There is no cure for chronic pancreatitis, but the related pain and symptoms may be managed or even prevented. Since chronic pancreatitis is most often caused by drinking, abstinence from alcohol is often one way to ease the pain. The following drugs are prescribed for pain relief: Acetaminophen and ibuprofen
Full Answer
What is the life expectancy of someone with pancreatitis?
- Severe abdominal pain (just below the ribs)
- Diabetes (a condition which can culminate into a symptom for chronic pancreatitis)
- Nausea and vomiting
- Poor digestion of fats and vitamins
How long will I live with chronic pancreatitis?
Though a life-threatening disorder, chronic pancreatitis life expectancy can range from 5 to 60 years with proper medication and treatment. Pancreas is an important organ that aids in digestion of fats and helps in metabolism of the body by regulating insulin levels.
How long does it take to recover from pancreatitis?
In 80% of people with acute pancreatitis, the inflammation either clears up completely or improves a lot within one to two weeks. But it sometimes leads to serious complications, so it’s usually treated in a hospital. Acute pancreatitis usually clears up within one to two weeks. Solid foods are generally avoided for a while in order to reduce the strain on the pancreas.
What are some natural remedies for pancreatitis?
Natural Ways To Help With Pancreatitis
- Blueberries. The presence of free radicals can aggravate or bring about pancreatitis. ...
- Tofu. Switching to tofu-based meals is a popular meat alternative for people, particularly those who suffer from chronic pancreatitis.
- Ginseng. ...
- Acupuncture. ...
- Yogurt. ...
- Reishi Mushrooms. ...
- Spinach. ...
- Coconut Oil. ...
- Red Grapes. ...
- Cut Out Sugar. ...
Will there ever be a cure for chronic pancreatitis?
There is no cure for chronic pancreatitis, but the related pain and symptoms may be managed or even prevented. Since chronic pancreatitis is most often caused by drinking, abstinence from alcohol is often one way to ease the pain.
What happens if chronic pancreatitis is not treated?
Without proper care, chronic pancreatitis can lead to serious problems, such as severe pain and malnutrition. Over the long term, people with this condition are at risk for developing diabetes and pancreatic cancer.
What is the newest treatment for chronic pancreatitis?
EUS-guided celiac plexus block (CPB) or celiac plexus neurolysis (CPN) is used to reduce the extremely disabling pain associated with chronic pancreatitis or pancreatic cancer. CPB is a temporizing treatment, most commonly injection of a local anesthetic together with a corticosteroid.
Can you live a long life with chronic pancreatitis?
However, up to 80 percent of people with chronic pancreatitis will have a life expectancy of at least 10 years after the initial diagnosis.
What is the most common complication of chronic pancreatitis?
The most common complications of chronic pancreatitis are pseudocyst formation and mechanical obstruction of the duodenum and common bile duct.
Is pancreatitis always fatal?
About 4 out of 5 cases of acute pancreatitis improve quickly and don't cause any serious further problems. However, 1 in 5 cases are severe and can result in life-threatening complications, such as multiple organ failure. In severe cases where complications develop, there's a high risk of the condition being fatal.
Can chronic pancreatitis go into remission?
The changes of chronic pancreatitis are not reversible. However, it is possible to have control of pain and steatorrhea with medical, endoscopic, percutaneous or surgical treatment.
Does chronic pancreatitis hurt all the time?
Acute pancreatitis causes severe, unrelenting pain that often sends patients to the emergency department. In chronic pancreatitis, pain may be dull, continual or episodic with relation to eating, and it may change or even disappear over time.
What can trigger chronic pancreatitis?
What causes chronic pancreatitis?An attack of acute pancreatitis that damages your pancreatic ducts.A blockage of the main pancreatic duct caused by cancer.Certain autoimmune disorders.Cystic fibrosis.Hereditary diseases of the pancreas.Smoking.Unknown cause in some cases.
Can chronic pancreatitis live 20 years?
Prognosis of chronic pancreatitis The 10-year survival rate was 70%, the 20-year survival rate 45%, compared with 93% and 65%, respectively, in patients without pancreatitis.
Are there stages of chronic pancreatitis?
On the basis of the results of these studies it is proposed that alcoholic chronic pancreatitis be divided into four stages: I) latent or subclinical, II) early, or stage of inflammatory complications, III) late, or stage of severe pancreatic insufficiency, and IV) advanced, or stage of secondary painless pancreatitis.
Can you get better from pancreatitis?
Most people with acute pancreatitis get better within a week and are well enough to leave hospital after a few days. Recovery can take longer in severe cases, as some people can develop complications. Read more about treating acute pancreatitis and the possible complications of acute pancreatitis.
How Is Acute Pancreatitis Treated?
Cases of moderate and severe acute pancreatitis are treated in the hospital. Visits should only last a few days. Doctors will administer blood and...
How Is Chronic Pancreatitis Treated?
There is no cure for chronic pancreatitis, but the related pain and symptoms may be managed or even prevented. Since chronic pancreatitis is most o...
How Is Severe Pancreatitis Treated?
About 20 percent of pancreatitis cases are severe, meaning they result in multiple organ failure that doesn't naturally subside within 48 hours. (3...
How Are Pancreatitis Complications Treated?
Antibiotics may also be necessary if an extra-pancreatic (outside of the pancreas) infection has developed.Up to one-third of people with pancreati...
How Do You Manage Pancreatitis at Home?
In addition to hospital treatment, the following lifestyle changes are recommended to help aid recovery and possibly prevent pancreatitis: 1. Drink...
What Is A Pancreatic Diet?
There is no one specific pancreatic diet that can treat chronic pancreatitis.But there are some general rules for nutrition if you have the conditi...
Why does my pancreas hurt?
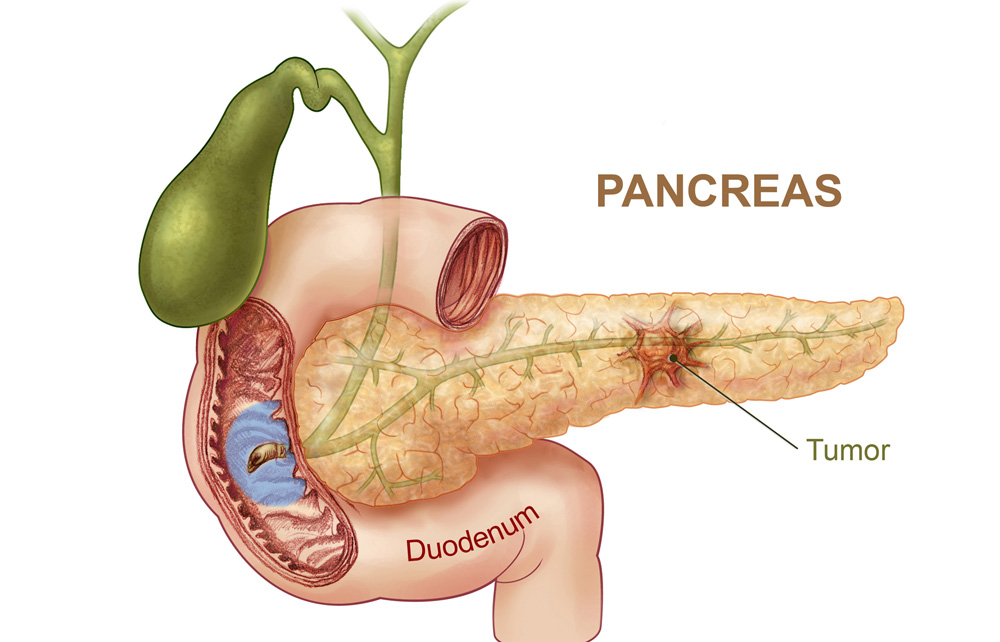
It's long been thought that an inflamed head of the pancreas or a blocked pancreatic duct causes the pain. In cases where doctors believe that to be the problem, surgery will be performed to remove the head of the pancreas.
How to treat pancreatitis in the hospital?
In addition to hospital treatment, the following lifestyle changes are recommended to help aid recovery and possibly prevent pancreatitis: 1 Drink plenty of water 2 Stop or reduce alcohol consumption 3 Stop smoking, because the habit increases your risk of pancreatitis 4 Refrain from eating foods high in fat
How long does a pancreatitis visit last?
Cases of moderate and severe acute pancreatitis are treated in the hospital. Visits should only last a few days. Doctors will administer blood and imaging tests to diagnose you, and then begin care. Because of the loss of fluids from vomiting and decreased food intake, the initial treatment for pancreatitis is hydration using intravenous (IV) ...
What is the procedure called when the pancreas is removed?
During this procedure, known as autologous islet cell transplantation, the entire pancreas is removed and the insulin-making cells of the pancreas are reinserted into the liver with a catheter. When the transplant is successful, it allows patients to make insulin without the pancreas.
What is the most common symptom of pancreatitis?
There are varying severities of the condition, but abdominal pain, nausea, and vomiting are among the most common symptoms of both acute and chronic pancreatitis.
How to help pancreatitis?
In addition to hospital treatment, the following lifestyle changes are recommended to help aid recovery and possibly prevent pancreatitis: Drink plenty of water. Stop or reduce alcohol consumption. Stop smoking, because the habit increases your risk of pancreatitis. Refrain from eating foods high in fat.
Can gallstones cause pancreatitis?
Gallstones are the number one cause of pancreatitis. For the majority of these cases, the gallstones are small and don't remain in the bile duct or pancreatic duct for long.
What is the name of the inflammation of the pancreas that doesn't improve over time?
Chronic pancreatitis is an inflammation of your pancreas that doesn’t improve over time. The pancreas is an organ located behind your stomach. It makes enzymes, which are special proteins that help digest your food. It also makes hormones that control the level of sugar in your bloodstream. Pancreatitis occurs when your pancreas becomes inflamed.
How to treat pancreatitis?
Treatment for pancreatitis can include medication, endoscopic therapies, or surgery.
What is the name of the disease that causes a narrow pancreatic duct?
Inflammatory bowel syndrome, which is inflammation of the digestive tract, and primary biliary cholangitis, which is a chronic liver disease associated with chronic pancreatitis. autoimmune disease, which occurs when your body mistakenly attacks your healthy cells and tissues. a narrow pancreatic duct, which is the tube ...
What age do you get chronic pancreatitis?
Chronic pancreatitis most frequently develops in people between the ages of 30 and 40. The condition is also more common among men than women. Children living in tropical regions of Asia and Africa may be at risk for developing tropical pancreatitis, which is another type of chronic pancreatitis.
What is the name of the disease that causes mucus to build up in the lungs?
a narrow pancreatic duct, which is the tube that carries enzymes from the pancreas to the small intestine. cystic fibrosis, which is a hereditary disease that causes mucus to build up in your lungs. a high level of triglyceride fats in your blood, which is called hypertriglyceridemia.
How to check for inflammation in the abdomen?
Your doctor might request that the following studies be done on your abdomen to look for signs of inflammation: Your doctor may also recommend an endoscopic ultrasound. During an endoscopic ultrasound, your doctor inserts a long, flexible tube into your mouth and down through the stomach and small intestine.
What causes pancreatitis?
There are numerous different causes of chronic pancreatitis. The most common cause is long-term alcohol abuse. Approximately 70 percent of cases are linked to alcohol consumption. Autoimmune disease occurs when your body mistakenly attacks your healthy cells and tissues.
What is the pancreas that controls blood sugar?
This is because the pancreas contains Islets of Langerhans — also known as islets or islet cells — that regulate the body's blood sugar levels. UCSF's Islet and Cellular Transplantation Center is one the few medical centers in the country to offer a total pancreatectomy performed with an islet autotransplant.
How much insulin dependent is a pancreatectomy?
Patients who have a pancreatectomy with an islet autotransplant have a 50 percent chance of becoming insulin dependent for life, while patients who have only a pancreatectomy have a 100 percent chance of becoming permanently insulin dependent.
What is the difference between a partial and total pancreatectomy?
A partial pancreatectomy involves removing part of the pancreas, such as the body or tail, during a Puestow or Whipple procedure. A total pancreatectomy involves removing the entire pancreas. While a total pancreatectomy is usually effective in relieving pain in patients when all other treatments fail, it induces permanent diabetes, requiring patients to take insulin shots or use an insulin pump for the rest of their lives. This is because the pancreas contains Islets of Langerhans — also known as islets or islet cells — that regulate the body's blood sugar levels.
Why is there no guarantee that diabetes will not develop?
While the goal is to eliminate each patient's pain, preserve their pancreatic function and prevent diabetes, there is no guarantee that diabetes will not develop because there is no way of determining the quality of a patient's islets before transplantation.
How to treat chronic pancreatitis?
Treatment of chronic pancreatitis depends on the cause of the disease, severity of the associated pain and effectiveness of former treatment approaches. The first step of treatment focuses on relieving pain and eating a diet that is high in carbohydrates and low in fat. It is essential to stop drinking alcohol ...
Can you have an islet auto after a pancreatitis?
Pancreatectomy and Islet Autotransplant. Patients with chronic pancreatitis have the option of having an islet auto (meaning "self") transplant after their total pancreatectomy.
What causes pancreatitis in Western societies?
The most common cause of chronic pancreatitis in Western societies is alcohol. Alcohol consumption has been implicated in approximately 70 percent of cases as a major cause of this disease. Other causes include gallbladder disease, hyperparathyroidism (increased secretion from the parathyroid glands) and trauma to the pancreas. ...
What is the cause of elevated blood glucose levels?
Diabetes mellitus is a disorder of carbohydrate metabolism characterized by inadequate secretion or utilization of insulin, resulting in elevated blood glucose levels. Chronic pancreatitis affects the endocrine function of the pancreas, responsible for insulin and glucagon production. Diabetes is common in patients with chronic pancreatitis, ...
What is a stent in a sphincter?
A stent, or endoprosthesis, is a hollow synthetic tube that may be inserted in a pancreatic or biliary duct or sphincter to facilitate flow of pancreatic juice or bile. Endoscopic sphincterotomy refers to the division of a muscle during endoscopy.
What is the treatment for pancreatitis?
Treatment for chronic pancreatitis includes medical, endoscopic and surgical therapy. Pancreatic enzyme replacement is therapy that replaces enzymes, the production of which is reduced because of the disease process of pancreatitis. The goal of pancreatic enzyme replacement therapy is to control diarrhea and help the patient stabilize his/her body ...
What is the term for an episode of abdominal pain accompanied by elevations in blood enzyme levels?
Acute pancreatitis is an isolated episode of abdominal pain accompanied by elevations in blood enzyme levels. Essentially, it describes active inflammation of the pancreas. More than 80 percent of the cases of acute pancreatitis are related to biliary stones or alcohol use. Acute pancreatitis may lead to chronic pancreatitis.
What is the cause of pancreatitis in children?
Its cause is unknown, although malnutrition is suspected to play a role. Several major physiological factors contribute to the development of chronic pancreatitis in alcoholic patients.
What are the complications of chronic pancreatitis?
Nutrient malabsorption, diabetes mellitus and splenic vein thrombosis are common complications of chronic pancreatitis. Malabsorption is faulty absorption of nutrients from the digestive tract. In chronic pancreatitis, malabsorption occurs after the capacity for enzyme secretion is reduced by more than 90 percent.
Why do I have pale stools?
The weight loss occurs because the body does not secrete enough pancreatic enzymes to digest food, so nutrients are not absorbed normally, leading to malnutrition.
What causes chronic pancreatitis?
Whereas there are causes of chronic pancreatitis that are unknown; several factors have been identified to cause chronic pancreatitis: Heavy alcohol use. Autoim mune conditions (when the body’s immune system attacks its own body) Genetic mutations due to cystic fibrosis.
Does pancreatitis cause pain in the back?
Symptoms of Chronic Pancreatitis. Most individuals with chronic pancreatitis experience upper abdominal pain, although some have no pain at all. The pain may spread to the back, become worse with eating or drinking, and become constant and disabling.