
Medication
Penicillin and amoxicillin are the antibiotics of choice for the treatment of pharyngitis. The association of amoxicillin and clavulanate is not indicated as the initial treatment of acute infection. Neither are macrolides indicated as first-line therapy; they should be reserved for patients allergic to penicillin.
Self-care
However there may be historical, cultural or anecdotal evidence linking their use to the treatment of Tonsillitis/Pharyngitis. For ratings, users were asked how effective they found the medicine while considering positive/adverse effects and ease of use (1 = not effective, 10 = most effective).
Nutrition
Shvartzman P, Tabenkin H, Rosentzwaig A, Dolginov F. Treatment of streptococcal pharyngitis with amoxycillin once a day. BMJ. 1993 May 1. 306 (6886):1170-2. [Medline]. [Full Text].
Which antibiotics are used in the treatment of pharyngitis?
An inflammation of the pharynx which frequently results in a sore throat and may be caused by a variety of microorganisms. The following list of medications are in some way related to, or used in the treatment of this condition. Activity ?
Is there any evidence to support the treatment of tonsillitis/pharyngitis?
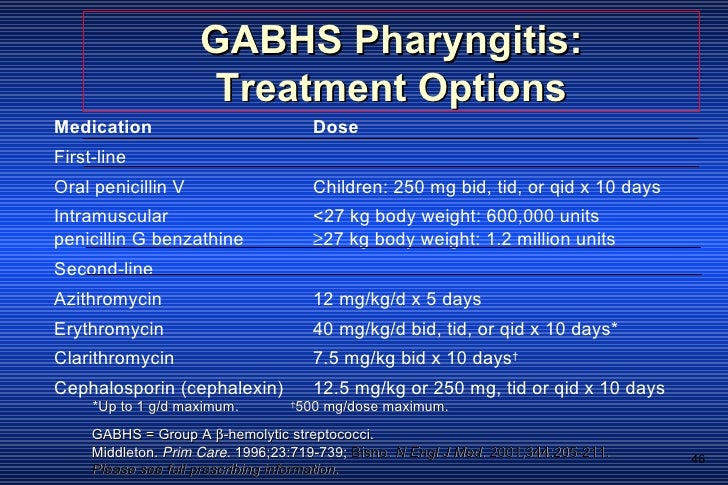
What are the treatment options for streptococcal pharyngitis (strep throat)?
What is pharyngitis?
What is the best antibiotic for pharyngitis?
Penicillin or amoxicillin is the antibiotic of choice to treat group A strep pharyngitis. There has never been a report of a clinical isolate of group A strep that is resistant to penicillin. However, resistance to azithromycin and clarithromycin is common in some communities.
How is bacterial pharyngitis treated?
Bacterial pharyngitis should be treated with appropriate antibiotics once the infection has been confirmed. The symptoms for any pharyngitis should be additionally treated with nonsteroidal anti-inflammatory drugs or acetaminophen for antipyresis and analgesia.
What medicine helps pharyngitis?
Acetaminophen or NSAIDs (nonsteroidal anti-inflammatory drugs) like ibuprofen and naproxen can take the edge off many cold symptoms, including your sore throat.
Why is penicillin used for pharyngitis?
Penicillin has been the drug of choice for the treatment of group A β haemolytic streptococci pharyngitis for more than four decades because it accelerates the resolution of symptoms and reduces the number of suppurative complications.
Can azithromycin treat pharyngitis?
Azithromycin is a type of macrolide antibiotic and used for the treatment of varieties of bacterial infections, including pharyngitis and tonsillitis.
Is azithromycin good for strep throat?
Z-Pack is a form of the brand-name drug Zithromax, which contains the antibiotic azithromycin. Azithromycin is an antibiotic that can treat strep throat, though it's not a common choice for this infection.
Is azithromycin an antibiotic?
Azithromycin: antibiotic to treat bacterial infections - NHS.
Is pharyngitis viral or bacterial?
Pharyngitis is most commonly caused by viral infections such as the common cold, influenza, or mononucleosis. Viral infections don't respond to antibiotics, and treatment is only necessary to help relieve symptoms. Less commonly, pharyngitis is caused by a bacterial infection.
What is amoxicillin used for?
Amoxicillin is a penicillin antibiotic. It is used to treat bacterial infections, such as chest infections (including pneumonia) and dental abscesses. It can also be used together with other antibiotics and medicines to treat stomach ulcers.
What is flagyl used for?
Metronidazole is an antibiotic that is used to treat a wide variety of infections. It works by stopping the growth of certain bacteria and parasites. This antibiotic treats only certain bacterial and parasitic infections. It will not work for viral infections (such as common cold, flu).
What is ciprofloxacin used for?
About ciprofloxacin It belongs to a group of antibiotics called fluoroquinolones. It is used to treat serious infections, or infections when other anitbiotics have not worked. It's used to treat bacterial infections, such as: chest infections (including pneumonia)
What is clindamycin used for?
Clindamycin is used to treat bacterial infections. This medicine may be given to patients who have had an allergic reaction to penicillin. Clindamycin will not work for colds, flu, or other virus infections. This medicine is available only with your doctor's prescription.
What is Gabhs in vitro?
GABHS remains uniformly susceptible in vitro. Interferes with synthesis of cell wall mucopeptides by binding to penicillin-binding proteins. Often used in place of oral penicillin VK in young children. Efficacy equal to penicillin, and often chosen because of the unpalatability of the penicillin susp.
What class of antibiotics is cleocin?
Sporadic resistance has been reported. Clindamycin (Cleocin) Belongs to the lincosamide class of antibiotics. Binds to the 50s ribosome and prevents bacterial protein synthesis. Is an option for symptomatic patients with multiple, recurrent episodes of pharyngitis proven by culture or rapid antigen testing.
What is the drug that interferes with cell wall synthesis?
Interferes with synthesis of cell wall by binding to penicillin -binding proteins. Penicillin is the drug of choice to treat GABHS pharyngitis, as recommended by expert committees of the American Heart Association, American Academy of Pediatrics, and the Infectious Disease Society of America, because of proven efficacy, safety, narrow spectrum, ...
What is the goal of pharmacotherapy?
The goals of pharmacotherapy are to eradicate the infection, to reduce morbidity, and to prevent complications. Next: Antibiotics. Antibiotics. Class Summary. Oral penicillin is currently the drug of choice for GABHS pharyngitis. [ 1] .
Is amoxicillin safe for pharyngitis?
Tetracyclines and trimethoprim/sulfamethoxazole should not be used to treat GABHS pharyngitis owing to higher rates of resistance.
Which antibiotic binds to the P site of the 50S ribosomal subunit of susceptible organisms?
Semisynthetic macrolide antibiotic that reversibly binds to P site of 50S ribosomal subunit of susceptible organisms and may inhibit RNA-dependent protein synthesis by stimulating dissociation of peptidyl t-RNA from ribosomes, causing bacterial growth inhibition.
Is cephalosporin a bactericidal agent?
Bactericidal activity against rapidly growing organisms. Oral cephalosporins are highly effective for streptococcal pharyngitis, and several studies have found them to have slightly higher eradication rates than those of penicillin. Second-line agents in the treatment of patients with GABHS pharyngitis.
What antibiotics are used for pharyngitis?
The ACP, American Academy of Pediatrics (AAP), and Infectious Diseases Society of America (IDSA) all agree that the antibiotics of choice for acute pharyngitis are oral penicillin V (for 10 days), intramuscular penicillin G benzathine (single dose), and oral amoxicillin (10 days), which is as efficacious as penicillin but more palatable, especially in children. [ 48]
What is the best antibiotic for pharyngitis?
Oral penicillin V remains the preferred antibiotic to treat GABHS pharyngitis. [ 1] . Amoxicillin is often prescribed and is an acceptable first-line agent because of its narrow spectrum, the ease of once-daily dosing, and improved palatability, especially for children.
What kind of doctor can treat pharyngitis?
In these cases, a drainage procedure performed by an interventional radiologist or otolaryngologist should be considered.
How long after antibiotics can you go to school?
Patients with bacterial pharyngitis should be kept out of daycare, school, or work until 24 hours after the initiation of antibiotics.
What macrolides are used in penicillin?
In patients with history of severe or anaphylactic reactions to penicillin, macrolides such as azithromycin, clarithromycin, and erythromycin may be used, although resistance has been reported in the United States [ 64] and internationally. [ 65] .
Can pharyngitis be recurrence?
Recurrence: Test of cure is not indicated when pharyngitis symptoms have resolved following treatment. In patients with recurrent symptoms, retreatment with an initial first-line agent (oral penicillin, benzathine penicillin, or a first-generation cephalosporin) is reasonable. Worth noting is the difficulty in differentiating between viral pharyngitis with GABHS carriage and actual GABHS pharyngitis. This becomes even more of an issue in patients with multiple recurrences. Between 5% and 15% of children are asymptomatic carriers during seasons when GABHS pharyngitis is most prevalent. [ 67] A positive test result during a time of wellness may indicate GABHS carriage. When multiple recurrences are believed to be due to GABHS infection, clindamycin or amoxicillin/clavulanic acid is indicated. [ 1] A 2018 systematic review supports this recommendation because of the superiority of the two drugs to penicillin in terms of eradicating streptococci and nonstreptococci. However, the level of evidence was deemed of moderate quality owing to the risk of bias from two included randomized controlled trials. [ 68]
What is delayed antibiotic prescription?
When a patient presents with signs and symptoms that cannot be initially confirmed as viral or bacterial by a healthcare provider , one strategy is to provide a delayed antibiotic prescription. The delayed prescription can be filled by the patient "just in case" the sore throat does not follow the course of viral pharyngitis, instead progressing as bacterial pharyngitis. Symptom control was similar between immediate and delayed antibiotic prescription, with the latter having the potential to decrease antibiotic usage. [ 70]
How does group A strep pharyngitis work?
Shortens the duration of symptoms. Reduces the likelihood of transmission to family members, classmates, and other close contacts. Prevents the development of complications, including acute rheumatic fever. When left untreated, the symptoms of group A strep pharyngitis are usually self-limited.
How old do you have to be to get antibiotics for strep pharyngitis?
Clinicians should confirm group A strep pharyngitis in children older than 3 years of age to appropriately guide treatment decisions. Giving antibiotics to children with confirmed group A strep pharyngitis can reduce their risk of developing sequela (acute rheumatic fever). Testing for group A strep pharyngitis is not routinely indicated for:
How long does it take for strep pharyngitis to develop?
The incubation period of group A strep pharyngitis is approximately 2 to 5 days.
How is strep pharyngitis transmitted?
Typically transmission occurs through saliva or nasal secretions from an infected person. People with group A strep pharyngitis are much more likely to transmit the bacteria to others than asymptomatic pharyngeal carriers.
What is the name of the virus that causes pharyngitis?
Many viruses and bacteria can cause acute pharyngitis. Streptococcus pyogenes, which are also called group A Streptococcus or group A strep, cause acute pharyngitis known as strep throat.
What is the name of the rash caused by group A strep?
Anterior cervical lymphadenopathy. Patients with group A strep pharyngitis may also present with a scarlatiniform rash. The resulting syndrome is called scarlet fever or scarlatina. Respiratory disease caused by group A strep infection in children younger than 3 years old rarely manifests as acute pharyngitis.
What is the most common cause of pharyngitis in all age groups?
The differential diagnosis of acute pharyngitis includes multiple viral and bacterial pathogens. Viruses are the most common cause of pharyngitis in all age groups. Experts estimate that group A strep, the most common bacterial cause, causes 20% to 30% of pharyngitis episodes in children. In comparison, experts estimate it causes approximately 5% to 15% of pharyngitis infections in adults.
What is the first generation of cephalosporin?
First-generation cephalosporin that arrests bacterial growth by inhibiting bacterial cell wall synthesis. Bactericidal activity against rapidly growing organisms. Oral cephalosporins are highly effective for streptococcal pharyngitis, and several studies have found them to have slightly higher eradication rates than those of penicillin. Second-line agents in the treatment of patients with GABHS pharyngitis.
What is the treatment for pharyngitis?
Treatment of choice for GAS pharyngitis, as recommended by expert committees of the American Heart Association, American Academy of Pediatrics, and the Infectious Disease Society of America, because of its proven efficacy, safety, narrow spectrum, and low cost. Inhibits biosynthesis of cell wall by binding to penicillin-binding proteins. Bactericidal against sensitive organisms when adequate concentrations are reached and most effective during stage of active multiplication. Inadequate concentrations may be ineffective. GABHS remains uniformly susceptible in vitro.
Which antibiotic binds to the P site of the 50S ribosomal subunit of susceptible organisms?
Semisynthetic macrolide antibiotic that reversibly binds to P site of 50S ribosomal subunit of susceptible organisms and may inhibit RNA-dependent protein synthesis by stimulating dissociation of peptidyl t-RNA from ribosomes, causing bacterial growth inhibition.
Does penicillin interfere with cell wall synthesis?
Interferes with synthesis of cell wall by binding to penicillin-binding proteins. Penicillin is the drug of choice to treat GABHS pharyngitis, as recommended by expert committees of the American Heart Association, American Academy of Pediatrics, and the Infectious Disease Society of America, because of proven efficacy, safety, narrow spectrum, and low cost. Preferred for patients unlikely to complete a full 10-d PO course. S pyogenes remains universally sensitive to penicillin.
What is a blister that affects the pharynx?
Gingivostomatitis, blisters and ulcers which affect the pharynx and the oral cavity. Can include pharyngeal exudate
What is the most common infectious disease in adults?
Acute pharyngitis in adults is one of the most common infectious diseases seen in general practitioners’ consultations. Viral aetiology is the most common. Among bacterial causes, the main agent is Streptococcus pyogenesor group A β-haemolytic streptococcus (GABHS), which causes 5%–30% of the episodes. In the diagnostic process, clinical assessment scales can help clinicians to better predict suspected bacterial aetiology by selecting patients who should undergo a rapid antigen detection test. If these techniques are not performed, an overdiagnosis of streptococcal pharyngitis often occurs, resulting in unnecessary prescriptions of antibiotics, most of which are broad spectrum. Consequently, management algorithms that include the use of predictive clinical rules and rapid tests have been set up. The aim of the treatment is speeding up symptom resolution, reducing the contagious time span and preventing local suppurative and non-suppurative complications. Penicillin and amoxicillin are the antibiotics of choice for the treatment of pharyngitis. The association of amoxicillin and clavulanate is not indicated as the initial treatment of acute infection. Neither are macrolides indicated as first-line therapy; they should be reserved for patients allergic to penicillin. The appropriate diagnosis of bacterial pharyngitis and proper use of antibiotics based on the scientific evidence available are crucial. Using management algorithms can be helpful in identifying and screening the cases that do not require antibiotic therapy.
When do most infections occur?
In terms of presentation, the highest incidence of all infections is usually in winter and spring. There are some exceptions, such as those caused by rhinoviruses or other viruses which cause upper respiratory tract infections, common at the end of spring or even at the beginning of summer, such as those caused by the adenovirus group.
Is AP resistant to penicillin?
To date, the streptococci which cause AP remain sensitive to penicillin and other β-lactam antibiotics, despite their massive use. No strain which is resistant to penicillin has been described , and penicillin G minimum inhibitory concentrations have not varied significantly for the past 90 years. Macrolides and lincosamides (clindamycin) are considered the treatment of choice in patients who are allergic, or suspected to be allergic, to β-lactam antibiotics. In recent years, resistance to these groups has increased in different parts of the world, including Spain. However, this problem does not affect everybody in the same way; while 14-atom macrolides (erythromycin, clarithromycin) and 15-atom macrolides (azithromycin) present resistance rates of 10%–30%, those of 16 atoms (midecamycin, josamycin) and lincosamides remain below 7% resistance.15The prevalence of resistance to macrolides and lincosamides should be known and updated in each area so that alternatives to penicillin can be made available.
Is antibiotic overprescribed for AP?
Establishing a suspected differential aetiological diagnosis on which to base the most appropriate treatment is one of the main problems which AP poses for primary care physicians. Antibiotics are in general overprescribed for AP, as most of its causes are viral. The excessive use of antibiotics results in possible side effects for the patient, resistance selection and the consequent increase in health expenditure.4, 5, 6, 7
Is AP a viral infection?
Most AP cases are viral in origin and occur in the context of a common cold. They usually present in the form of epidemic outbreaks and are accompanied by viral symptoms such as nasal congestion, low-grade fever, cough, dysphonia, headache and myalgia. The course of bacterial AP is the acute onset of high fever with chills, severe odynophagia and dysphagia, but no general viral symptoms. Table 1shows the main clinical differences between viral and bacterial aetiologies. Table 2shows the main signs and symptoms suggestive of a specific aetiology in AP.
What bacteria cause pharyngitis?
Other bacteria may also cause pharyngitis, including streptococcus groups C and G, but due to the difficulty of distinguishing colonization from infection, it is difficult to quantify the relative rates of these bacterial causes. [4] Sexually transmitted infections, such as Neisseria gonorrhea and Chlamydia trachomatis, should be considered if risk factors are present, though they are typically asymptomatic. [5] Rarer infections, such as Yersinia pestis and Corynebacterium diphtheriae, could be considered if recent exposure to endemic areas is suspected. [6] [7]
How to diagnose bacterial pharyngitis?
As with most medical conditions, the diagnosis and management of bacterial pharyngitis depend on collecting an effective history and performing a directed physical exam. Bacterial pharyngitis is most commonly acute in onset with a relatively isolated severe sore throat, potentially with associated symptoms like the scarlatiniform rash or abdominal pain. [3] [4] Providers should collect information about associated symptoms, time course, previous history, and risk factors. Additional upper respiratory symptoms, such as congestion, cough, and eye irritation, suggest viral infections or seasonal allergies as more likely etiologies. [2] Seasonally recurrent or persistent symptoms with no fever favor allergic etiologies. History of acid reflux, positional exacerbation, and association with recent irritant foods, caffeine, or alcohol favors gastroesophageal reflux disease. Risk factors like high-risk sexual behavior or close family with strep throat may lower the bar for potential testing.
What is the allergic reaction to pollen?
Allergic reaction to environmental factors like pollen, indoor or outdoor pollutants or medications. Irritant pharyngitis due to gastroesop hageal reflux or smoking. Traumatic pharyngitis due to excessive shouting, snoring, or recent tracheal intubation. Aphthous ulcers.
What is the best treatment for pharyngitis?
The symptoms for any pharyngitis should be additionally treated with nonsteroidal anti-inflammatory drugs or acetaminophen for antipyresis and analgesia.
How to improve outcomes for pharyngitis?
The primary areas for improving outcomes around bacterial pharyngitis are in accurately identifying and responsibly treating the cause of patients' pharyngitides. Resulting from patients' expectations as well as limitations in the sensitivity and speed of current testing, current practice is often to inappropriately treat what is likely nonbacterial pharyngitis with antibiotics. [31] Following guidance from the Infectious Diseases Society of America, the American Academy of Pediatrics, and the Centers for Disease Control and Prevention, health care teams should embrace shared decision making with their patients and families. [2]
What are the complications of pharyngitis?
Generally, a bacterial infection can spread, leading to abscess, cellulitis, lymphadenitis, meningitis, and bacteremia.
What is a sore throat?
Pharyngitis, more commonly described as sore throat, represents inflammation or irritation of the posterior oropharynx. While the majority of cases arise by either non-infectious or non-bacterial causes, bacteria are responsible for a substantial portion of pharyngeal infections, and these infections present differently, ...
