Lithium carbonate is a well documented cause of nephrogenic diabetes insipidus, with as many as 10 to 15% of patients taking lithium developing this condition. Clinicians have been well aware of lithium toxicity for many years; however, the treatment of this drug-induced condition has generally been remedied by discontinuation of the medication or a reduction in dose. For those patients unresponsive to traditional treatment measures, several pharmacotherapeutic regimens have been documented as being effective for the management of lithium-induced diabetes insipidus including hydrochlorothiazide This medication is used to treat high blood pressure.Hydrochlorothiazide
Can lithium cause nephrogenic diabetes insipidus?
Background: Lithium can cause nephrogenic diabetes insipidus in up to 20 to 40 percent of patients currently taking the medication, and a subset of these patients will have a persistent concentrating defect long after lithium is discontinued. They are at risk for serious hypernatremia when fluid intake is restricted for any reason.
What is the prognosis of lithium induced di?
Lithium induced DI is believed to be dependent on the dose of the medication. In some cases, the symptoms can be reduced or eliminated by using the lowest effective medication dose. If improvements are seen, then function tests will be conducted 2x per year to make sure the lithium regimen is still functioning properly.
How is Dialysis used to treat lithium intoxication?
Hemodialysis is one of the methods which can be used in the treatment of lithium intoxication, and is used especially for patients in whom the lithium concentration is over 3.5 mEq/L or those with concomitant renal failure, heart failure, and pulmonary edema.
Is there a need for novel treatments for lithium-induced non-drug induced diabetic ketoacidosis?
However, these drugs have been associated with acute lithium-level elevations of up to 33–50%, which could increase the risk of acute central nervous system and renal toxicity [ 19, 20 ]. Therefore, there is a need for novel, well-tolerated treatments for lithium-induced NDI.
How is nephrogenic DI treated?
Nephrogenic diabetes insipidus. Instead, your doctor may prescribe a low-salt diet to reduce the amount of urine your kidneys make. You'll also need to drink enough water to avoid dehydration. Treatment with the drug hydrochlorothiazide (Microzide) may improve your symptoms.
How is lithium induced polyuria treated?
Polyuria can be treated with medications, such as diuretics and nonsteroidal anti-inflammatory drugs (NSAIDs; see Medication). The potassium-sparing diuretic amiloride is the most established therapy for the polyuria associated with lithium use.
Is lithium induced nephrogenic diabetes insipidus reversible?
Lithium induced nephrogenic diabetes insipidus is considered to be reversible on cessation of therapy but polyuria persisted in this patient for ten years after lithium was stopped.
Is lithium induced Di reversible?
Lithium-induced nephrogenic diabetes insipidus is usually reversible on stopping therapy but a few patients remain symptomatic long after the lithium has been discontinued [12] (a case of persistent nephro- genic diabetes insipidus has been reported 8 years after discontinuation of lithium [13]).
How is lithium-induced diabetes insipidus treated?
Amiloride, thiazide diuretics, indomethacin and desmopressin have all been used to successfully treat lithium-induced DI.
Which drug is used in lithium-induced diabetes insipidus?
Vasopressin, amiloride and thiazide diuretics have been used in lithium-induced nephrogenic diabetes insipidus treatment. Acetazolamide might be an option to treat lithium-induced nephrogenic diabetes insipidus patients who fail to respond to standard treatment.
Is nephrogenic diabetes insipidus curable?
There's no cure for diabetes insipidus. But treatments can relieve your thirst and decrease your urine output and prevent dehydration.
Can lithium damage your kidneys?
Lithium may cause problems with kidney health. Kidney damage due to lithium may include acute (sudden) or chronic (long-term) kidney disease and kidney cysts. The amount of kidney damage depends on how long you have been taking lithium.
What is the drug of choice for lithium-induced diabetes insipidus when lithium must be continued?
Clinicians have been aware of lithium toxicity for many years and traditionally have administered thiazide diuretics for lithium-induced polyuria and nephrogenic diabetes insipidus. Recently, amiloride, a potassium-sparing diuretic, has been reported as a successful treatment for nephrogenic diabetes insipidus.
How is lithium induced diabetes insipidus diagnosed?
Diagnosing lithium-induced nephrogenic diabetes insipidus (NDI) begins with a history of the patient's symptoms and ordering lab tests. The next step involves a water restriction test, also known as a thirst test, to measure the patient's ability to concentrate his or her urine.
How is lithium excreted?
Lithium is excreted almost entirely by the kidneys (2). Lithium is freely filtered by the glomerulus since it is not bound to serum proteins (2). In the proximal tubule, lithium is handled similarly to sodium (2).
What are the symptoms of nephrogenic diabetes insipidus?
The two main symptoms of NDI are chronic excessive thirst (polydipsia) and excessive urine production (polyuria). Excessive urination at night (nocturia) also occurs. Some infants may present with vomiting, retching, unexplained fevers, lethargy, and irritability. Constipation, diarrhea and poor feeding may also occur.
Is lithium related to diabetes?
Certainly, a number of patients have varying degrees of persistent lithium-related nephrogenic diabetes insipidus. Although pathologic changes are associated with persistent nephrogenic diabetes insipidus, the exact mechanism of the persistent defect is unknown.
Is lithium a risk factor for hypernatremia?
They are at risk for serious hypernatremia when fluid intake is restricted for any reason. Methods: MEDLINE as used to search the key words "nephrogenic diabetes insipidus" and "lithium" from 1990 to the present. A case report describes a patient who had been off lithium for 8 years and who developed hypernatremia after she was transferred ...
Can lithium cause diabetes?
Background: Lithium can cause nephrogenic diabetes insipidus in up to 20 to 40 percent of patients currently taking the medication, and a subset of these patients will have a persistent concentrating defect long after lithium is discontinued. They are at risk for serious hypernatremia when fluid intake is restricted for any reason.
What happens if you take lithium?
At lithium concentrations greater than 3 mmol/L, patients may progress to seizures, coma, and irreversible brain damage. Diabetes insipidus is a condition marked by polyuria caused by an inability of the kidneys to resorb free water. There are various causes of diabetes insipidus, which can be further classified into central and nephrogenic subgroups. Central diabetes insipidus is characterized by injury to the neurohypophysial system and is often the result of hypoxic encephalopathy, iatrogenic injury to the pituitary gland during surgical procedures, and autoimmune attack on vasopressin-producing cells in the hypothalamus. Nephrogenic diabetes insipidus is also characterized by an inability of the kidneys to respond to adequate levels of vasopressin, often the result of chronic lithium use, which injures the collecting ducts of the kidneys.6It is also characterized by polydipsia, polyuria, and an inability to concentrate urine, and results from unresponsiveness of the kidneys to the effects of antidiuretic hormone. Polyuria, polydipsia, and nephrogenic diabetes insipidus are frequent complications of treatment with lithium, and may be present shortly after starting treatment.
Where does lithium accumulate in the kidney?
Lithium accumulates in the distal tubular cells of the kidneys at concentrations 10–20 times higher than in serum, and at toxic serum concentrations is associated with degenerative changes and necrosis of the tubular cells. Chronic treatment with lithium commonly produces a defect in the concentrating ability of the kidney due to inhibition of generation of cyclic adenosine monophosphate by antidiuretic hormone at the distal tubule, with lithium probably acting via adenylate cyclase and possibly also at a point distal to the generation of cyclic adenosine monophosphate. About 30%–90% of patients show lowered maximum urine osmolality.7
What is lithium salt used for?
Lithium salts have been used in clinical practice since the 1970s. Widely used in the treatment and prophylaxis of bipolar disorder, lithium has a very narrow therapeutic index and toxicity is common in patients taking this agent. The effects of lithium on the kidney, thyroid, and parathyroid causes changes in body weight and the skin, and causes congenital malformations. Although often used to treat patients with a range of mood disorders, lithium has been associated with several forms of renal injury, the most prevalent of which is impaired urinary concentrating ability, which is estimated to be present in at least 50% of individuals on chronic lithium therapy. Drug-induced diabetes insipidus is almost always of the nephrogenic type. Lithium is the most common drug implicated.1
How much urine output increased after 24 hours of hemodialysis?
The patient’s urine output increased with 24 hours of hemodialysis (11,000 mL /24 hours). Laboratory findings at that time were as follows: blood urea nitrogen 14 mg/dL, creatinine 0.9 mg/dL, sodium 159 mmol/L, plasma osmolality 329 mOsm/L, and urine density 1005, so the patient was thought to have developed diabetes insipidus, and desmopressin was started at 6 μg three times daily via subcutaneous injection.
Can desmopressin be used for lithium intoxication?
The clinician is also reminded that nephrogenic diabetes insipidus due to lithium intoxication may respond to treatment with desmopressin as well as thiazides, amiloride, and nonsteroidal anti-inflammatory drugs. More studies are needed about the use of desmopressin in the treatment of nephrogenic diabetes insipidus due to lithium intoxication.
Is lithium toxic to the kidneys?
Lithium has a narrow therapeutic index, so a large proportion of patients on chronic lithium therapy experience at least one episode of toxicity during treatment. The highest intracellular lithium levels are found in the brain and the kidneys. Nephrogenic diabetes insipidus is the most common renal side effect of lithium.2Although nephrogenic diabetes insipidus may persist, acute renal toxicity is temporary. However, patients with severe lithium intoxication have shown persistent cerebellar damage with, for example, tremor, ataxia, and dysarthria, and persisting basal ganglia problems have also been described. The clinician should determine the severity of the intoxication from the history and serial lithium levels. In chronic use, nephrogenic diabetes insipidus often becomes irreversible. In one study, patients who had been on lithium for more than 18 years invariably had an irreversible defect.3
Where is lithium filtered?
Lithium is filtered completely at the glomerulus and absorbed in the proximal tubule, so the clearance of lithium is approximately 30% of creatinine clearance. Its predominant toxicity is at the distal tubule and is related partially to effects on inhibition of adenylate cyclase and generation of cyclic adenosine monophosphate. This inhibition promotes accumulation of glycogen, so glycogen can be seen clearly in the distal tubules on renal biopsy. Deposition of glycogen causes tubular dysfunction, and later, tubule loss and scarring can be seen. At doses in the toxic range, the proximal tubules may also be affected. Therefore, low-dose (and usually chronic) toxicity is associated with distal tubular abnormalities, and high-dose toxicity characteristically manifests as proximal tubular damage, when a prerenal effect is often also seen.
How old are people who have lithium?
The mean age per episode was 63.4 [standard deviation (SD) 18.9] and the median 69 years. The age ranged from 19 to 93 years. A total of 59% of episodes related to patients aged 65 years or older. In 42% of episodes, patients had been exposed to lithium at some point, either currently (28%) or in the past (14%) (Table 1).
Is lithium good for bipolar?
Lithium remains the first-line maintenance treatment for bipolar affective disorder (BPAD).1It is also used as augmentation of antidepressant medication and as a mood stabilizer in the treatment of schizoaffective disorder. Only recently has lithium been endorsed as superior in the prevention of suicide and severe affective episodes.2,3Yet, despite its therapeutic superiority and versatility, adverse effects limit lithium use in clinical practice. Over half of all patients may discontinue lithium at some time, and adverse effects are the most common reason for discontinuation.4
Does lithium cause renal failure?
Lithium is associated with an increased risk of loss of renal function .5,6Whereas glomerular damage appears only after years of lithium treatment, tubular dysfunction may emerge within weeks after lithium initiation.7Tubular dysfunction leads to urine concentration deficits and subsequently polyuria. Later on, this may progress to nephrogenic diabetes insipidus (NDI),8where tubular cells have lost their ability to respond to vasopressin [antidiuretic hormone (ADH)]. Up to 20–40% of patients treated with lithium may experience NDI.8,9It remains unclear whether NDI is reversible once lithium has been stopped.
Is lithium a risk factor for hypernatraemia?
In this study, we tested the hypothesis that lithium treatment was a risk factor for hyperna traemia.
Is NDI a contributing factor?
We also evaluated NDI as a major contributing factor for hypernatraemia. Here, we considered both confirmed and suspected NDI. NDI was considered confirmed when either the diagnosis had been established or urine osmolality was inadequately low in relation to plasma osmolality or suspected when polyuria and/or polydipsia (polyuria–polydipsia complex) was explicitly recorded in the medical records.
What is lithium used for?
It is particularly useful when treating conditions such as bipolar disorder.
Why do people take lithium once a day?
Sometimes a switch to once-per-day lithium will also provide improvements. This is because it gives the kidneys a longer time of being away from the drug. Some patients who require the levels of lithium for therapeutic purposes may find relief from their diabetes insipidus through the use of certain diuretics.
Why is a lithium urine test important?
This test is important because it helps to track the overall severity of the disease.
How often should I do a lithium saturation test?
If improvements are seen, then function tests will be conducted 2x per year to make sure the lithium regimen is still functioning properly. Lithium saturation tests may be ordered 2x per week during the stabilization period so that issues may be quickly identified.
Can you use thiazide with lithium?
Thiazide diuretics may also be used, but may also require a 50% or greater reduction in lithium medication, so it may not be suitable for everyone . NSAID medications in combination with diuretics have also been found to be effective in urine concentration increases.
Does lithium affect kidney function?
When lithium is used for an extended period of time, it will desensitize or reduce the ability of the kidney to respond to the ADH that is being produced by the body. This means the kidneys stop listening to the hormones, which is a trademark sign of nephrogenic diabetes insipidus.
Can lithium cause fatigue?
Lithium induced diabetes insipidus will typically first be discovered on a routine checkup or walk-in appointment, either at the doctor’s office or with the individual’s psychiatrist. The most common complaint is an increased level of thirst, but there may also be unusual daytime fatigue, problems sleeping at night, and even muscle tremors.
What is the effect size of statins on NDI?
In our previous cross-sectional findings in chronic lithium users, the effect size of statins on NDI was 0.33 [ 21 ], however that was not an intervention study. We acknowledge that there is relatively little data at the current time to justify the sample size. This RCT will provide the necessary and adequate data to plan a subsequent larger RCT [ 39 ].
What is the grant number for the Kidney Foundation of Canada?
This study is supported by a biomedical research grant from the Kidney Foundation of Canada (KFoC). Grant number: KFOC170016.
Does lithium cause CKD?
The exact mechanism whereby lithium causes CKD is not known. The most prominent pathology seen in patients with CKD attributed to lithium is interstitial nephropathy [ 15 ]. This points to a potential link between lithium related NDI and CKD. NDI is characterized by excessive production of dilute urine (> 3 L/24 h) due to tubular resistance to antidiuretic hormone [ 16 ]. Half of lithium users have difficulty concentrating urine: e.g. urine osmolality (UOsm) < 600 mOsm/kg following overnight water restriction [ 15 ]. Lithium-induced NDI is problematic: in addition to being related to frequent AKI and hypernatremia [ 17 ], NDI is also associated with a 2–3 times increased risk of chronic kidney disease (CKD) [ 12, 17 ]. Thus, treating lithium-induced NDI could potentially help prevent CKD.
Is lithium safe for bipolar?
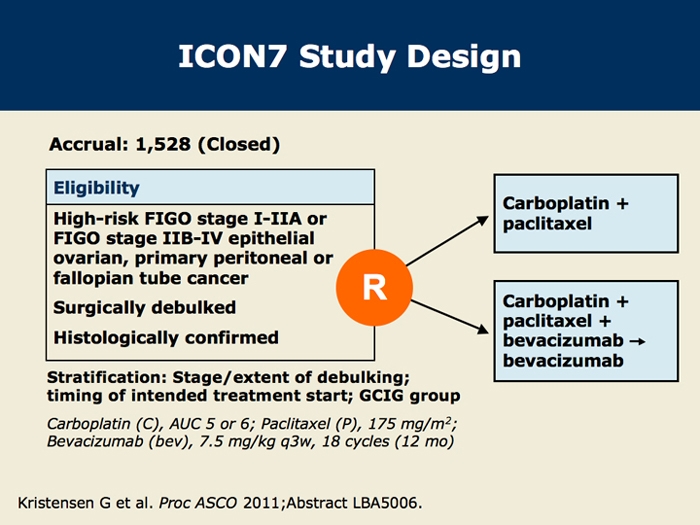
Lithium is the gold-standard treatment for bipolar disorder, is highly effective in treating major depressive disorder, and has anti-suicidal properties. However, clinicians are increasingly avoiding lithium largely due to fears of renal toxicity. Nephrogenic Diabetes Insipidus (NDI) occurs in 15–20% of lithium users and predicts a 2–3 times increased risk of chronic kidney disease (CKD). We recently found that use of statins is associated with lower NDI risk in a cross-sectional study. In this current paper, we describe the methodology of a randomized controlled trial (RCT) to treat lithium-induced NDI using atorvastatin.
Does lithium cause kidney disease?
Rej S, Herrmann N, Shulman K, Fischer HD, Fung K, Harel Z, Gruneir A. Lithium use, but not valproate use, is associated with a higher risk of chronic kidney disease in older adults with mental illness. J Clin Psychiatry. 2017;78 (8):e980–5.
Is lithium good for mood disorders?
Lithium is valuable considering the difficulty in achieving and maintaining symptomatic remission in the majority of patients with mood disorders [ 6 ]. Furthermore, lithium responders often do not respond well to alternative pharmacotherapies [ 5 ].
Is lithium good for depression?
Lithium is also effective in treatment-resistant depression [ 1 ], has been associated with reduced suicidality [ 3 ], and is even being investigated in a number of neurological conditions such as dementia and stroke [ 4, 5 ].
How does lithium affect the kidneys?
Lithium reduces the ability of the kidneys to reabsorb body water flowing through the kidney collecting ducts. This unabsorbed body water is voided as dilute urine. So much body water is voided in this manner that the patient would suffer from dehydration if he or she did not have ready access to drinking water. To better understand how lithiuminterferes with the water reabsorption (and resulting urine concentration) process it helps to know the molecular sequence that underlies it.
What is the treatment for polyuria?
Clinicians generally prescribe thiazide diuretics or amiloride, a potassium-sparing diuretic. Lithium concentration in the blood should be measured after the introduction of diuretic compounds because there is a risk of increased lithium reabsorption by the kidney. Sometimes clinicians prescribe a combination of both of these medicines. These diuretics take a little while to begin working. In emergency situations, clinicians may administer indomethacin, a prostaglandin synthesis inhibitor. It is not, however, recommended for long-term use.
What is NDIF website?
The Nephrogenic Diabetes Insipidus Foundation (NDIF) is dedicated to informing and helping the NDI community. The authors of the information archived on the NDIF website, and the archivists, cannot be held responsible for any damage which may result from using the information on this site without concurrence of your medical doctor. Consult your personal physician for your individual medical needs.
Does lithium decrease cAMP?
Animal studies have shown that lithium decreases cAMP concentration by blocking the activation of adenylyl cyclase. Lithium may also decrease cAMP levels by increasing its destruction by phosphodiesterase. Lithium has been shown to increase the ability of AVP to produce prostaglandin E2 in the kidney medulla. This also results in increased urination.
Does lithium affect AQP2?
Lithium causes a dramatic decrease in the numbers of AQP2 expressed in the principal cells. This decrease is paralleled by a progressive development of severe polyuria. Of the few AQP2s that do get expressed in the presence of lithium, very few are able to travel to the apical membrane where they must be if they are to perform their function of letting water flow across the membrane. Lithium has been shown to impair the production of cAMP in CD cells, and it is likely that reduced cAMP is, in part, responsible for the reduced numbers of AQP2 found in patients with lithium-induced NDI.
What is nephrogenic diabetes?
Nephrogenic diabetes insipidus (nephrogenic DI) results from partial or complete resistance of the kidney to the effects of antidiuretic hormone (ADH). As a result, patients with this disorder are not likely to have a good response to hormone administration (as desmopressin [dDAVP]) or to drugs that increase either the renal response to ADH ...
Is UpToDate a substitute for medical advice?
The content on the UpToDate website is not intended nor recommended as a substitute for medical advice, diagnosis, or treatment. Always seek the advice of your own physician or other qualified health care professional regarding any medical questions or conditions. The use of UpToDate content is governed by the UpToDate Terms of Use. ©2021 UpToDate, Inc. All rights reserved.
Is nephrogenic di X-linked?
Hereditary nephrogenic DI, which is largely an X-linked disease, may also be seen by internists since early recognition and treatment in infancy has led to survival to adulthood [ 2-4 ]. In addition, affected women may be carriers with few or no symptoms until pregnancy or other stress.
What is lithium used for?
1 It is also used as augmentation of antidepressant medication and as a mood stabilizer in the treatment of schizoaffective disorder. Only recently has lithium been endorsed as superior in the prevention of suicide and severe affective episodes. 2, 3 Yet, despite its therapeutic superiority and versatility, adverse effects limit lithium use in clinical practice. Over half of all patients may discontinue lithium at some time, and adverse effects are the most common reason for discontinuation. 4
What are the side effects of lithium?
Polyuria and polydipsia are common adverse effects of lithium treatment. 4 NDI with polyuria as primary disturbance occurs when the distal renal tubular cells become impaired in their ability to respond to vasopressin and reuptake water through aquaporines. 8 Estimates for the prevalence of polyuria and renal diabetes insipidus vary widely. Up to 70% patients treated with lithium may experience urine concentration deficits. 21 Up to 40% may experience NDI. 8 Hypernatraemia can occur, when patients with lithium treatment have developed urine concentration deficits and lose more water than they actually take in. For instance, this can happen in the context of an acute infection, surgical interventions, excessive sweating when changing to a warmer climate or increased concentrations of exercise. It still remains unclear how far NDI is reversible once lithium has been discontinued. This question has not been investigated in recent years. NDI reversibility may depend on length of treatment. Long-term lithium treatment may render NDI irreversible. 7, 22 However, it remains less clear what happens after intermediate lithium exposure. Grandjean et al. 22 suggest that NDI is ‘usually’ reversible after lithium treatment up to 6 years. Garofeanu et al. 7 pooled data from several studies of patients who had been treated with lithium for a mean of 8 years and who had developed NDI. In 5% of all cases, NDI was reversible and in 25% partially reversible. In the remaining 70% cases, NDI persisted. Our study also suggests that lithium associated NDI may not be reversible in all cases. We found hypernatraemia episodes with confirmed or suspected NDI not only associated with current but also with past lithium use. We could also endorse a time trend: length of lithium exposure increased the likelihood of suspected or definite NDI. Despite a high prevalence of NDI in patients taking lithium, tubular function is not routinely assessed in clinical practice. Checking urine osmolality, plasma osmolality and daily urine output could improve the detection rate of NDI, thereby reducing a lithium-specific risk factor for hypernatraemia.
How many osmolality samples are there for NDI?
There were only 15 urine osmolality samples and no plasma osmolality samples available. Thus, diagnosis of suspected NDI had to rely solely on the documentation of polyuria–polydipsia complex in the medical records. Patients with psychogenic polydipsia or excessive fluid intake due to xerostomia can also present with a polyuria–polydipsia complex, clinically indistinguishable from NDI. This may have led to an overestimation of the NDI prevalence. In NDI, polydipsia is a consequence of polyuria. Primary polydipsia, for instance psychogenic polydipsia, however, usually leads to hyponatremia and is unlikely to cause hypernatraemia.
How long does it take for hypernatraemia to be clinically significant?
We considered hypernatraemia to be clinically significant when it was at least moderate with a serum sodium concentration of at least 150 mmol/L. 15 For each episode, we determined whether the hypernatraemia was an isolated incident or persistent: hypernatraemia was defined as an isolated incident if sodium concentrations had been normal within 3 months prior to the current episode or persistent if abnormal concentrations had existed for more than 3 months prior to the current hypernatraemia episode.
How old are people who have lithium?
The mean age per episode was 63.4 [standard deviation (SD) 18.9] and the median 69 years. The age ranged from 19 to 93 years. A total of 59% of episodes related to patients aged 65 years or older. In 42% of episodes, patients had been exposed to lithium at some point, either currently (28%) or in the past (14%) ( Table 1 ).
Where was the Lisie study conducted?
We performed a retrospective cohort study in the Swedish region of Norrbotten into the effects and potential adverse effects of lithium treatment and other mood stabilizers (LiSIE). For this particular study, we included all patients who had experienced at least one episode with a sodium concentration ⩾150 mmol/L between 1997 and 2013. Medical records were reviewed regarding past or current lithium exposure, diabetes insipidus and other potential risk factors for hypernatraemia.
Is lithium a risk factor for hypernatraemia?
In this study, we tested the hypothesis that lithium treatment was a risk factor for hyperna traemia.