
Treatment modality of failing grafts was determined by the length of the stenotic lesion; short (≤2 cm) stenotic lesions were treated with percutaneous transluminal angioplasty (PTA) (Fig. 2A, B) while longer (>2 cm) stenotic lesions were treated with vein patch angioplasty or graft extension using a new autogenous vein graft. Fig. 2
Full Answer
Can drugs reduce vein graft failure in humans?
The team, led by Manfred Boehm, M.D., chief of the Laboratory of Cardiovascular Regenerative Medicine at NIH's National Heart, Lung, and Blood Institute, identified similar properties in samples of clogged human vein grafts, suggesting that select drugs might be used in reducing vein graft failure in humans.
What is vein graft failure?
Vein graft failure. In medicine, vein graft failure (VGF) is a condition in which vein grafts, which are used as alternative conduits in bypass surgeries (e.g. CABG), get occluded. Veins, mainly the great saphenous vein (GSV) are the most frequently used conduits in bypass surgeries (CABG or PABG), due to their ease of use and availability.
How to prevent vein graft occlusion?
To prevent vein graft occlusion, lifestyle management, antithrombotic therapies, and lipid-lowering therapies are key.
Why do vein grafts block up so often?
It also turns out, according to the new Hopkins-led study results, that one in five vein grafts blocks off within six months of surgery, usually because of blood clots. To find out why, Rade and his research colleagues first drilled down into the world of platelets, hoping to learn which of the many anticoagulation agents did the best job.
What happens when vein graft fails?
After grafting, the implanted vein remodels to become more arterial, as veins have thinner walls than arteries and can handle less blood pressure. However, the remodeling can go awry and the vein can become too thick, resulting in a recurrence of clogged blood flow.
What happens if a bypass graft fails?
Third, patients presenting with bypass graft failure are often old (mean age was 68–70 years in this study) and have worse baseline left ventricular function, hence may be at increased risk for heart failure or arrhythmias, and for developing noncardiac disease, such as infections and cancer.
What treatment can be taken for the occluded vein bypass grafts?
In the absence of effective pharmacological interventions for the treatment and prevention of occlusive vein graft disease, gene therapy has emerged as a potential therapeutic alternative. Gene therapy could improve vein graft patency by reducing early thrombosis, neointimal hyperplasia and atherosclerosis.
What causes vein graft failure?
Three processes are responsible for vein graft failure. Thrombosis, intimal hyperplasia and accelerated atherosclerosis contribute to graft failure in the acute, subacute and late postoperative periods, respectively.
Can a bypass graft be stented?
Sometimes, a coronary artery bypass graft may need to be repeated or you may need a procedure to widen your arteries using a small balloon and a tube called a stent (coronary angioplasty).
Can you have a second CABG?
— When a coronary artery bypass grafting (CABG) patient needs a second surgery because of recurrent chest pain, more often than not it's a percutaneous coronary intervention (PCI), commonly known as coronary angioplasty with stents.
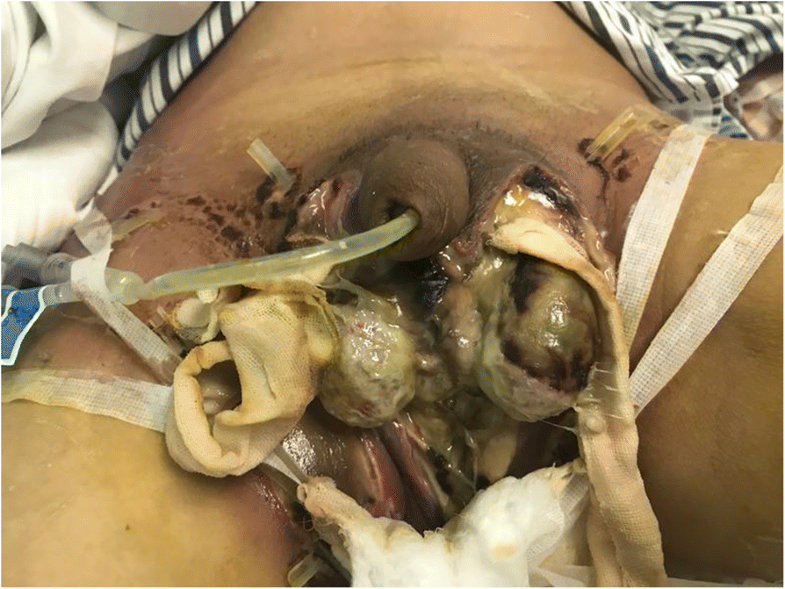
How is graft occlusion treated?
There have been various treatment strategies to manage occluded bypass grafts. Several treatment strategies of stenosis of fem-pop bypass graft have been proposed, including surgical revision orthrombectomy, balloon angioplasty, catheter-based thrombolysis, and repeat bypass grafting.
What causes early CABG graft failure?
Systemic Atherosclerotic Risk Factors In addition, other systemic factors (eg, platelet reactivity, age) might affect the individual response to medical therapy after CABG, therefore increasing the risk for early or late graft failure because of either thrombosis or atherosclerosis.
Can a bypass graft collapse?
Approximately 50% of saphenous vein grafts (SVGs) fail by 5 to 10 years post-coronary artery bypass grafting (CABG) and between 20–40% fail within the first year (1,2). While SVG failure can sometimes be silent, when symptomatic events occur, SVG percutaneous coronary intervention (PCI) is often performed.
How long does a vein graft last?
It's well known in cardiac circles, says Rade, that more than half of venous grafts will be completely blocked off within 10 years after the surgery. It also turns out, according to the new Hopkins-led study results, that one in five vein grafts blocks off within six months of surgery, usually because of blood clots.
Why do saphenous vein grafts fail?
Saphenous vein graft failure during the first year of surgery is due to technical errors, thrombosis, and intimal hyperplasia. All saphenous vein grafts experience endothelial damage during harvesting and initial exposure to arterial pressure.
How long will bypass grafts last?
How long do bypass grafts last? People tend to do very well after heart bypass and most get a good 15 years before needing another intervention, which at that point would almost always be having a stent inserted. Redoing heart bypass could also be an option if stenting weren't suitable.
How long does it take for a vein graft to fail?
However, the remodeling can go awry and the vein can become too thick, resulting in clogged blood flow. About 40% of vein grafts fail within 18 months of the operation.
Why is the great saphenous vein used as a bypass?
The great saphenous vein—the large vein running up the length of the leg—is often used as a bypass due to its size and the ease of removing a small segment. After grafting, implanted veins remodel to become more arterial.
What cells contribute to vein thickening?
By tracing the fate of endothelial cells, the researchers showed that endothelial-derived cells contribute to vein thickening through EndoMT.
What happens to the inside of a vein?
The scientists suspected that a process known as endothelial-to-mesenchymal transition, or EndoMT, may cause the inside of the vein to over-thicken. During EndoMT, endothelial cells that line the inner surface of the vein proliferate and convert into more fibrous and muscle-like cells.
What is bypass surgery?
Bypass surgery is a common procedure in the United States. A healthy artery or vein from elsewhere in the body is grafted onto arteries that feed the heart to bypass clogged vessels and restore blood flow.
What happens to the veins after engraftment?
During and after the harvesting, veins go through a period of ischemia and reperfusion after engraftment, which causes damage to endothelial and smooth muscle cells (SMC). The grafting exposes the vein to arterial pressure and flow that causes increased shear stress and wall tension, which further damages the endothelial layer and SMC. The damage causes local release of tissue factors and reduced bioavailability of prostacyclin and nitric oxide (NO), all of which contribute to platelet activation, deposition of fibrin, which promotes thrombosis. Growth factors that released from macrophages and platelets lead to increased proliferation and migration of SMCs to the intima. The migrated SMC release extracellular matrix resulting in reduced intimal cellularity. Low levels of endothelial nitric oxide, adenosine and prostaglandins, further contribute to SMC proliferation. Over time continued SMC migration and proliferation cause extracellular matrix deposition and fibrotic change that lead to development of intimal hyperplasia, which results in luminal loss that makes the graft more susceptible to atherosclerosis. Progressive atherosclerosis is the primarily cause of late vein graft failure. Vein graft atherosclerotic lesions are more diffuse and concentric, yet less calcified, compared to native atherosclerotic lesions, and are more susceptible to thrombosis formation and rupture.
What is the best treatment for VGF?
Statins and antiplatelets such as aspirin, are the only medications recommended by the ESC guidelines and the ACC/AHA Task Force guidelines for the prevention of VGF. Different surgical techniques had been studied in attempt to reduce VGF.
What is a VGF?
In medicine, vein graft failure (VGF) is a condition in which vein grafts, which are used as alternative conduits in bypass surgeries (e.g. CABG ), get occluded . Veins, mainly the great saphenous vein (GSV) are the most frequently used conduits in bypass surgeries ( CABG or PABG), due to their ease of use and availability.
How to prevent VGF?
Gene therapy is another strategy that been suggested to prevent VGF as the veins are ideally suited for ex vivo treatment prior to grafting. Preclinical studies showed that such strategy has the potential to reduce intimal hyperplasia but more clinical data is needed.
Can VGF cause ischemia?
VGF may be identified in asymptomatic patients, but can also produce symptoms of ischemia, depending on the area of the supplied territory of the heart, and the function of native arteries and other grafts. VGF has been closely correlated with revascularization, myocardial infarction and death.
Does EVH cause stenosis?
Although, EVH has been associated with higher risk of vein graft stenosis and occlusion. The solutions in which vein grafts are stored after harvesting also play an important role. Buffered saline, instead of saline or blood, has shown to reduce the risk of significant stenosis or occlusion.
Is VGF a revascularization?
VGF has been closely correlated with revascularization, myocardial infarction and death. Treatment of occluded GSVs can be performed by percutaneous coronary intervention or redo CABG and is considered to be challenging, and thus preventing their obstruction is of great importance.
How long does it take for a venous graft to block off?
It’s well known in cardiac circles, says Rade, that more than half of venous grafts will be completely blocked off within 10 years after the surgery. It also turns out, according to the new Hopkins-led study results, that one in five vein grafts blocks off within six months of surgery, usually because of blood clots.
Where are vein grafts located?
According to study co-investigator John Conte, surgeons usually count on one or two single available arteries—the left and right internal mammary arteries—conveniently located within every rib cage right next to the heart.
What veins do surgeons use for bypass?
But for additional bypass, surgeons typically resort to the leg veins. The trouble with veins, as surgeons know, stems from venous tissues’ native purpose of moving the body’s low-pressure blood flow back to the heart.
Did God make veins into arteries?
“God did not make veins to be turned into arteries,” says cardiologist Jeffrey Rade. “When you try to do that, they can act in unpredictable ways.”.
Can veins be harvested from a patient's legs?
Though they may provide the most plentiful source of replacement vessels for surgeons facing an extensively diseased heart, veins harvested from a patient’s legs are never a surgeon’s first choice.
What is CABG surgery?
CABG is the most commonly performed cardiac surgical procedure worldwide and is preferred over percutaneous coronary intervention in patients with diabetes, reduced left ventricular ejection fraction, and three vessel and complex coronary artery disease. 1 Both arterial and saphenous vein grafts (SVG) can be used as conduits.
What are the risk factors for SVG failure?
It is established that smoking 18 and hyperlipidaemia 24 are associated with SVG failure. Diabetes and probably hypertension influence graft occlusion after CABG, 25,26 and management of both decreases adverse clinical events. 27,28 Therefore, addressing risk factors by adequate secondary prevention remains the cornerstone of strategies to improve graft patency.
What happens in the first month after CABG?
In the first month after CABG, mechanical factors and endothelial damage after surgery cause thrombotic occlusion. 10 Thereafter, until 1 year after CABG, the predominant process causing failure is intimal hyperplasia.
Does dipyridamole improve SVG patency?
However, studies investigating additional antithrombotic therapies after CABG have not provided definite conclusions. Addition of dipyridamole does not appear to improve SVG patency 34 and might lead to worse clinical outcomes after CABG 35; therefore, it is not recommended. 32,33.
Does clopidogrel improve SVG?
The addition of the P2Y12 inhibitor clopidogrel to aspirin did not improve SVG patency in certain studies, 5 whereas in others it showed better SVG patency. 36 This may be due to 30% of patients having an inadequate inhibitory response to clopidogrel.
What is bypass surgery?
Bypass surgery to restore blood flow hindered by clogged arteries is a common procedure in the United States. The great saphenous vein, which is the large vein running up the length of the leg, often is used as the bypass conduit due to its size and the ease of removing a small segment.
What cells are responsible for narrowing blood vessels?
Endothelial cells not only form the inner lining of a blood vessel, but also contribute to blood vessel narrowing as shown in this mouse vein graft model. Endothelial cells (green) lose their typical morphology and become more like smooth muscle cells (red).
Can a vein remodel after grafting?
After grafting, the implanted vein remodels to become more arterial , as veins have thinner walls than arteries and can handle less blood pressure. However, the remodeling can go awry and the vein can become too thick, resulting in a recurrence of clogged blood flow.
