Medication
For most people, PVCs with an otherwise normal heart won't need treatment. However, if you have frequent PVCs, your doctor might recommend treatment. In some cases, if you have heart disease that could lead to more-serious rhythm problems, you might need the following: Lifestyle changes.
Procedures
If the burden of PVCs is low, the evaluation as described earlier reveals no relevant underlying condition, and the ejection fraction is normal, reassurance alone may be reasonable and sufficient. In fact, determining therapy based on symptoms requires some important questions for the patient.
Do you need treatment for PVCs?
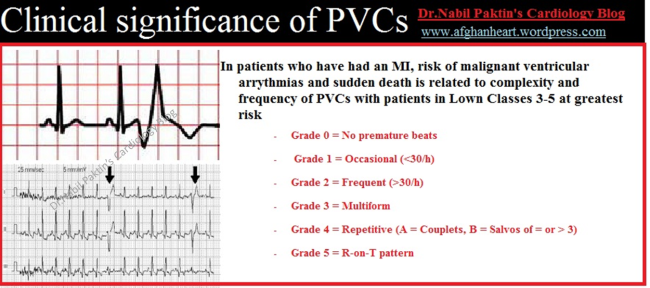
Most PVCs occur infrequently and are benign. Frequent PVCs may increase the risk of developing other, more serious cardiac arrhythmias. Individuals with frequent PVCs who have underlying heart disease, structural abnormalities in the heart or have had a previous heart attack have a higher risk of death.
When is reassurance alone sufficient for patients with PVCs?
The clinician is often faced with the dilemma of finding PVCs in a patient and deciding whether the PVCs should be treated. Management of PVCs includes discernment of associated heart disease and other predisposing conditions prior to the decision to specifically treat the PVCs.
What is the prognosis of PVCs?
What is the role of the clinician in managing PVCs?
When should you seek treatment for PVCs?
For most people, PVCs occur infrequently and are benign. You should consult a heart specialist if you experience frequent, regular or prolonged (duration of several minutes) PVCs, or are experiencing PVCs and have a structural heart problem or heart disease or have had a heart attack.
Is it normal to have PVCs every day?
Quantity of PVCs: A 24-hour-holter monitor tells us how many PVCs occur on a given day. The normal person has about 100,000 heartbeats per day (athletes a few fewer). Patients with more than 20,000 PVCs per day are at risk for developing cardiomyopathy (weak heart).
What is considered high PVC burden?
[72-74] Although symptomatic patients usually suffer from a high PVC burden (>10000 PVCs/24h), symptoms are not exclusive to these patients and those with a smaller PVC burden (<5000/24h) may also be highly symptomatic and warrant ablation.
Should I go to the hospital for PVCs?
They usually go away on their own. They don't need treatment. Talk to your doctor if you have other symptoms along with PVCs, such as dizziness, lightheadedness, or fainting. If you have a known heart problem, such as heart failure or a heart attack, PVCs may be a sign that a dangerous heart rhythm could occur.
Can you live a long life with PVCs?
In general even those with fairly frequent PVC's who have had underlying heart disease ruled out can be reassured and likely have a good prognosis.
Why am I suddenly getting PVCs?
Heart disease or scarring that interferes with the heart's normal electrical impulses can cause PVCs. Certain medications, alcohol, stress, exercise, caffeine or low blood oxygen, which is caused by chronic obstructive pulmonary disease (COPD) or pneumonia, can also trigger them.
Is PVCs considered a heart condition?
Premature ventricular complexes (PVCs) are the most common ventricular arrhythmia. Their prognostic significance cannot be interpreted without considering the presence or absence of any associated underlying cardiac condition. In the absence of structural heart disease, PVCs were generally considered to be benign.
Can frequent PVCs be benign?
It is a relatively common occurrence for cardiovascular clinicians to see patients with frequent premature ventricular contractions. Frequent and apparently idiopathic PVCs are usually considered a benign condition that can be managed with conservative measures.
How often do PVCs turn into Vtach?
It is important to note that three or more consecutive PVCs are classified as ventricular tachycardia.
At what heart rate should you go to the ER?
If you're sitting down and feeling calm, your heart shouldn't beat more than about 100 times per minute. A heartbeat that's faster than this, also called tachycardia, is a reason to come to the emergency department and get checked out. We often see patients whose hearts are beating 160 beats per minute or more.
Does working out help PVCs?
Many patients experience PVCs or palpitations before and after exercise, but not during exercise. When most patients start to exercise, their own heart rate rises and the PVCs or other extra beats disappear at higher heart rates.
Does magnesium help with PVCs?
Oral magnesium supplementation reduces the frequency of PVCs and/or PACs. Oral magnesium supplementation reduces the symptoms associated with PVCs and PACs.
Is a stress test useful for PVCs?
If there are exertional symptoms, a stress test is helpful. It's useful to divide the PVCs into two groups, multi-focal, as shown on the left have multiple morphologies and mandate evaluation for underlying structural heart disease.
Can PVCs be unifocal?
On the other hand, unifocal PVCs in which they have a single morphology, may suggest a normal heart with an abnormal electrical focused. Treatment is indicated if it's symptomatic, if there's a drop in ejection fraction, or if there's left ventricular enlargement.
How to control PVCs?
You can help control your PVCs by reducing or eliminating your caffeine, tobacco and alcohol intake and reducing stress and anxiety.
Why do PVCs go away?
When PVCs are due to some form or heart disease or structural abnormality, treating that problem often causes the PVCs to go away. A beta blocker medication may be prescribed for patients with PVCs who have heart failure or who have had a heart attack.
What is premature ventricular contraction?
What are premature ventricular contractions? A premature ventricular contraction (PVC) is a too-early heartbeat that originates in the ventricles and disrupts the heart’s normal rhythm. The pattern is a normal beat, an extra beat (the PVC), a slight pause, then a stronger-than-normal beat.
Do older people have PVCs?
PVCs occur more commonly in older people and in individuals with underlying heart disease , including a history of heart attack. People with a family history of cardiac arrhythmias (abnormal heart rhythm) also have a higher risk for PVCs.
Can caffeine cause PVCs?
Certain medications, alcohol, illegal drugs and high levels of adrenaline due to stress, exercise or caffeine also can cause PVCs. Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services.
Can frequent PVCs cause heart problems?
Frequent PVCs may increase the risk of developing other, more serious cardiac arrhythmias. Individuals with frequent PVCs who have underlying heart disease, structural abnormalities in the heart or have had a previous heart attack have a higher risk of death.
What is the purpose of PVCs?
From the sinus node, electrical impulses travel across the atria to the ventricles, causing them to contract and pump blood to your lungs and body. PVCs are abnormal contractions that begin in the ventricles. These extra contractions usually beat sooner than the next expected regular heartbeat.
What are the symptoms of premature ventricular contractions?
But you might feel an odd sensation in your chest, such as: Fluttering. Pounding or jumping. Skipped beats or missed beats. Increased awareness of your heartbeat.
What to do if you have PVCs?
If you have PVCs, your doctor may want to perform a cardiac evaluation, looking for previously unknown heart disease and assessing your risk of developing heart disease in the future. 1
How common are PVCs?
PVCs are relatively common. In fact, around 50% of people with or without heart disease will have at least one PVC during a 24-hour Holter monitor study. 1 Those who have more than three PVCs in a row are said to have non-sustained ventricular tachycardia (NSVT).
What is premature ventricular complex?
Treatment. A premature ventricular complex (PVC, or premature ventricular contraction) is an extra electrical impulse arising from one of the heart's ventricles. This extra impulse happens before the next normal heartbeat has a chance to occur.
What is PVC in medical terms?
Dr. Ali is also an award-winning writer. A premature ventricular complex (PVC, or premature ventricular contraction) is an extra electrical impulse arising from one of the heart's ventricles. This extra impulse happens before the next normal heartbeat has a chance to occur.
How to tell if you have PVC?
Those who do experience PVC symptoms may notice one or more of the following: 3 1 Shortness of breath 2 Lightheadedness 3 Fatigue 4 Palpitations (an unusual awareness of the heartbeat)
Is PVC dangerous?
The bulk of evidence today suggests that PVCs usually aren't inherently dangerous. In fact, studies have shown that suppressing PVCs with antiarrhythmic drugs may actually increase the risk of death in certain patients, indicating that the drug is more dangerous than the PVC. 6.
Can PVC cause cardiomyopathy?
People with frequent PVCs are more likely to have or develop significant heart disease. There is evidence that if PVCs are persistent and very frequent (more than 15% of all heartbeats), they can sometimes lead to PVC-induced cardiomyopathy. 1.
Can PVC be ruled out?
Therapeutic options: (1) This depends heavily on patient's symptoms and observed PVC frequency - once identified, and cardiac disease is ruled out, many patients can be reassured. If they learn to avoid potential triggers such as stress, alcohol or caffeine, this may be all that is required.
Can PVC be divided into structural or structural?
PVC therapies: From a clinical perspective it is useful to divide patients with frequent PVCs into those with and those without structural heart disease: PVCs in patients with structural heart disease such as LVH, cardiomyopathy, and congestive heart failure, prior myocardial infarction, etc.
Can a 12-lead EKG detect PVC?
While patients may be asymptomatic, typically these PVCs cause sensations of skipping, heart pounding, and possibly chest pain, shortness of breath or dizziness. The 12-lead EKG is very useful in identifying the PVC morphology, as certain clinical syndromes exhibit very characteristic PVC morphologies (see below).
Can PVCs be seen without structural heart disease?
PVCs and symptoms related to PVCs are seen frequently in clinical practice, can occur in patients with or without structural heart disease, and often require therapy to improve symptoms. Once identified …. • Assess PVC morphology on 12 lead EKG (monomorphic or not – need long 12 lead rhythm strip)
What is the best treatment for PVCs?
In the presence cardiac disease such as cardiac ischemia, infarction, or heart failure and symptoms from PVCs, optimal medical therapy including beta-blockers and ACE inhibitors may improve symptoms. Amiodarone and ablation may be considered for refractory symptoms in all patients.
What is the dilemma of finding PVCs in a patient?
The clinician is often faced with the dilemma of finding PVCs in a patient and deciding whether the PVCs should be treated. Management of PVCs includes discernment of associated heart disease and other predisposing conditions prior to the decision to specifically treat the PVCs. Prevalence.
What is premature ventricular contraction?
Premature ventricular contractions are frequently encountered and management is determined by symptoms, precipitating factors, and the presence of underlying cardiac disease. No specific medical treatment is indicated in asymptomatic PVCs or tolerable symptoms in the absence of cardiac disease; if a reversible cause of PVCs is not determined, ...
Is there any evidence that suppression of PVCs with medications improves mortality?
In the absence of symptoms and structural heart disease, no treatment is needed, and reassurance is recommended. There is no evidence that suppression of PVCs with medications in this situation improves mortality.
Can PVCs be treated without cardiac disease?
No treatment is indicated in patients with asymptomatic PVCs in absence of cardiac disease. Symptomatic patients without cardiac disease may be managed by identifying and correcting reversible causes. In patients with cardiac disease, management includes treating the underlying cardiac disease to improve both symptoms and prognosis.
How common are PVCs?
PVCs are common among the general population . The estimated prevalence ranges from 1% to 4% on electrocardiogram and 40% to 75% on a 24 or 48-hour Holter monitor.[6] . Young and healthy adults have shown a highly similar frequency rate of PVCs in contrast to the older segments of the general population.
What causes PVCs?
In many cases, excess intake of stimulants and/or lower levels of potassium and magnesium is the cause of the PVCs. These patients can be easily managed via minimization of stimulants and/or repletion of electrolytes.
What is a PVC in a heart?
Continuing Education Activity. During a premature ventricular contraction (PVC), the heartbeat is initiated by the Purkinje fibers rather than the SA node. Given that a PVC occurs before a regular heartbeat, there is a pause before the next regular heartbeat. PVCs can occur in isolation or in repeated patterns.
What is the result of premature ventricular contraction?
The result is the contraction of the ventricles and pumping of blood from the heart out to the body's arteries. [1] During a premature ventricular contraction (PVC), the heartbeat is initiated by the Purkinje fibers rather than the SA node. Given that a PVC occurs before a regular heartbeat, there is a pause before the next regular heartbeat. [2]
What is it called when you have three consecutive PVCs?
It is important to note that three or more consecutive PVCs are classified as ventricular tachycardia. If the PVCs continuously alternate with a regular sinus beat, the patient is in bigeminy.[3] Likewise, if every third heartbeat is a PVC, then it is named trigeminy. PVCs present as heart palpitations in most patients.
Why do PVCs have triggered beats?
The final explanation for PVCs is that triggered beats occur due to after-depolarizations. [7] On the molecular level, there are a few changes that create an environment for spontaneous depolarization of the ventricular myocytes. These include hypokalemia, hypomagnesemia, excess calcium, and excess catecholamines.
What is the most common sensation associated with PVCs?
History and Physical. The most common sensation associated with PVCs is that of a skipped heartbeat followed by a fluttering sensation. Patients commonly present complaining of heart palpitations. The vast majority of patients are entirely asymptomatic as there are no associated symptoms with the palpitations.
What is the first indication of PVC frequency?
Similarly, that physical examination may be the first indication of PVC frequency, which ultimately may prove to be clinically relevant.
What is the most useful contribution a physician can provide a patient with PVCs?
In many cases, the most useful contribution a physician can provide a patient with PVCs is reassurance. In considering whether additional management beyond reassurance should be pursued, 3 key pieces of information are needed: (1) information regarding symptoms, (2) the burden of the PVCs (typically reported in PVCs as a percentage of all beats), and (3) the presence or absence of structural heart disease.
What are the causes of PVCs?
Premature ventricular complexes (PVCs) are extremely common, found in the majority of individuals undergoing long-term ambulatory monitoring. Increasing age, a taller height, a higher blood pressure, a history of heart disease, performance of less physical activity, and smoking each predict a greater PVC frequency. Although the fundamental causes of PVCs remain largely unknown, potential mechanisms for any given PVC include triggered activity, automaticity, and reentry. PVCs are commonly asymptomatic but can also result in palpitations, dyspnea, presyncope, and fatigue. The history, physical examination, and 12-lead ECG are each critical to the diagnosis and evaluation of a PVC. An echocardiogram is indicated in the presence of symptoms or particularly frequent PVCs, and cardiac magnetic resonance imaging is helpful when the evaluation suggests the presence of associated structural heart disease. Ambulatory monitoring is required to assess PVC frequency. The prognosis of those with PVCs is variable, with ongoing uncertainty regarding the most informative predictors of adverse outcomes. An increased PVC frequency may be a risk factor for heart failure and death, and the resolution of systolic dysfunction after successful catheter ablation of PVCs demonstrates that a causal relationship can be present. Patients with no or mild symptoms, a low PVC burden, and normal ventricular function may be best served with simple reassurance. Either medical treatment or catheter ablation are considered first-line therapies in most patients with PVCs associated with symptoms or a reduced left ventricular ejection fraction, and patient preference plays a role in determining which to try first. If medical treatment is selected, either β-blockers or nondihydropyridine calcium channel blockers are reasonable drugs in patients with normal ventricular systolic function. Other antiarrhythmic drugs should be considered if those initial drugs fail and ablation has been declined, has been unsuccessful, or has been deemed inappropriate. Catheter ablation is the most efficacious approach to eradicate PVCs but may confer increased upfront risks. Original research remains necessary to identify individuals at risk for PVC-induced cardiomyopathy and to identify preventative and therapeutic approaches targeting the root causes of PVCs to maximize effectiveness while minimizing risk.
What is a PVC in EKG?
Premature ventricular complexes (PVCs) are observed in the majority of individuals monitored for more than a few hours, and the absence of a PVC will likely become more of a rare phenomenon as longer monitoring devices are used. The direct-to-consumer wearables with ECG capabilities, such as the Apple Watch and the Alivecor Kardia device, ...
Why does absence of PVC occur intermittently?
It is important to note that the absence of a PVC may occur intermittently because of ventricular refractoriness related to the separate underlying rhythm, and therefore multiples of the parasystolic PVC interval should be considered before excluding automaticity.
Is a PVC asymptomatic?
PVCs are commonly asymptomatic but can also result in palpitations, dyspnea, presyncope, and fatigue. The history, physical examination, and 12-lead ECG are each critical to the diagnosis and evaluation of a PVC. An echocardiogram is indicated in the presence of symptoms or particularly frequent PVCs, and cardiac magnetic resonance imaging is ...
Is premature depolarization a mechanical contraction?
Of note, the Heart Rhythm Society consensus recommends the term “premature ventricular complex” and not “ventricular premature depolarization” or “premature ventricular contraction” to standardize the literature and acknowledge that electric activity may not lead to mechanical contraction. 1.

Diagnosis
Clinical Trials
Lifestyle and Home Remedies
Preparing For Your Appointment