Can patients make their own medical decisions?
See other articles in PMC that citethe published article. Many patients cannot make their own medical decisions, having lost what is called decisional capacity.
Who can make medical decisions in a family law case?
These laws generally provide a hierarchy of authorized family decision-makers who in descending order starting with the spouse can make medical treatment decisions on someone’s behalf.
Should physicians tell the truth to patients'families?
The family may know the truth, but they protect the patient by preserving hope and keeping the truth from the patient; this protection is the family's duty. In fact, subjects in this study thought physicians should check with the family prior to telling a patient the truth about a diagnosis or prognosis.
What do hospitalists think about the decision-making process?
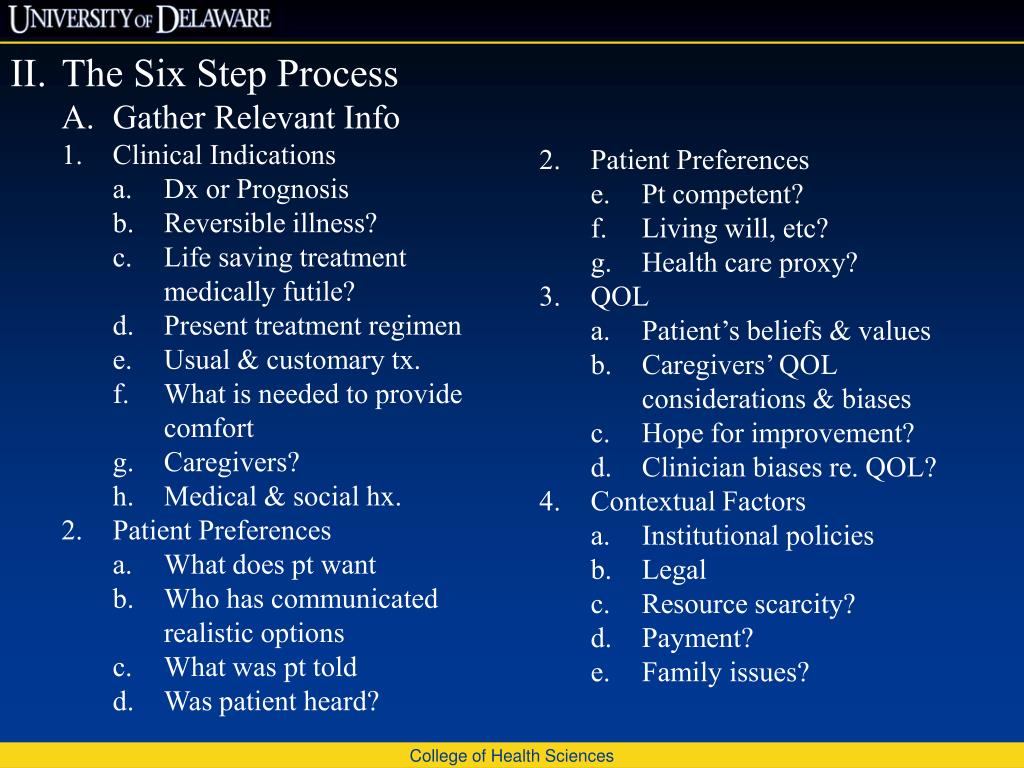
Perhaps most interesting was the perspective of the hospitalists on the decision-making process. During the focus group, many stated that the process to identify the patient’s values and preferences was more important than the legal identification of the proper decision-maker.
Which group is most commonly prohibited from serving as alternate decision makers?
How many states have default surrogate decisions?
About this website
Who decides medical treatment?
In California, the part of an advance directive you can use to appoint an agent to make healthcare decisions is called a Power of Attorney For Health Care. The part where you can express what you want done is called an Individual Health Care Instruction.
Who has the right to make health care decisions for patients?
The law recognizes that adults—in most states, people age 18 and older—have the right to manage their own affairs and conduct personal business, including the right to make health care decisions.
Who makes decisions in a hospital?
Decision-makers, occasionally known as “budget-holders,” are executives of hospitals and IDNs and may hold titles such as CEO, CFO, or COO. Who qualifies as a decision-maker depends on the product and goal of the company selling into that care facility.
How do doctors decide which treatment?
Physicians would choose to treat when the probability of disease is above the threshold probability and would choose to withhold treatment otherwise[1, 2]. The threshold model stipulates that as the therapeutic benefit/harms ratio increases, the threshold probability at which treatment is justified is lowered.
Do patients have the right to choose their treatment?
A patient's right to choose or refuse treatment is limited by the physician's right (and duty) to practice medicine responsibly. Bizarre or destructive choices made by a patient are not sacrosanct simply because the patient made them.
Who determines if a patient is competent?
Competence is determined by a judge [1][2][3]. This legal determination is never determined by medical providers.
Who decides medical decisions if you are incapacitated?
If you become incapacitated and do not make your own medical decisions through an advance directive like a living will or medical power of attorney, then the court may appoint a legal guardian to make any necessary medical decisions for you.
Who makes medical decisions if there is no next of kin?
The general term for such person is surrogate decision maker. If there is no health care power of attorney document in place and no court-appointed guardian with authority to make health care decisions, most states provide for a default surrogate decision maker in their state laws.
Who makes medical decisions if there is no advance directive?
Unrepresented patients are those who have no surrogate or advance directive to guide medical decision making for them when they become incapacitated.
Can a doctor decide for a patient?
When deciding whether a patient can make medical decisions, the doctor must evaluate whether the patient can understand these things: the nature of his illness. the nature and purpose of the treatment. the advantages and risks of the treatment.
Can doctors make decisions for patients?
When a patient lacks decision-making capacity, the physician has an ethical responsibility to: Identify an appropriate surrogate to make decisions on the patient's behalf: The person the patient designated as surrogate through a durable power of attorney for health care or other mechanism.
How are clinical decisions made?
Clinical decision making is a balance of experience, awareness, knowledge and information gathering, using appropriate assessment tools, your colleagues and evidence-based practice to guide you. Good decisions = safe care. Good, effective clinical decision making requires a combination of experience and skills.
Who Makes Medical Decisions if You’re Incapacitated?
A living will. A living will is an instrument that states your preferences for a variety of possible treatments or procedures that physicians may have to perform, depending on your medical circumstances.. Usually, these are things that physicians only have to decide in an emergency, most often when you are unconscious or incapacitated.
Adults Who Can't Make Medical Decisions on Their Own
Adults can usually make medical decisions (consent to treatment) on their own. But they may need someone to make medical decisions for them if their decision-making ability is affected by an illness or disability. This is called substituted consent. Deciding Whether Someone Can Make Medical Decisions When suggesting treatment, medical professionals must evaluate whether their patients are able ...
If There is No Advance Directive or Guardian, Who Makes Medical ...
Because questions about surrogate decisions are so grave and the existing knowledge so scant, in the Spring of 2015, the ABA Commission on Law and Aging conducted a focus group of physicians at the March meeting of the Society of Hospital Medicine. The group included 22 hospitalists from 13 states, with a medical experience range of from five to 32 years. While small and not conclusive for ...
Who has the legal right to make decisions about your funeral? - Funeral ...
Personal Preference Laws for Body Disposition In more than half the states, there is a statutory obligation for survivors to honor the written wishes of the deceased, to follow your personal preference. In a few states, your wishes may be over-turned in the case of cremation, however. Even if there is no personal preference law... Read More >
My legal next of kin | Novant Health | Choices and Champions
Recognizing your legal decision makers. If you do not have a healthcare agent or guardian, and you are not able to make your own medical decisions, the law specifies who is given the legal right to make decisions for you.
Which group is most commonly prohibited from serving as alternate decision makers?
The group most commonly prohibited from serving as alternate decision makers is health care providers , with 35 states limiting or prohibiting their service in this role. Of the 51 jurisdictions, 41 have a provision allowing for appointment of a default surrogate for medical decision making in the absence of an agent (Fig. 1).
How many states have default surrogate decisions?
Four states are silent on the topic of default-surrogate decision making. In the 35 states that establish a surrogate hierarchy, the highest-priority classes always include spouse, child, and parent, though 8 states also insert partner or “chosen adult” on or immediately below the first ladder rung (Fig. 1).
What is the responsibility of a medical caregiver?
The next responsibility of the medical caregiver is to anticipate and negotiate cultural differences. In the United States, medical, legal, and ethical practices hold patient autonomy in the highest regard. The principle of patient autonomy asserts the rights of individuals to make informed decisions about their medical care. Thus, patients should be told the truth regarding their diagnosis and prognosis, as well as the risks and benefits of proposed treatments, and should be allowed to make choices based on this information. The standard of care in this country is to tell patients the truth about even fatal illnesses and to obtain their informed consent for major procedures [3].
What did Mrs. Odundo's husband say about surgery?
Odundo's husband repeated the statement—on many occasions, to many doctors —that his wife would want to exhaust all treatment options, including surgery, even if there were only a minimal chance for improvement or cure.
Does HIPAA require an interpreter?
HIPAA further mandates that the patient's permission for an ad hoc interpreter must be documented in the record. University of California, San Diego's Medical Center policy is that only professional interpreters may participate in end-of-life-discussions.
Should physicians check with family members before telling a patient the truth?
In fact, subjects in this study thought physicians should check with the family prior to telling a patient the truth about a diagnosis or prognosis. Paradoxically, it's possible that, in these cultures, patients maintain their autonomy by deferring to a family member.
Did Dr Martinez arrange for an interpreter?
In the case above, Dr. Martinez did well to arrange for the interpreter to meet with the entire family. Given the contradictory reports from the patient's family about what Mrs. Odundo's wishes truly are, it is necessary to discuss the possible complications of the procedure since her husband or children may have omitted this. It would also be important to preserve hope (since this is a goal of medicine in any culture) and to emphasize that the medical team will continue to work in her behalf if she chooses not to have surgery.
Does having an interpreter guarantee understanding?
That said, having an interpreter does not guarantee understanding and clear communication—quite the contrary. Numerous studies have reported the high number of errors made in translation, including omissions, additions, editorializations, and false fluency [2].
Is it impractical to have a medical interpreter?
It is impractical to expect to have a professional medical interpreter for every patient encounter. The service is time consuming—not only waiting for interpreters to arrive in person or be reached by phone—but the actual process of interpreting is laborious and lengthy.
When making any treatment decision, should you consider the risks, benefits, and supporting evidence for the treatment?
In addition, you should consider if the treatment is compatible with your personal values and preferences and if it is accessible at a reasonable cost.
What is the foundation for informed medical decision making?
The Foundation for Informed Medical Decision Making is an organization that offers DVD and VHS-based decision support tools, which can be ordered from their website.
What is decision support tool?
A decision support tool will take into account both the quantitative and qualitative benefits of each outcome: it will consider the fact that a mastectomy will greatly lower the changes of getting breast cancer, but also how surgery might affect your self-esteem and feelings about your body.
Is treatment decision emotional?
Making a treatment decision can be complex and emotional. Luckily there are tools to help you weigh all the factors that apply in your individual situation. Some of these can be found online.
Is it important to consider the risks, benefits, and evidence together?
It is often helpful to consider the risks, benefits, and evidence together. For example, you may decide to pursue a course of treatment even if there is only a moderate amount of research for it but the potential benefits are high and the known risks are low. On the other hand, if the risk of a treatment is high and the benefit ...
Who decides whether a patient's treatment is necessary?
Regardless of what an individual doctor decides about a patient’s health and appropriate course of treatment, the medical group is given authority to decide whether a patient’s treatment is actually necessary. But the medical group is beholden to its relationship with the insurance company.
What is a medical group contract?
The medical group contracts with the insurance company to provide services to insured parties in exchange for coverage. These contracts often require the medical group to make its own determinations about a patient’s treatment.
What happens when a health insurance provider rejects a claim in bad faith?
When a health insurance provider rejects a claim in bad faith, policyholders have the right to sue. When a procedure or course of treatment has been recommended by a treating physician, a health insurance provider should not be able to unilaterally claim a lack of medical necessity in contravention of the medical evidence.
What is a medical group?
The medical group is an entity separate from the actual practicing physicians within the group. In order to insulate themselves from unilaterally deciding whether a treatment is medically necessary, the insurance companies often rely on the decisions of the medical group. This system is flawed. Regardless of what an individual doctor decides about ...
Can a doctor deny a referral to a specialist?
In many cases, however, a treating physician will recommend a procedure or referral to a specialist for a serious health condition, but their recommended treatment will be denied by the patient’s insurance provider.
Is a procedure not medically necessary?
If the insurance company, by itself or with the blessing of a complicit medical group, claims a procedure is not medically necessary in contravention of the actual medical needs of the patient, the patient’s finances, health, and life are at stake.
What percentage of people are not mentally able to make their own decisions about their care?
Most people nearing the end of life are not physically, mentally, or cognitively able to make their own decisions about care. Approximately 40 percent of adult medical inpatients, 44-69 percent of nursing home residents, and 70 percent of older adults facing treatment decisions are incapable of making those decisions themselves.1. ...
What is hospital medicine?
Hospital medicine is an emergent medical specialty dedicated to the delivery of comprehensive medical care to hospitalized patients. Hospitalists are on the front line every day. They work under pressure—sometimes with incomplete records or delayed records, and little or no knowledge of a patient’s background.
How many Americans have an advance directive?
Because less than 30% of Americans have an advance directive in place, 3 these surrogate consent laws cover the vast majority of decisions for patients unable to give informed consent. Indeed, “default surrogates are the most numerous type of surrogate.
What to do if your treatment center does not give you a treatment plan?
Even if your treatment center does not use treatment plans or does not give you one, you can ask for as much information in writing as possible. This will help you remember what's been told to you, which can be hard to do when you're given a lot of information at once. Either way, having things in writing is helpful.
What is treatment planning?
Treatment planning involves figuring out the exact doses of the treatment that will be given and how long it will last.
What to do if you don't get a treatment plan?
If you don't get a written treatment plan, you can ask for a treatment schedule to be written out for you. A treatment schedule includes: The type of treatment that will be given, such as radiation therapy, chemotherapy, targeted therapy, immunotherapy, hormone therapy, etc.
How is cancer treatment planned and scheduled?
How Treatment Is Planned and Scheduled. To plan and schedule cancer care and treatments, a lot of information must first be collected. This information often needs to be shared with different specialists , as well as with patients and their caregivers, to help decide what treatment option is best. Once a treatment is decided on, care can be ...
What tests are done to determine the stage of cancer?
Your exact cancer diagnosis and stage. Special test results, such as imaging (x-rays), blood tests, tumor marker tests, genetic testing, or biomarker tests done on the tumor. Your planned treatment, its doses, the schedule for getting it, and how long it is expected to be given.
Why do we need a cancer treatment plan?
A cancer treatment plan is kind of like a roadmap because it helps to lay out the expected path of treatment. It is a document that is created by the cancer care team and given to the patient and others that may need to know the planned course of care.
Can you take a break from cancer treatment?
Sometimes taking a break is recommended by the cancer care team, and that's OK. It might be due to side effects, to do more tests, because of a holiday or special event, or because of other health problems. But some patients who are actively on treatment might wonder if they can take a break for personal reasons.
Which group is most commonly prohibited from serving as alternate decision makers?
The group most commonly prohibited from serving as alternate decision makers is health care providers , with 35 states limiting or prohibiting their service in this role. Of the 51 jurisdictions, 41 have a provision allowing for appointment of a default surrogate for medical decision making in the absence of an agent (Fig. 1).
How many states have default surrogate decisions?
Four states are silent on the topic of default-surrogate decision making. In the 35 states that establish a surrogate hierarchy, the highest-priority classes always include spouse, child, and parent, though 8 states also insert partner or “chosen adult” on or immediately below the first ladder rung (Fig. 1).

Case
Commentary
- American physicians are providing more and more care to patients from different ethnic and cultural backgrounds who frequently speak languages other than English. According to the 2000 U.S. Census , 65 percent of the population was white, and the remaining ethnic groups were black (13 percent), Hispanic (13 percent), Asian-Pacific Islander (4.5 percent; the great majority of wh…
Language Barriers
- The first and most obvious problem is the language barrier. In this case, the patient speaks an East African dialect for which there are no translators available at the hospital. Her husband provided a history. This scenario is common even when the patient is Spanish-speaking and professional interpreter services are available. Very often, due to convenience and timeliness, fa…
Cultural Barriers and Differences
- The next responsibility of the medical caregiver is to anticipate and negotiate cultural differences. In the United States, medical, legal, and ethical practices hold patient autonomy in the highest regard. The principle of patient autonomy asserts the rights of individuals to make informed decisions about their medical care. Thus, patients should ...
The Case at Hand
- In the case above, Dr. Martinez did well to arrange for the interpreter to meet with the entire family. Given the contradictory reports from the patient's family about what Mrs. Odundo's wishes truly are, it is necessary to discuss the possible complications of the procedure since her husband or children may have omitted this. It would also be important to preserve hope (since this is a go…