to the doctor’s prescription. 3 Assemble the top piece, tubing, mask, and mouthpiece. 4 Attach the tubing to the machine, according to the instructions. 5 Turn the nebulizer on; they can be battery- or electrically powered. 6 While using the nebulizer, hold the mouthpiece and medicine cup upright to help deliver all the medication. 7 Take slow, deep breaths through the mouthpiece and inhale all the medicine.
What conditions require a nebulizer?
Doctors typically prescribe nebulizers to people with one of the following lung disorders: asthma. chronic obstructive pulmonary disease (COPD) cystic fibrosis. bronchiectasis.
How does a nebulizer work?
A nebulizer turns liquid medicine into a very fine mist that a person can inhale through a face mask or mouthpiece. Taking medicine this way allows it to go straight into the lungs and the respiratory system where it is needed.
How long does it take for a nebulizer to work?
Nebulizers tend to be a little easier to use, in terms of delivering the medicine. However, a nebulizer may take up to 10 minutes to dispense the medication, and the user needs to sit still until they have inhaled all of it, which may be hard for a young child.
What is the difference between a nebulizer and an inhaler?
Nebulizers and inhalers have some similarities — for example, they both deliver medicine directly into the lungs to help make breathing easier. However, there are some important differences. There are two types of inhalers: a metered-dose inhaler (MDI) and a dry-powder inhaler. An MDI is the most common type of inhaler.
How does a dry powder inhaler work?
A dry-powder inhaler is similar, but the medication is in powder form inside the inhaler. It requires the user to take a deep, fast breath, which pulls the powdered medicine deep into the lungs. Both types require the ability to inhale the medicine deep within the lungs.
