Medication
For some people, Barrett's esophagus can heal, per Cedars Sinai, though it's typically a permanent condition. Tip If you have severe or frequent GERD symptoms or take heartburn medicine more than twice a week, visit your doctor to get treatment and check for Barrett's esophagus, per the Mayo Clinic.
Procedures
Those who asked “can Barrett’s esophagus be cured?” and find that the answer is “no” can at least take relief in the fact that management and treatment of Barrett’s are possible, and can greatly improve your quality of life.
Therapy
In GERD, stomach contents wash back into the esophagus, damaging esophagus tissue. As the esophagus tries to heal itself, the cells can change to the type of cells found in Barrett's esophagus. However, some people diagnosed with Barrett's esophagus have never experienced heartburn or acid reflux.
Self-care
Barrett’s esophagus does not proceed to cancer in all patients; however, it is estimated that around 10–15% of cases of BE may progress to esophageal cancer. There are two kinds of cell transformations that are associated with either squamous cell or adenocarcinoma of the esophagus.
Nutrition
Does Barretts esophagus ever heal?
Does Barretts esophagus get better?
Can Barrett's esophagus heal itself?
How often does Barrett's turn to cancer?
See more

Can Barrett's esophagus be cured?
There is no cure for Barrett's esophagus. Your care plan will try to stop any more damage by keeping acid reflux out of your esophagus.
Is Barrett's esophagus serious?
Barrett's esophagus is a potentially serious complication of GERD, which stands for gastroesophageal reflux disease. In Barrett's esophagus, normal tissue lining the esophagus -- the tube that carries food from the mouth to the stomach -- changes to tissue that resembles the lining of the intestine.
What is the survival rate for Barrett's esophagus?
During the 1960s and 1970s, only about 5% of patients survived at least 5 years after being diagnosed. Now, about 20% of patients survive at least 5 years after diagnosis.
What medications should be avoided with Barrett's esophagus?
Some studies have found that the risk of cancer of the esophagus is lower in people with Barrett's esophagus who take aspirin or other non-steroidal anti-inflammatory drugs (NSAIDs), such as ibuprofen. However, taking these drugs every day can lead to problems, such as kidney damage and bleeding in the stomach.
What is the best medication for Barrett's esophagus?
Proton pump inhibitors (PPIs) are drugs that block the three major pathways for acid production. PPIs suppress acid production much more effectively than H2 blockers. PPIs are the most effective medication for healing erosive esophagitis and providing long-term control of GERD symptoms.
How often should you have an endoscopy with Barrett's esophagus?
Usually, you don't need treatment at this stage. But your healthcare provider will want to monitor the condition. You'll need to have an upper endoscopy every two to three years.
How do you keep your Barrett's esophagus from progressing?
Getting plenty of fiber in your daily diet is good for your overall health. Medical research shows that it may also help prevent Barrett's esophagus from worsening and lower your risk of cancer in the esophagus. Add these and other fiber-rich foods to your daily diet: fresh, frozen, and dried fruit.
Are there stages of Barrett's esophagus?
DISEASE PROGRESSION AND COMPLICATIONS Barrett's esophagus can progress to more serious stages, potentially resulting in esophageal adenocarcinoma, a type of esophageal cancer. There are three stages of Barrett's esophagus, which range from intestinal metaplasia without dysplasia to high-grade dysplasia.
What are the stages of Barrett's disease?
The stages of Barrett's esophagus are:non-dysplastic (no cancerous tissue present)low-grade dysplasia (minor cell changes found)high-grade dysplasia (extensive cell changes found, but not yet cancer)noninvasive cancer.invasive cancer.
How long should you take omeprazole for Barrett's esophagus?
Continuous treatment with omeprazole 20 mg daily for up to 6 years in Barrett's oesophagus.
How does Barrett's esophagus make you feel?
A burning sensation after eating is heartburn. If heartburn occurs two or more times a week, it's considered gastroesophageal reflux disease (GERD). Along with heartburn or GERD, it's typical for those with Barrett's esophagus to experience regurgitation of stomach contents.
How long does it take for Barrett's esophagus to become cancerous?
This cohort study showed that the incubation period from Barrett esophagus to invasive cancer is likely more than 30 years.
Can you live a long life with Barrett's esophagus?
Those who are diagnosed with Barrett's Esophagus can expect to live a normal life. This condition is treatable and doesn't hold any risk of premature death. However, Barrett's Esophagus is a serious condition and should be under the treatment guidelines recommended to you by a gastroenterologist.
How long does it take for Barrett's esophagus to become cancerous?
This cohort study showed that the incubation period from Barrett esophagus to invasive cancer is likely more than 30 years.
Does Barrett's esophagus shorten your life?
Solaymani-Dodaran et al[26] demonstrated that overall mortality in patients with Barrett's esophagus was 21% higher than in control subjects from the general population (with higher rates of neoplastic, respiratory and gastrointestinal causes of death).
Are there stages of Barrett's esophagus?
DISEASE PROGRESSION AND COMPLICATIONS Barrett's esophagus can progress to more serious stages, potentially resulting in esophageal adenocarcinoma, a type of esophageal cancer. There are three stages of Barrett's esophagus, which range from intestinal metaplasia without dysplasia to high-grade dysplasia.
What is the treatment for Barrett's esophagus?
If you have Barrett’s esophagus and gastroesophageal reflux disease (GERD), your doctor will treat you with acid-suppressing medicines called proton pump inhibitors (PPIs). These medicines can prevent further damage to your esophagus and, in some cases, heal existing damage.
How does Barrett's mucosal resection work?
In endoscopic mucosal resection, your doctor lifts the Barrett’s tissue, injects a solution underneath or applies suction to the tissue, and then cuts the tissue off. The doctor then removes the tissue with an endoscope. Gastroenterologists perform this procedure at certain hospitals and outpatient centers. You will receive local anesthesia to numb your throat and a sedative to help you relax and stay comfortable.
How often should you do endoscopy surveillance?
Experts aren’t sure how often doctors should perform surveillance endoscopies. Talk with your doctor about what level of surveillance is best for you. Your doctor may recommend endoscopies more frequently if you have high-grade dysplasia rather than low-grade or no dysplasia. Read whether people with Barrett’s esophagus are more likely to develop cancer.
What is the alternative to endoscopic surgery?
Surgery called esophagectomy is an alternative to endoscopic therapies. Many doctors prefer endoscopic therapies because these procedures have fewer complications.
What is endoscopic ablative therapy?
Endoscopic ablative therapies use different techniques to destroy the dysplasia in your esophagus. After the therapies, your body should begin making normal esophageal cells. A doctor, usually a gastroenterologist or surgeon, performs these procedures at certain hospitals and outpatient centers.
What is the procedure to numb your throat?
You will receive local anesthesia to numb your throat and a sedative to help you relax and stay comfortable. Before performing an endoscopic mucosal resection for cancer, your doctor will do an endoscopic ultrasound. Complications can include bleeding or tearing of your esophagus.
How long does it take to recover from esophageal surgery?
The surgery is performed at a hospital. You’ll receive general anesthesia, and you’ll stay in the hospital for 7 to 14 days after the surgery to recover.
What is the best way to determine if you have Barrett's esophagus?
Endoscopy is generally used to determine if you have Barrett's esophagus.
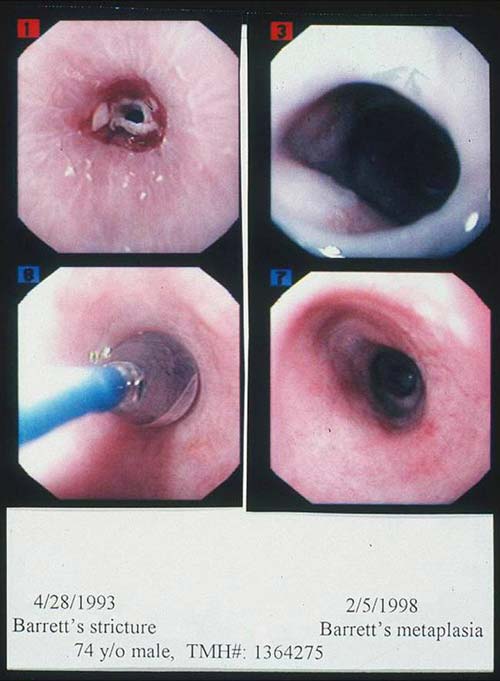
What is the video camera used to see Barrett's esophagus?
Barrett's esophagus has a distinct appearance when viewed during an endoscopy exam. During endoscopy, the doctor passes a flexible tube with a video camera at the tip (endoscope) down your throat and into the swallowing tube (your esophagus). The video camera detects surface abnormalities, such as acid reflux damage or the presence of a hiatal hernia or ulcers, as well as Barrett's esophagus.
What is the best treatment for esophageal cancer?
But, given the risk of esophageal cancer, treatment may be recommended if the diagnosis is confirmed. Preferred treatments include: Endoscopic resection , which uses an endoscope to remove damaged cells to aid in the detection of dysplasia and cancer. Radiofrequency ablation, which uses heat to remove abnormal esophagus tissue.
How to treat GERD?
Treatment for GERD. Medication and lifestyle changes can ease your signs and symptoms. Surgery or endoscopy procedures to correct a hiatal hernia or to tighten the lower esophageal sphincter that controls the flow of stomach acid may be an option.
Can Barrett's esophagus reoccur?
Recurrence of Barrett's esophagus is possible after treatment. Ask your doctor how often you need to come back for follow-up testing. If you have treatment other than surgery to remove abnormal esophageal tissue, your doctor is likely to recommend lifelong medication to reduce acid and help your esophagus heal.
Is Barrett's esophagus a low grade or high grade?
No dysplasia, if Barrett's esophagus is present but no precancerous changes are found in the cells. Low-grade dysplasia, if cells show small signs of precancerous changes. High-grade dysplasia, if cells show many changes. High-grade dysplasia is thought to be the final step before cells change into esophageal cancer.
Can acid back up in the esophagus?
This reinforces the lower esophageal sphincter, making it less likely that acid will back up in the esophagus. High-grade dysplasia is generally thought to be a precursor to esophageal cancer. For this reason, your doctor may recommend endoscopic resection, radiofrequency ablation or cryotherapy.
How to diagnose Barrett's esophagus?
How is Barrett's esophagus diagnosed? The only way to confirm the diagnosis of Barrett's esophagus is with a test called an upper endoscopy. This involves inserting a small lighted tube (endoscope) through the throat and into the esophagus to look for a change in the lining of the esophagus.
What is Barrett's esophagus?
Barrett’s esophagus is a change in the tissue lining your esophagus, the tube in your throat that carries food to your stomach. For reasons no one understands completely, cells in the esophageal lining sometimes become more like intestinal cells. Researchers suspect that having acid reflux or gastroesophageal reflux disease (GERD) ...
How to keep esophagus healthy?
The best way to keep the lining of your esophagus healthy is to address heartburn or GERD symptoms. People with ongoing, untreated heartburn are much more likely to develop Barrett’s esophagus. Untreated heartburn raises the risk of esophageal adenocarcinoma by 64 times.
What is the procedure to remove a spot on the esophagus?
Surgery: If you have severe dysplasia or esophageal cancer, your provider may recommend an esophagectomy, a surgery to remove all or part of the esophagus.
Why does Barrett's esophagus irritate?
This chronic (ongoing) condition occurs when stomach contents flow backward into the esophagus. Experts believe the acidic liquid irritates the lining of the esophagus, leading to changes in the tissue. But you can also have Barrett’s esophagus without having GERD.
What is the most common procedure for esophageal sloughing?
Radiofrequency ablation: This is the most common procedure. It burns off abnormal tissue using radio waves, which generate heat. Cryotherapy: Healthcare providers use liquid nitrogen to freeze diseased parts of the esophagus lining so it will slough off (shed).
How to treat GERD?
If you have GERD, your healthcare provider may prescribe medications to treat GERD. These medicines decrease stomach acid, which can protect your esophagus from damage. Lifestyle changes, like sleeping slightly inclined and avoiding eating dinner late, often help, too.
What is the procedure to remove Barrett's esophagus?
The last and final step for treating Barrett's esophagus is the surgical removal of the damaged sections of the esophagus, a procedure called esophagectomy.
What is the procedure for esophageal mucosal resection?
Esophageal mucosal resection: The doctor lifts the damaged tissue, injects a solution underneath to act as a cushion, and removes the affected tissue using a snare or suction cup.
What is the best treatment for GERD?
Rabeprazole (AcipHex) Esomeprazole (Nexium) Dexlansoprazole (Dexilant) If GERD symptoms don't respond to medication or if the patient has high-grade dysplasia, the doctor may recommend an endoscopic procedure to remove or destroy the abnormal cells or dysplasia. The approach depends on the patient and how far the Barrett's esophagus has progressed.
What is Barrett's esophagus?
Barrett's esophagus is a potentially serious complication of GERD, which stands for gastroesophageal reflux disease. In Barrett's esophagus, normal tissue lining the esophagus -- the tube that carries food from the mouth to the stomach -- changes to tissue that resembles the lining of the intestine. About 10% of people with chronic symptoms of GERD ...
What are the risk factors for Barrett's esophagus?
Risk factors include age over 50, male sex, white race, hiatal hernia, long standing GERD, and overweight, especially if weight is carried around the middle.
How to prevent acid reflux in stomach?
Sleep with the head of the bed elevated. Sleeping with your head raised may help prevent the acid in your stomach from flowing up into the esophagus.
Can Barrett's esophagus be diagnosed with a biopsy?
How Is Barrett's Esophagus Diagnosed? Because there are often no specific symptoms associated with Barrett's esophagus, it can only be diagnosed with an upper endoscopy and biopsy.
Is Barrett's esophagus cancer rare?
It does, though, increase the risk of developing esophageal adenocarcinoma, which is a serious, potentially fatal cancer of the esophagus. Although the risk of this cancer is higher in people with Barrett's esophagus, the disease is still rare. Less than 1% of people with Barrett's esophagus develop this particular cancer.
Does GERD cause Barrett's esophagus?
With GERD, stomach contents flow backward into the esophagus. This is known as reflux. Most people with acid reflux don't develop Barrett's esophagus.
Can anyone develop Barrett's esophagus?
And not everyone with Barrett's esophagus has GERD. But long-term GERD is the primary risk factor. Anyone can develop Barrett's esophagus, but white males who have had long-term GERD are more likely than others to develop it .
What is Barrett's esophagus attributed to?
The development of Barrett's esophagus is most often attributed to long-standing GERD, which may include these signs and symptoms:
How long do you have to wait to see a doctor about Barrett's esophagus?
If you've had trouble with heartburn, regurgitation and acid reflux for more than five years, then you should ask your doctor about your risk of Barrett's esophagus.
What is the valve between the esophagus and the stomach called?
Between the esophagus and the stomach is a critically important valve, the lower esophageal sphincter (LES). Over time, the LES may begin to fail, leading to acid and chemical damage of the esophagus, a condition called gastroesophageal reflux disease (GERD). GERD is often accompanied by symptoms such as heartburn or regurgitation.
What causes the lining of the esophagus to thicken?
Barrett's esophagus is a condition in which the flat pink lining of the swallowing tube that connects the mouth to the stomach (esophagus) becomes damaged by acid reflux, which causes the lining to thicken and become red. Between the esophagus and the stomach is a critically important valve, the lower esophageal sphincter (LES).
What are the factors that increase the risk of Barrett's esophagus?
Factors that increase your risk of Barrett's esophagus include: Family history. Your odds of having Barrett's esophagus increase if you have a family history of Barrett's esophagus or esophageal cancer. Being male. Men are far more likely to develop Barrett's esophagus. Being white.
Can Barrett's esophagus cause cancer?
Fortunately, most people with Barrett's esophagus will never develop esophageal cancer. By Mayo Clinic Staff. Barrett's esophagus care at Mayo Clinic.
Does acid reflux cause Barrett's esophagus?
Whether this acid reflux is accompanied by GERD symptoms or not, stomach acid and chemicals wash back into the esophagus, damaging esophagus tissue and triggering changes to the lining of the swallowing tube, causing Barrett's esophagus.
What is Barrett's esophagus?
Barrett's esophagus is a complication of chronic gastroesophageal reflux disease (GERD), primarily in white men . GERD is a disease in which there is reflux of acidic fluid from the stomach into the esophagus (the swallowing tube). GERD most commonly causes heartburn. There are two requirements for the diagnosis of Barrett's esophagus.
Why is Barrett's esophagus so important?
The reason for the great interest in Barrett's esophagus is that it is associated with an increased risk of cancer of the esophagus. The type of cancer that occurs in patients with Barrett's is adenocarcinoma, which arises from the metaplastic intestinal tissue.
How to treat GERD without esophagus?
GERD, with or without the presence of Barrett's esophagus, sometimes is treated by anti-reflux surgery. This operation, called fundoplication, is done to stop the reflux of acid. Fundoplication is not done for Barrett's esophagus itself. The operation involves wrapping the upper stomach (the fundus) around the lower end of the esophagus. The purpose of the wrap is to tighten the lower esophageal sphincter (LES) in order to prevent the reflux of stomach contents into the esophagus. There is no evidence that anti-reflux surgery, or for that matter, acid suppression therapy with drugs, decreases the risk of esophageal cancer among patients with Barrett's. This doesn't mean that the possibility is not affected, but it would take long-term studies to prove that either medical or surgical treatment decreases the risk of cancer, and such studies are not likely to be done.
What type of cells are in Barrett's esophagus?
They pointed out that Barrett's esophagus consisted of a metaplasia in which the normal cells lining the esophagus were replaced by a mixture of gastric and intestinal lining cells. The intestinal-type lining cells also are called specialized columnar cells which include goblet cells.
Why does my esophagus narrow?
A stricture or narrowing is due to scarring (fibrosis) of the esophagus that may cause difficulty in swallowing ( dysphagia ). The dysphagia is sensed as a sticking (stopping) of solid food in the chest (in the esophagus), and liquids when the narrowing is severe.
Why is Barrett's esophagus a protective response?
This transformation, called metaplasia, is believed to be a protective response because the specialized columnar epithelium (epithelium means lining) in Barrett's esophagus is more resistant to injury from acid than the squamous epithelium.
How far up the esophagus is the pink lining?
The diagnosis of Barrett's esophagus rests upon seeing (at endoscopy) a pink esophageal lining that extends a short distance (usually less than 2.5 inches) up the esophagus from the gastroesophageal junction and finding intestinal type cells (goblet cells) on biopsy of the lining.
How to treat Barrett's esophagus?
DOs and DON’Ts in Managing Barrett’s Esophagus: 1 DO remember that the only way to diagnose the disorder is by tissue biopsy via endoscopy. A gastroenterologist (a specialist who treats diseases of the stomach and bowel) will do this. 2 DO remember that acid reflux tends to occur more frequently at night when you lie flat. Elevating the head of the bed will help. 3 DO lose weight. 4 DO make lifestyle changes and take medicines to lower your risk of getting Barrett’s esophagus. 5 DO call your health care provider if you have heartburn that medicine doesn’t help, food gets stuck in your throat and you throw up, or you have trouble swallowing and lose weight. 6 DO call your health care provider if you vomit blood.
How to diagnose a bowel disorder?
DO remember that the only way to diagnose the disorder is by tissue biopsy via endoscopy. A gastroenterologist (a specialist who treats diseases of the stomach and bowel) will do this.

Diagnosis
Treatment
Clinical Trials
Lifestyle and Home Remedies
Specialist to consult
Preparing For Your Appointment