What is the best foot care for diabetics?
In many cases, antibiotics are given for treatment of infections. If a wound develops, then dressings and medications are applied to the foot in order to help the wounds heal. A person with diabetic foot problems who develops a wound that either does not heal or develops a serious infection may sometimes need to have a surgery (amputation) performed in order to treat the …
How to care for your feet with diabetes?
First, the doctor will make attempts to treat the diabetic foot without doing any kind of surgery. Some of the non-surgical methods are: Keeping wounds clean and dressed Keeping close track of the growing gangrene on the toes Wearing cast boot or total contact cast or any other immobilization devices. Surgical Treatment
What is the best remedy for diabetic foot pain?
Apr 20, 2012 · Negative-pressure wound therapy (NPWT) has emerged as a new treatment for diabetic foot ulcers. It involves the use of intermittent or continuous subatmospheric pressure through a special pump (vacuum-assisted closure) connected to a resilient open-celled foam surface dressing covered with an adhesive drape to maintain a closed environment.
How to treat diabetic foot at home?
a multidisciplinary approach to care for the diabetic foot is recommended, which includes annual (3-month intervals in high-risk patients) assessments by a primary care physician and referral to a podiatrist and vascular surgeon for diabetics with a foot ulcer for evaluation of foot arterial perfusion and off-loading therapy to reduce plantar …

How do you treat diabetic feet?
Diabetes Foot CareWash and Dry Your Feet Daily.Check Your Feet Every Day.Take Care of Your Toenails.Be Careful When Exercising.Protect Your Feet With Shoes and Socks.Make Sure Your Shoes Fit.Good Shoe Choices.Diabetic Socks.More items...•May 18, 2021
Can diabetic foot be cured?
Background. Diabetic foot infections are a frequent clinical problem. About 50% of patients with diabetic foot infections who have foot amputations die within five years. Properly managed most can be cured, but many patients needlessly undergo amputations because of improper diagnostic and therapeutic approaches.Oct 24, 2014
What is the best medicine for diabetic foot?
Agents such as cephalexin, dicloxacillin, amoxicillin-clavulanate, or clindamycin are effective choices. If methicillin-resistant S aureus (MRSA) infection is suspected, then clindamycin, trimethoprim-sulfamethoxazole, minocycline, or linezolid may be used.Jan 16, 2020
What is the fastest way to heal a diabetic foot wound?
Tips to help a diabetic wound heal fasterWash your hands with soap and water.Rinse off the wound with warm water.Apply pressure to stop any bleeding.Apply antibiotic cream and cover with a bandage.
How does a diabetic foot start?
Although rare, nerve damage from diabetes can lead to changes in the shape of your feet, such as Charcot's foot. Charcot's foot may start with redness, warmth, and swelling. Later, bones in your feet and toes can shift or break, which can cause your feet to have an odd shape, such as a “rocker bottom.”
What are signs of diabetic feet?
Signs of Diabetic Foot ProblemsChanges in skin color.Changes in skin temperature.Swelling in the foot or ankle.Pain in the legs.Open sores on the feet that are slow to heal or are draining.Ingrown toenails or toenails infected with fungus.Corns or calluses.Dry cracks in the skin, especially around the heel.More items...•Jun 22, 2021
What is the best antibiotic for foot infection?
Patients with mild infections can be treated with oral antibiotics, like cephalexin, dicloxacillin, amoxicillin-clavulanate, or clindamycin. A more severe infection is typically treated intravenously with ciprofloxacin-clindamycin, piperacillin-tazobactam, or imipenem-cilastatin.
What part of the foot hurts with diabetes?
Diabetic foot pain is mainly due to a condition called peripheral neuropathy. Approximately 50% of people who have type 2 diabetes will develop peripheral neuropathy, which happens when high blood sugar levels cause damage to the nerves in the legs and the feet.Jun 11, 2020
What is a diabetic foot infection?
Diabetic foot infection, defined as soft tissue or bone infection below the malleoli, is the most common complication of diabetes mellitus leading to hospitalization and the most frequent cause of nontraumatic lower extremity amputation.Aug 1, 2013
Which ointment is best for diabetic wound?
Antibiotics such as Neomycin, Gentamycin, and Mupirocin have good antibacterial coverage when used topically. Silver containing dressings come in different formulations and have very good antibacterial coverage. Silver dressings and polyherbal preparations have shown good results in healing diabetic foot wounds[74].
What is the best dressing for diabetic foot ulcer?
Various types of nonadherent or saline-soaked gauze dressings are often regarded as standard treatment for diabetic ulcers and have usually been used as the control arm in studies of dressings. These dressings are designed to be atraumatic and to provide a moist wound environment.Aug 1, 2004
Is Betadine safe for diabetics?
The use of full-strength betadine, hydrogen peroxide, whirlpools, and soaking are not recommended, as these practices could lead to further complications.
What Are Diabetic Foot?
Diabetic foot are one of the complications of diabetes. Over time, people with diabetes start feeling numbness in their foot because of poor blood flow. Nerve damage is the main reason for this. One can have nerve damage in any part of the body. But nerves in your legs and foot are mostly affected areas.
How Can Diabetes Affect Foot and Legs?
If you have had diabetes for a long time now, and you have been suffering from high blood sugar levels (hyperglycemia), it causes severe complications in your foot.
Other Causes of Foot Problems
Corns are the buildup tissues or hard skin in the toes, especially near the bony area of a toe or between them. They might be the result of pressure or friction generated in the toes by the shoes.
Diabetic Foot Complications
Well, diabetic feet themselves are one of the severe complications of diabetes. But this doesn’t stop here. Diabetic feet further cause complications as well. Some are:
Treatment of Diabetic Foot
Of course, the treatment for diabetic feet depends upon the severity of the wound. Both surgical and nonsurgical treatments are available.
Tips For Healthy Foot
Don’t leave your foot unchecked even for one day. You need to avoid cuts and injuries. Checking for swelling, redness, blisters, corns, calluses, if any should be caught initially itself. Ask for someone’s help to check the bottom side of the feet. You can use a mirror also.
A Word From Mantra Care
If you are looking for more information on this topic or on Diabetes treatment, Online Therapy, Hypertension, PCOS treatment, Weight Loss, and Physiotherapy, please visit mantracare.org or feel free to reach out to us at +91-9711118331 or email at [email protected]. You can also download our free Android App or IOS app.
How long does it take for a foot ulcer to heal?
The majority (60–80%) of foot ulcers will heal, while 10–15% of them will remain active, and 5–24% of them will finally lead to limb amputation within a period of 6–18 months after the first evaluation.
What is EGF in diabetics?
Epidermal growth factor (EGF) act s on epithelial cells, fibroblasts, and smooth muscle cells to promote healing [61]. Evidence for the use of EGF in diabetic ulcers is limited, with only a small amount of data reporting a significantly higher rate of ulcer healing with EGF use compared with placebo [62].
What are the most common causes of foot ulcers?
Pathogenesis. The most significant risk factors for foot ulceration are diabetic neuropathy, peripheral arterial disease, and consequent traumas of the foot. Diabetic neuropathy is the common factor in almost 90% of diabetic foot ulcers [9, 10]. Nerve damage in diabetes affects the motor, sensory, and autonomic fibers.
What is the most significant and devastating complications of diabetes?
Introduction. Diabetic foot is one of the most significant and devastating complications of diabetes, and is defined as a foot affected by ulceration that is associated with neuropathy and/or peripheral arterial disease of the lower limb in a patient with diabetes. The prevalence of diabetic foot ulceration in the diabetic population is 4–10%;
What are the symptoms of peripheral neuropathy?
Symptoms such as a burning sensation; pins and needles; shooting, sharp, or stabbing pains; and muscle cramps, which are distributed symmetrically in both lim bs (“stocking and glove distribution”), and often worse at night, are usually present in peripheral neuropathy.
Why should gangrene be kept dry?
The only exception is dry gangrene, where the necrotic area should be kept dry in order to avoid infection and conversion to wet gangrene. A wound’s exudate is rich in cytokines, platelets, white blood cells, growth factors, matrix metalloproteinases (MMPs), and other enzymes.
What is the effect of neuropathy on the motor, sensory, and autonomic fibers?
Motor neuropathy causes muscle weakness, atrophy, and paresis. Sensory neuropathy leads to loss of the protective sensation of pain, pressure, and heat.
What is the treatment for invasive foot infection?
When invasive foot infection develops and tissue beneath the fascia is involved, inpatient care is recommended for systemic antibiotic therapy, vascular laboratory testing of artery limb perfusion, and surgical debridement of infected tissue. The goals of treatment are to achieve a healed foot and keep the patient ambulatory.
What is the risk of a foot ulcer?
Once a foot ulcer develops, the limb is at high risk for invasive infection and, when combined with peripheral artery occlusive disease, the patient should be considered to have critical limb ischemia.
How many people develop diabetic foot ulcers?
It is estimated that 19–34% of patients with diabetes are likely to be affected with a diabetic foot ulcer in their lifetimes, and the International Diabetes Federation reports that 9.1–26.1 million people will develop DFUs annually.1These numbers are alarming, as the clinical implications for the development of a DFU are not negligible.
What is the goal of dressing?
It is generally agreed that the goal of a dressing should be to create a moist environment that promotes granulation, autolytic processes, angiogenesis, and more rapid migration of epidermal cells across the wound base.9 ,11,15The selected dressing should also be appropriate to manage excess wound exudates.
Can you swab after debridement?
It is recommended that, before antibiotic therapy, a deep tissue culture via biopsy or curettage after debridement be obtained. Swab specimens should be avoided, especially in inadequately debrided wounds.9Antibiotic therapy should be targeted to aerobic Gram-positive cocci in mild to moderate infections.
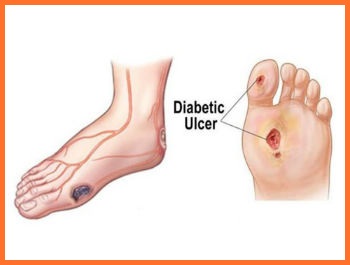
What Does a Diabetic Foot Look Like?
The foot’s appearance will provide some tell-tale signs of diabetic foot. A physical examination is, therefore, the usual starting place for doctors.
What Does Diabetes Do To Your Feet?
Diabetic neuropathy – where nerve damage leads to numbness in the foot and insensitivity to pain or irritation (which, in turn, can lead to infections and other complications like gangrene.)
What Are The Signs Of Diabetic Feet?
The main signs of a diabetes-related foot condition are the physical irregularities described above.
What Causes Diabetic Foot?
Diabetic foot is caused by the side effects of diabetes: notably, high blood sugar levels that lead to restricted blood flow to the body’s extremities and nerve damage.
How Do You Treat Diabetic Feet?
Firstly, it’s very important to recognize the symptoms of diabetic foot and seek treatment immediately if you suspect it.
What is Diabetic Foot Pain
Diabetic foot pain is a common diabetic complication marked by pain and nerve damage in the feet. Diabetics often have poor circulation, so blood flow to their feet can reduce which makes it difficult for wounds to heal.
Types of Diabetic Foot Pain
Diabetic foot pain is a very common complication of diabetes, occurring in up to 50% of diabetic patients. There are three main types: diabetic neuropathy (nerve damage), Charcot’s joints (joint deformities that occur due to nerve damage), and diabetic ulcers (ulcers on the feet).
Diabetic Foot Pain Ulcers
Diabetic foot ulcers are one of the most common diabetic complications. In fact, they can affect up to 30% of people living with diabetes. As a result of nerve damage from diabetic neuropathy, it is difficult for your body to heal itself and recuperate after an injury.
Diabetic Sores on Leg
Diabetes sores are open wounds that diabetic people get on their legs. Diabetic sores occur when the diabetic person does not have enough blood flow to heal a wound site, which can happen because of nerve damage in diabetics or because they do not check themselves often for cuts and scrapes.
Treatment of Diabetic Foot Pain
Treatment for diabetic foot problems varies according to the severity of the condition. Surgical and nonsurgical treatments are available in a variety of forms.
Diabetic Foot Pain Care
This is so important. Diabetic foot pain can occur in the feet and lower limbs of diabetic patients, resulting from damage to nerves and blood vessels caused by diabetes mellitus.
Diabetic Foot Pain Prevention
Diabetic neuropathy is a problem that affects the nerves in the feet and legs, causing severe discomfort and pain. It’s also possible to prevent or reduce many of these problems by managing diabetes.
Diabetic Foot
Diabetes is one of the most common diseases in the society, can have more than one result in people with the disease. Diabetic foot is the name given to chronic standing wounds in cases where the disease of a diabetic patient lasts for a long time or when the sugar level becomes difficult to control.
What Is Diabetic Foot?
Diabetics are adversely affected throughout their lives due to standing wounds. A foot problem that a normal person experiences and overcomes in a short time, such as ingrown toenails, a person with diabetes has to live under very difficult conditions. These wounds can cause diabetic foot ulcers.
What Are The Diabetic Foot Sypmtoms?
Diabetic foot is a disease that occurs over time. It is difficult to understand at first because it does not spread in a very short time. Therefore, when diabetic foot symptoms are felt or started to be seen, it is important to consult a specialist.
Why Does Diabetic Foot Disease Occur?
There are many reasons that cause diabetic foot disease to occur. Nervous and vascular diseases trigger diabetic foot disease. Uncontrolled diabetes, smoking of the patient, mistakes in shoe selection, nail problems, obesity, advanced age and hygiene problems are some of the factors that cause diabetic foot disease.
How Is Diabetic Foot Care Done?
What is a diabetic foot? As stated in the title, microbes enter from wounds and cracks caused by the dryness of the feet of diabetics and easily cause a serious infection in the whole foot.
Shoe Selection In Diabetic Foot Treatment
Diabetic foot patients should take extreme care in choosing shoes and socks. Socks should always be seamless, wool or cotton. Diabetic foot socks should never be too big. Another important item of diabetic foot care rules is to change socks every day.
What Is Good For Diabetic Feet?
First of all, it should be tried to bring the blood sugar level to normal levels in order to strengthen the blood circulation. Ankle exercises should be done to increase blood circulation. If you are wondering what is good for diabetic footed, the most important thing is to keep the blood level at a normal level.
How to prevent ulcers in diabetic feet?
Stay off your feet to prevent pain from ulcers. This is called off-loading, and it’s helpful for all forms of diabetic foot ulcers. Pressure from walking can make an infection worse and an ulcer expand. Your doctor may recommend wearing certain items to protect your feet: shoes designed for people with diabetes. casts.
How to prevent foot problems?
You can also help prevent foot problems by: washing your feet every day. keeping toenails adequately trimmed, but not too short. keeping your feet dry and moisturized.
What causes ulcers on the foot?
Diabetic Ulcers: Causes and Treatment. Foot ulcers are a common complication of diabetes that is not being managed through methods such as diet, exercise, and insulin treatment. Ulcers are formed as a result of skin tissue breaking down and exposing the layers underneath.
How many diabetic ulcers are infected?
According to a 2017 review article in the New England Journal of Medicine, more than half of diabetic foot ulcers become infected. Approximately 20 percent of moderate to severe foot infections in people with diabetes lead to amputation. Preventive care is crucial.
How long does it take for a diabetic foot ulcer to heal?
Untreated infections may require amputations. While your ulcers heal, stay off your feet and follow your treatment plan. Diabetic foot ulcers can take several weeks to heal. Ulcers may take longer to heal if your blood sugar is high and constant pressure is applied to the ulcer.
Why do diabetics get ulcers on their feet?
Causes of diabetic foot ulcers. Ulcers in people with diabetes are most commonly caused by: poor circulation. high blood sugar (hyperglycemia) nerve damage. irritated or wounded feet. Poor blood circulation is a form of vascular disease in which blood doesn’t flow to your feet efficiently.
Why is it so hard to heal ulcers?
Poor circulation can also make it more difficult for ulcers to heal. High glucose levels can slow the healing process of an infected foot ulcer, so blood sugar management is critical. People with type 2 diabetes and other ailments often have a harder time fighting off infections from ulcers.
