Monoclonal antibodies are administered either subcutaneously or as an intravenous infusion. The FDA strongly recommends IV infusion except for when IV infusion is not available or would lead to a delay in treatment.
What are the dangers of monoclonal antibodies?
administer monoclonal antibodies to patients if they have experienced the onset of mild to moderate symptoms of COVID-19 in the last 10 days, have tested positive for COVID-19, and have one or more of the following high-risk factors.1 ☐ Develop a process to gain patient consent for treatment as indicated by local and state requirements.
When to administer monoclonal antibodies?
Jan 25, 2022 · Neutralizing antiviral monoclonal antibodies have been used clinically against Ebola virus disease (EVD), e.g., ZMapp, and respiratory syncytial virus (RSV) e.g.palivizumab. Due to that, monoclonal antibodies have been explored as an option against SARS-CoV-2. Neutralizing antibodies can directly neutralize the virus without the aid of other immune factors or cells.
Are there side effects of monoclonal antibody treatment?
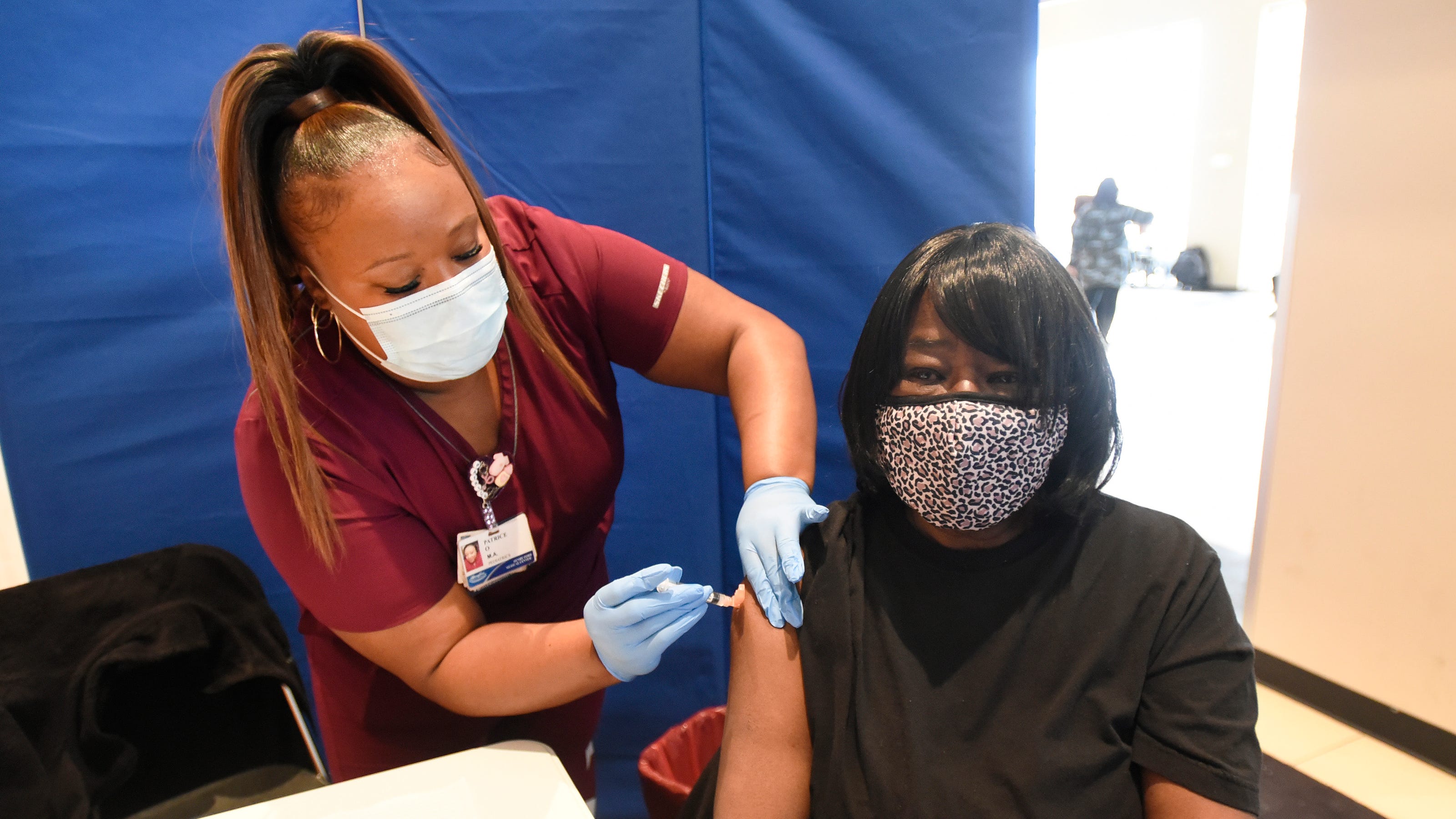
Jan 06, 2022 · “Monoclonal antibodies are laboratory-made proteins that mimic the body’s immune system to fight off COVID-19 infection,” Spivak says. These antibodies are given to people directly through an intravenous (IV) infusion. How does monoclonal antibody therapy help?
How effective is the monoclonal treatment?
Treatment with COVID-19 monoclonal antibodies is done through a one-time intravenous (IV) infusion. Another option for COVID-19 therapy is an antiviral called Remdesivir. Remdesivir is approved by the FDA and helps reduce the effects of COVID-19.
What is the function of antibodies?
Antibodies are proteins that exist in our bodies as part of our immune system to recognize and defend against harmful viruses and bacteria. Monoclonal antibodies are made in a laboratory and designed to target a specific virus or bacteria.
Does infusion cause nausea?
Some people may experience infusion-related side effects, such as nausea and dizziness, that are short-lived and go away on their own. As with any medication, there is the potential for mild or more severe allergic reactions, which are uncommon.
What is the purpose of monoclonal antibodies?
Monoclonal antibodies targeting the S protein have the potential to prevent SARS-CoV-2 infection and to alleviate symptoms and limit progression to severe disease in patients with mild to moderate COVID-19, particularly in those who have not yet developed an endogenous antibody response. 3.
What antibody targets the RBD of the S protein?
Bamlanivimab (also known as LY-CoV555 and LY3819253) is a neutralizing monoclonal antibody that targets the RBD of the S protein of SARS-CoV-2. Etesevimab (also known as LY-CoV016 and LY3832479) is another neutralizing monoclonal antibody that binds to a different but overlapping epitope in the RBD of the SARS-CoV-2 S protein. Casirivimab (previously REGN10933) and imdevimab (previously REGN10987) are recombinant human monoclonal antibodies that bind to nonoverlapping epitopes of the S protein RBD of SARS-CoV-2.
What are the adverse events of bamlanivimab?
In the Phase 2 Blocking Viral Attachment and Cell Entry with SARS-CoV-2 Neutralizing Antibodies (BLAZE-1) trial, the most common adverse events associated with bamlanivimab were nausea, diarrhea, dizziness, headache, pruritis, and vomiting. The safety profile of bamlanivimab at all three doses was reportedly like that of the placebo.
What is Casirivimab plus imdevimab?
Casirivimab plus imdevimab: These are recombinant human monoclonal antibodies that bind to nonoverlapping epitopes of the spike protein RBD of SARS-CoV-2. Sotrovimab: This monoclonal antibody was originally identified in 2003 from a SARS-CoV survivor.