Louis Pasteur developed the earliest effective vaccine against rabies that was first used to treat a human bite victim on 6 July 1885 [13].Mar 15, 2012
When did rabies vaccine for humans come out?
The first human vaccination with a rabies virus attenuated by exposure to dry air started on July 6, 1885, and was reported in the session of the French Academy of Sciences on October 26, 1885 (1).
When did treatment for rabies come out?
The first real treatment for rabies came in the 1880's. A French chemistry teacher named Louis Pasteur was dabbling with chicken cholera when he noticed that virulent cultures exposed to the elements no longer caused disease.
How was rabies treated in people 100 years ago?
The treatment consisted of 25 injections of rabies vaccine: three on the first day, two on the second, two on the third, and one each day after for 18 days. Each dose was slightly stronger, or more virulent, than the preceding, so that the body could build up immunity.Oct 28, 2013
How did they treat rabies in the 1800s?
Until Louis Pasteur and Emile Roux developed a vaccine in the mid-1880s, bite marks from rabid or suspected rabid animals often were treated by cutting away the flesh in and around the infected area and then cauterizing the wound with "lunar caustic" (fused silver nitrate).Dec 5, 2010
Who invented rabies vaccine for the first time?
On July 6, 1885, Pasteur vaccinated Joseph Meister, a nine-year-old boy who had been bitten by a rabid dog. The vaccine was so successful that it brought immediate glory and fame to Pasteur.
What animal did rabies originate from?
Given that rabies has been enzootic in Indian mongooses since their importation, it was once thought that epizootics in the Caribbean resulted from the introduction of infected animals from India (Smith et al., 1992).Mar 29, 2017
Why is there no cure for rabies?
Rabies infects the central nervous system (CNS), and — if left untreated — it can be fatal if it reaches the brain. Once it reaches the brain, there's currently no treatment available.Aug 19, 2021
How did humans stop rabies?
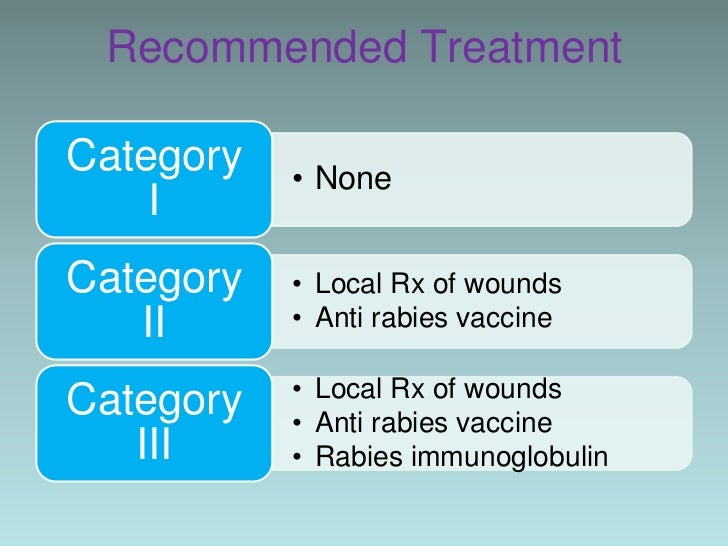
Rabies in humans can be prevented either by eliminating exposures to rabid animals or by providing exposed persons with prompt local treatment of wounds combined with appropriate passive and active immunization.
How did rabies first start?
Rabies Transmission
In 300 BCE, Aristotle noted the disease affected dogs and any animal bitten by infected dogs. In the 1st Century CE, the Roman scholar Celsus suggested the disease was transmitted via the saliva of an infected animal.Jul 9, 2020
In 300 BCE, Aristotle noted the disease affected dogs and any animal bitten by infected dogs. In the 1st Century CE, the Roman scholar Celsus suggested the disease was transmitted via the saliva of an infected animal.Jul 9, 2020
How did Jeanna Giese survive rabies?
Giese was put into an induced coma for two weeks while feeding and breathing tubes kept her alive.Jul 19, 2021
How long did the rabies vaccine take to develop?
The first rabies vaccine was introduced in 1885 and was followed by an improved version in 1908. Millions of people globally are vaccinated against the virus.
When was rabies first discovered and by who?
In 1804, Georg Gottfried Zinke first transmitted rabies1 from a rabid dog to a normal one, and from dog to a rabbit and a hen, by injection of saliva. This proved that the disease was infectious.
Overview
- Rabies is a deadly virus spread to people from the saliva of infected animals. The rabies virus is usually transmitted through a bite.Animals most likely to transmit rabies in the United States include bats, coyotes, foxes, raccoons and skunks. In developing countries of Africa and Southeast Asia, stray dogs are the most likely to spread rabies to people.Once a person begins s…
- Rabies is a deadly disease caused by a virus that is spread in the saliva of infected animals. All mammals can get rabies. People usually get rabies from licks, bites, or scratches from infected dogs and other animals such as bats, foxes, raccoons, and mongooses.
Treatment
- This is a fast-moving virus. If it is not treated soon after the symptoms have begun, the prognosis is poor. Therefore, if your cat has been in a fight with another animal, or has been bitten or scratched by another animal, or if you have any reason to suspect that your pet has come into contact with a rabid animal (even if your pet has been vaccinated against the virus), you must ta…
- Once a person has symptoms of rabies, there is no cure. At this stage immune globulin, vaccination and anti-viral drugs are of no benefit. A person can be kept alive indefinitely on a life-support system, but no-one has ever made a recovery from rabies. The usual care is to make the patient as comfortable as possible in the face of a painful and fearful death. High doses of pain…
- Once a rabies infection is established, there's no effective treatment. Though a small number of people have survived rabies, the disease is usually fatal. For that reason, if you think you've been exposed to rabies, you must get a series of shots to prevent the infection from taking hold.
- There is no specific treatment for rabies once the infection develops in a child. There have been very few survivors of the infection. Therefore, prevention is extremely important.
Symptoms
- The first symptoms of rabies may be very similar to the flu and may last for days. Later signs and symptoms may include: 1. Fever 2. Headache 3. Nausea 4. Vomiting 5. Agitation 6. Anxiety 7. Confusion 8. Hyperactivity 9. Difficulty swallowing 10. Excessive salivation 11. Fear of water (hydrophobia) because of the difficulty in swallowing 12. Hallucinations 13. Insomnia 14. Partia…
- Initially, a dog whos become infected may show extreme behavioral changes such as restlessness or apprehension, both of which may be compounded by aggression. Friendly dogs may become irritable, while normally excitable animals may become more docile. A dog may bite or snap at any form of stimulus, attacking other animals, humans and even inanimate objects. T…
- There are two forms of rabies: paralytic and furious. In the early symptom (prodomal) stage of rabies infection, the cat will show only mild signs of CNS abnormalities. This stage will last from one to three days. Most cats will then progress to either the furious stage, the paralytic stage, or a combination of the two, while others succumb to the infection without displaying any major sym…
- From the point where the rabies virus entered the body, the virus moves towards the brain along the nerves. A person may show the first signs of rabies an average of 1 to 3 months after the virus enters the body. In humans, the first symptoms of the disease are non-specific and resemble other viral infections. They include: 1. pain or tingling at the bite site 2. a general feeling of illnes…
Prevention
- To reduce your risk of coming in contact with rabid animals: 1. Vaccinate your pets. Cats, dogs and ferrets can be vaccinated against rabies. Ask your veterinarian how often your pets should be vaccinated. 2. Keep your pets confined. Keep your pets inside and supervise them when outside. This will help keep your pets from coming in contact with wild animals. 3. Protect small pets fro…
- Rabies is a 100% vaccine-preventable disease. Countries embarking on rabies elimination programmes have successfully experienced marked reductions, often progressing to the elimination of rabies. Elimination programs often revolve around mass dog vaccination campaigns, where at least 70% of the dog population should be covered in order to break the cy…
- Dogs who are not vaccinated or allowed outdoors without supervision have a higher risk of contracting rabies from an infected animal. Prevention is necessary to lower the risk of contracting or spreading this deadly disease.Dogs can be vaccinated for rabies. Some countries, such as the United Kingdom, don’t experience rabies and therefore don’t offer this vaccination. K…
- In many countries the risk of rabies is similar to the United States, including most of Europe, Japan, Canada, and Australia. However, in many other parts of the world, rabies in dogs is still a problem, and access to preventive treatment may be hard. These areas include much of Africa, Asia, and Central and South America. If traveling to a country where there is an increased risk of …
Diagnosis
- Rabies is diagnosed by testing fluids of the brain, skin, saliva and urine of an animal, not its blood serum. Diagnosis in the U.S. is done using a post-mortem direct fluorescence antibody test performed by a state-approved laboratory for rabies diagnosis. Your veterinarian will collect fluid samples if your cat dies while in quarantine, or if it begins showing progressive signs of rabies; i…
- As in many diseases, clinical suspicion is critical to a timely diagnosis of rabies. Rabies should be included in the differential diagnosis of any case of encephalitis of unknown origin, particularly when the patient has a history of an animal bite and signs of autonomic disturbance in the absence of coma. Thus, hyperventilation, hypersalivation, aerophobia, and hydrophobia are all p…
- Tests are performed on the animal that bit a person in order to confirm the presence of rabies in the animal. This requires killing the animal, if possible. This step is necessary because a person will not immediately show antibodies to the virus after being in contact with a rabid animal. If the bite came from a pet that appears sick, the pet is euthanized so its brain can be tested for rabies…
- Rabies is usually recognised by the history of a bite or exposure, symptoms and signs. However, the disease is rare, and if you do not report a recent dog bite, it can be difficult for a health care professional to identify rabies in the early stages. Often the disease is only confirmed after death. By law, a post-mortem examination is required in cases of suspected rabies. Typical changes in …
Cause
- Rabies infection is caused by the rabies virus. The virus is spread through the saliva of infected animals. Infected animals can spread the virus by biting another animal or a person. In rare cases, rabies can be spread when infected saliva gets into an open wound or the mucous membranes, such as the mouth or eyes. This could occur if an infected animal were to lick an open cut on yo…
- This severe, and often fatal, viral polioencephalitis also has zoonotic characteristics, and can therefore be transmitted to humans. Rabies is usually transmitted through the saliva of an infected animal and is most commonly spread through bites. It is still possible to get rabies from a cat scratch or a scratch from any infected animal, but it is less common. Some other less com…
- The bite of a rabid animal (an animal infected with rabies virus) is by far the most common cause of rabies. The virus is carried in the saliva of the rabid animal and is able to enter the body through an opening in the skin, such as a bite wound. Although it is possible to get rabies from a non-bite exposure, this is very rare. For example, non-bite exposures include inhalation of aerosol particle…
- Rabies is caused by the rabies virus and other related rabies-like viruses. Once the virus has entered the body, it enters peripheral nerves and is carried towards the brain. The virus multiplies in the brain, causing brain dysfunction and ultimately death. The disease is spread from animal to animal, and occasionally from animals to humans. Human to human transmission is theoreticall…
Epidemiology
- With the exception of Antarctica, rabies is endemic on all continents. Of the tens of thousands of deaths occurring annually due to rabies, 95% of cases are reported in Asia and Africa.
- Rabies is found around the world, except Antarctica. Travelers who may come into contact with wild or domestic animals are at risk for rabies. This includes travelers spending a lot of time outdoors (such as campers and cavers), travelers with occupational risks (such as veterinarians and wildlife professionals), and long-term travelers and expatriates. Children are also at higher ri…
- The epidemiology of human rabies is an exact reflection of the epizootiology of the disease in animals. From the viewpoint of public health, the dog or other canid species are the only important vector for humans, being responsible for most infections in Asia, Africa, and Latin America. However, with the retreat of canine rabies from most of the developed world, rabies tra…
- 1. Rabies occurs in all continents of the world except Antarctica, although some countries are rabies-free (including the UK). 2. Knowledge exists to eliminate the threat of canine rabies but lack of motivation by governments, cultural issues and lack of funding prevent progress. 3. There are estimated to be up to 61,000 deaths from rabies worldwide every year. 95% of these deaths occ…
Risk Factors
- Factors that can increase your risk of rabies include: 1. Traveling or living in developing countries where rabies is more common, including countries in Africa and Southeast Asia 2. Activities that are likely to put you in contact with wild animals that may have rabies, such as exploring caves where bats live or camping without taking precautions to keep wild animals away from your cam…
Prognosis
- The true burden of the disease is likely to be underestimated due to chronic underreporting and political neglect in many developing countries. Improved reporting systems are required to address the lack of accurate data and validate these estimates in a number of regions.
- Rabies affects the central nervous system, ultimately causing brain disease and death. Once symptoms of rabies appear, the disease is nearly always fatal, so prevention is especially important.
- It is essential to administer post-exposure prophylaxis correctly. Death is almost certain if early treatment fails to prevent progression to infection and prodromal symptoms.Only a handful of cases of survival of human rabies have been documented, mostly in people who had either been previously vaccinated or who had received post-exposure prophylaxis.
Pathophysiology
Once the virus enters the cat's body, it replicates in the cells of the muscles and then spreads to the closest nerve fibers, including all peripheral, sensory and motor nerves, traveling from there to the CNS via fluid within the nerves. The incubation of rabies is, on average, between one and three months, but can be as little as a day …
- The virus is transmitted in the saliva of rabid animals and generally enters the body via infiltration of virus-laden saliva from a rabid animal into a wound (e.g. scratches), or by direct exposure of mucosal surfaces to saliva from an infected animal (e.g. bites). The virus cannot infiltrate intact skin. Once the virus reaches the brain, it further replicates, resulting in presentation of clinical si…
- 1. Any mammal can carry rabies but transmission occurs to humans most commonly worldwide from dogs (over 99% of cases). 2. In some countries, bats, monkeys and cats can also transmit rabies. Even in countries which are free of terrestrial rabies, bats may carry a rabies-like virus. (The only case acquired in the UK in the last century was attributed to a bat.) Foxes, racoons an…