Treatment
- Hospitalization. Certain clinical presentations warrant hospitalization for patients with ADHF. ...
- Inpatient Monitoring. Hospitalized HF patients are at risk for hemodynamic instability and arrhythmias; therefore, close monitoring is necessary.
- Diuresis. ...
- Vasodilation. ...
- Ultrafiltration. ...
- Inotropic Therapy. ...
Full Answer
How to improve time to diagnosis in acute heart failure?
Jan 03, 2022 · An initial dose of 5 to 10 mcg/min of IV nitroglycerin is recommended with the dose increased in increments of 5 to 10 mcg/min every three to five minutes as required and tolerated (dose range 10 to 200 mcg/min). Similar benefits have been described with high-dose IV isosorbide dinitrate, where available [ 12,13 ].
What are the treatment options for heart failure?
Keywords: Treatment; Acute; Decompensated Heart Failure This review is aiming to discuss treatment of acute decompensated heart failure, the presented review was conducted by search-ing in Medline, Embase, Web of Science, Science Direct, BMJ journal and Google Scholar for, researches, review articles and reports, ...
Does ejection fraction decrease with acute heart failure?
The main treatment goals in the hospitalized patient with heart failure are to restore euvolemia and to minimize adverse events. Common in-hospital treatments include intravenous diuretics, vasodilators, and inotropic agents.
What does compensated CHF mean?
Acute decompensated heart failure (ADHF) is a clinical syndrome of worsening signs or symptoms of heart failure (HF) requiring hospitalization or other unscheduled medical care. For many years, ADHF was viewed as simply an exacerbation of chronic HF as a result of volume overload, with few implications beyond a short-term need to intensify diuretic therapy (a similar …
What is the treatment for decompensated heart failure?
Common in-hospital treatments include intravenous diuretics, vasodilators, and inotropic agents. Novel pharmaceutical agents have shown promise in the treatment of acute decompensated heart failure and may simplify the treatment and reduce the morbidity associated with the disease.
How is acute decompensation treated?
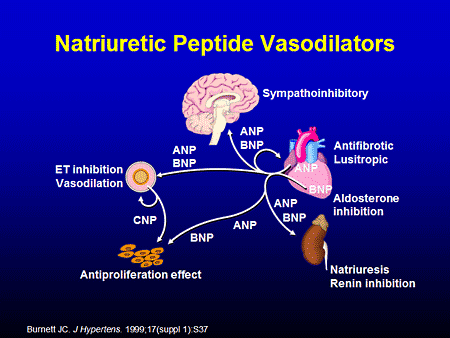
TreatmentLoop diuretics. Volume overload is central to the pathophysiology of most episodes of acute decompensated heart failure. ... Ultrafiltration. ... Vasodilators. ... Natriuretic peptides. ... Respiratory therapies. ... Inotropes.
How long can you live with acute decompensated heart failure?
The mean life expectancy of patients discharged after admission for HF has been estimated at 5.5 years [3]. Several studies investigated the short- and intermediate-term risk of death after discharge for acutely decompensated heart failure (ADHF).Jan 26, 2017
Can decompensated heart failure be cured?
It cannot usually be cured, but the symptoms can often be controlled for many years.
How serious is acute decompensated heart failure?
ADHF is a common and potentially serious cause of acute respiratory distress. The condition is caused by severe congestion of multiple organs by fluid that is inadequately circulated by the failing heart.
What is the most important treatment for a patient suffering from CHF exacerbation?
The main goal in treatment for CHF exacerbation is to reduce the fluid volume in the body. If recently prescribed beta-blockers or other medication changes caused your CHF exacerbation, you may be given diuretics, which are water pills that increase the amount of water and salt that leave your body through urination.Jun 23, 2021
What happens when a patient decompensated?
Decompensated and compensated HF In medicine, the term decompensation refers to the deterioration of a structure or system that was previously functioning. This means the heart can no longer continue to compensate for its defects. A system that is compensated can function despite the presence of stressors or defects.
What causes acute decompensated heart failure?
Acute decompensated heart failure (ADHF) refers to rapid onset of fluid volume overload. The most common causes are medication and dietary noncompliance; however, acute coronary syndrome, arrhythmias, uncontrolled hypertension, and infections such as endocarditis may also cause acute decompensated heart failure.
How do you know when a heart failure patient is Decompensating?
The cardinal manifestations of ADHF are dyspnea, fluid retention, and fatigue. Fluid retention, commonly leads to pulmonary congestion and peripheral edema in patients with ADHF. Patients may present with progressive weight gain, lower extremity edema, increasing dyspnea on exertion, or dyspnea at rest.
What happens when diuretics don't work?
Stay on top of this Diuretics can stop working and that doesn't mean anything bad necessarily. Different diuretics work on different parts of the kidney. If one stops working or doesn't work as well, your doctor can change up your medications to see if something else works better.Sep 23, 2020
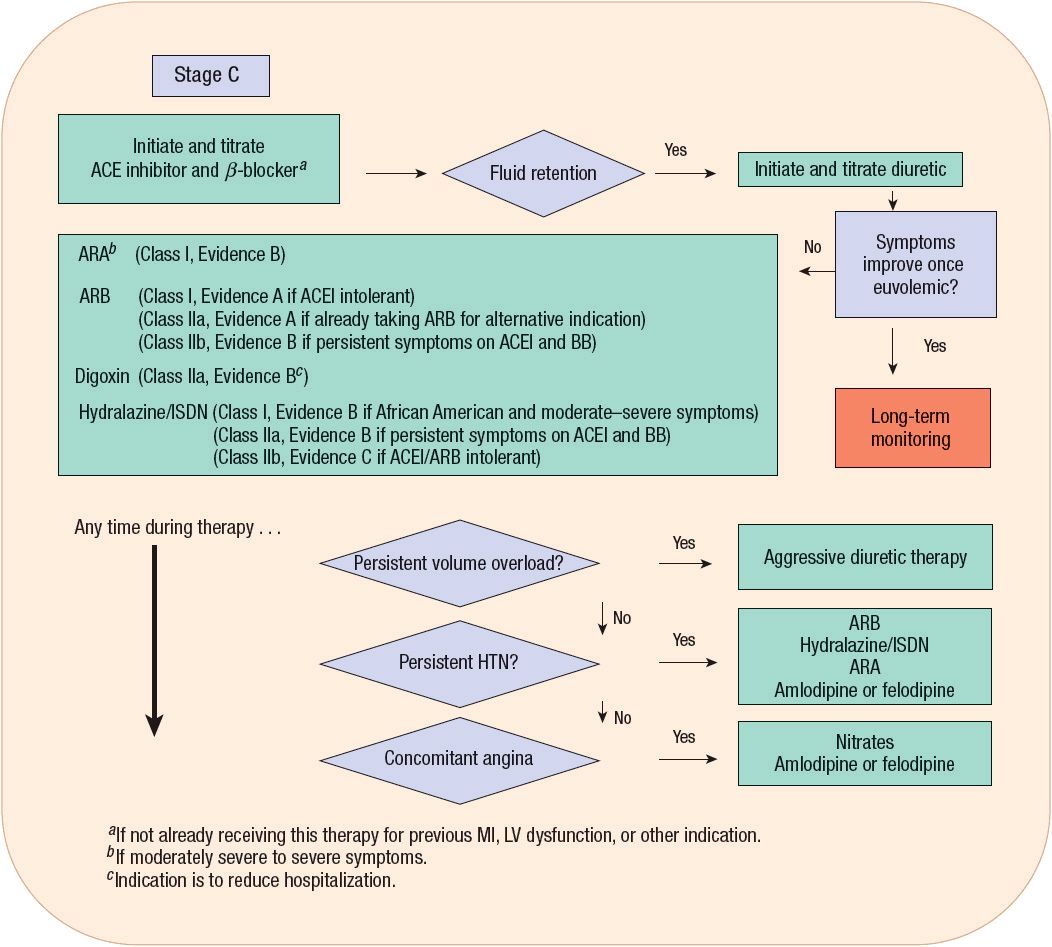
What is the first line treatment for heart failure?
First-line drug therapy for all patients with HFrEF should include an angiotensin-converting enzyme (ACE) inhibitor and beta blocker. These medications have been shown to decrease morbidity and mortality.
What is a commonly prescribed drug for congestive heart failure?
There are many different types of diuretic, but the most widely used for heart failure are furosemide (also called frusemide) and bumetanide.
What is the treatment for acute decompensated heart failure?
Common in-hospital treatments include intravenous diuretics, vasodilators, and inotropic agents. Novel pharmaceutical agents have shown promise in the treatment of acute decompensated heart failure and may simplify the treatment and reduce the morbidity associated with the disease.
How much Nesiritide is given?
Nesiritide is given as a loading dose of 2 μg/kg, followed by an infusion of 0.01 to 0.03 mg/kg/min. Nesiritide effectively lowers LV filling pressures and improves symptoms during the treatment of ADHF. Nesiritide is not indicated for diuresis, despite its classification as a natriuretic.
What vasodilators cause venous dilation?
By stimulating guanylate cyclase within smooth-muscle cells, vasodilators such as nitroglycerin, nitroprusside, and nesiritide cause both arterial and venous dilation, which results in a lowering of LV filling pressure, improved stroke volume, and improved forward cardiac output, without increasing arrhythmias.
How does adenosine antagonist affect diuresis?
Adenosine antagonists induce diuresis both by inhibiting sodium absorption in the proximal tubule and by blocking tubuloglomerular feedback, thereby increasing the glomerular filtration rate in HF.51In an early clinical study, the adenosine A1antagonist BG9719 caused a dose-dependent increase in urine output.
How long does it take for nitroglycerin to cause headaches?
Hemodynamic tolerance of nitroglycerin, or tachyphylaxis, occurs as early as 1 to 2 hours after initiation of the drug.
How many people are affected by heart failure?
Heart failure (HF) is a growing problem worldwide: more than 20 million people around the world are affected, and more than 5 million in the United States.1The prevalence of HF follows an exponential pattern, and it rises with age. Heart failure affects 6% to 10% of people over the age of 65 years. Although the relative incidence is lower in women ...
What are the signs of HF?
Patients with a new diagnosis of HF are much more likely to present with pulmonary edema or cardiogenic shock, while decompensation of chronic HF usually presents with other signs of congestion and fluid retention, such as weight gain, exertional dyspnea, or orthopnea.
What is ADHF in medical terms?
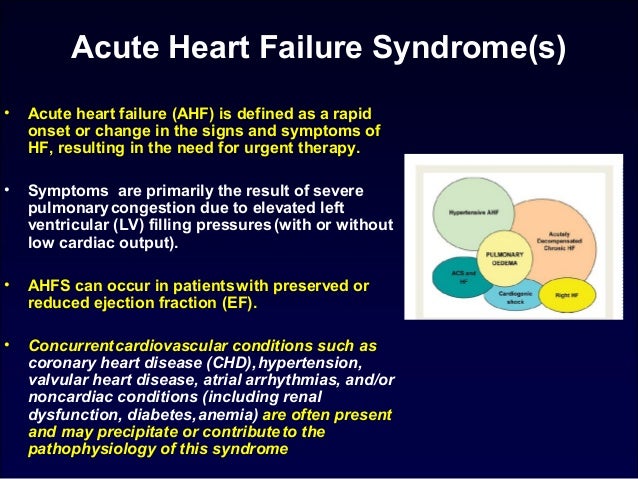
Acute decompensated heart failure (ADHF) is a clinical syndrome of worsening signs or symptoms of heart failure (HF) requiring hospitalization or other unscheduled medical care. For many years, ADHF was viewed as simply an exacerbation of chronic HF as a result of volume overload, with few implications beyond a short-term need to intensify diuretic therapy (a similar paradigm to exacerbations of chronic asthma). Recent decades have seen an explosion of research into the epidemiology, pathophysiology, outcomes, and treatment of ADHF. Although some controversy persists, multiple lines of evidence now support the concept that ADHF is a unique clinical syndrome with its own epidemiology and underlying mechanisms and that there is a need for specific therapies. This viewpoint suggests that ADHF is not just a worsening of chronic HF any more than an acute myocardial infarction (MI) is just a worsening of chronic angina.
Why are loop diuretics used in AHF?
Interestingly, loop diuretics are commonly used worldwide to relieve the fluid congestion seen in AHF despite the lack of randomized control studies. At its worst, AHF will be represented as cardiogenic shock and hemodynamic instability needs to be addressed with the use of inotropes.
What is acute HF?
Acute HF (also referred to as ADHF or “acute HF syndromes”) is the rapid occurrence of symptoms and signs of HF, or the deterioration of stable chronic HF, leading to the requirement of hospitalization and/or intensive therapy (see also Chapters 43 and 44Chapter 43Chapter 44 ). 74 It may occur in the presence or absence of preexisting cardiac disease, and may be new-onset HF or worsening of previously stable HF. 75 Thus acute HF has a broad spectrum of clinical presentations and an evolving clinical definition. 76
Is ADHF worse than MI?
This viewpoint suggests that ADHF is not just a worsening of chronic H F any more than an acute myocardial infarction (MI) is just a worsening of chronic angina. Outcome data from a variety of studies now support the concept that hospitalization for ADHF can often signal a dramatic change in the natural history of the HF syndrome.
How long does it take for a patient to show signs of hypertension?
1 The average patient has had symptoms for about 5 to 7 days before seeking medical attention. 10,11.
Is AHF a diagnosis?
AHF is a clinical diagnosis. No single test or physical exam feature definitively “rules in” or “rules out” AHF. Thus there is no diagnostic “gold standard.” Perhaps unsurprisingly, there is neither a universal, well-accepted definition of AHF, nor a nomenclature to describe the various AHF syndromes. 11 Various names have been used, including acute decompensated heart failure (ADHF), hospitalization for heart failure (HHF), and acute heart failure syndromes (AHFS). Currently, AHF is the most widely used and is the current terminology in several consensus guidelines.12,13
Is AHF a high rate of morbidity?
AHF is associated with a high rate of morbidity and mortality; therefore, it must be recognized and treated promptly. With progression of heart failure, the heart becomes an ineffective pump and is unable to adequately manage circulating blood volume.
What to do if your weight does not improve?
If weight does not improve or if increasing symptoms of dyspnea or other symptoms of congestion, call a care provider. Chronic heart failure management programs, if available.
How long does it take for AHF to develop?
AHF is often not acute in onset, typically developing gradually over the course of days to weeks, where the acuity is a function of the need for urgent or emergent therapy due to the severity of these signs or symptoms. AHF may be the result of a primary disturbance in the systolic or diastolic function of the heart or of abnormal venous ...
What is the best medication for AHF?
Catecholamines such as dobutamine , epinephrine, and norepinephrine have been used to improve myocardial contractility and increase the heart rate in the setting of AHF. Dobutamine is a predominant beta-1adrenergic receptor agonist with mild vasodilating properties.
What is the most common manifestation of AHF?
In addition to disturbances in oxygenation due to pulmonary edema, renal dysfunction is a frequent manifestation of AHF and reflects the multisystem nature of this disease.
What is the cause of AHF?
AHF may be the result of a primary disturbance in the systolic or diastolic function of the heart or of abnormal venous or arterial vasoconstriction, but generally represents an interaction of multiple factors, including volume overload.
What is the meaning of AHF?
Acute heart failure (AHF), also known as acute decompensated heart failure or cardiac failure, is not a single disease entity, but rather a syndrome of the worsening of signs and symptoms reflecting an inability of the heart to pump blood at a rate commensurate to the needs of the body at normal filling pressure.
What is heart failure in Europe?
In Europe, heart failure (HF) is the cause of 5% of acute hospital admissions, is present in 10% of patients in hospital beds, and accounts for 2% of the national expenditure on health, mostly due to the cost of hospital admissions. Patients with a substrate of cardiovascular disease are most at risk for developing AHF, ...
What Is Acute Heart Failure?
Acute heart failure can be a rapid change in the heart's ability to pump, or fill with, enough blood to nourish the body's cells. It is potentially life-threatening and often requires hospitalization for treatment.
Acute vs. Chronic Heart Failure
In chronic heart failure, symptoms are kept at a manageable level, often for very long periods of time, with medical treatment and by the body's own compensatory mechanisms. These compensatory mechanisms may include: 2
Symptoms of Acute Heart Failure
On their own, each of the symptoms of heart failure do not indicate heart failure. However, if you have more than one of these symptoms, especially if they appear suddenly, you should have them evaluated by a healthcare professional as soon as possible. These signs include:
Diagnosis and Treatment of Acute Heart Failure
If any signs and symptoms of heart failure develop, especially if there has not been any previous diagnosis of heart failure, it is important to see a healthcare professional quickly. After performing a physical exam and obtaining information about current symptoms and your medical history, your doctor may order the following tests:
Summary
Heart failure occurs when your heart cannot efficiently pump blood to the rest of your body. Acute heart failure occurs suddenly, while chronic heart failure takes place over time. It typically requires medical help as soon as possible because it can be life-threatening if left untreated.
A Word From Verywell
A diagnosis of heart failure can feel scary and overwhelming. Heart failure can be managed by collaborating with a healthcare professional on a plan of care that can allow life to be lived to its fullest.
Frequently Asked Questions
The difference between acute heart failure and acute decompensated heart failure is subtle. Acute heart failure is the sudden development of signs and symptoms of heart failure, which need to be evaluated quickly to avoid serious complications, when there is no prior diagnosis of heart failure.
What is ADHF in medical terms?
December 9, 2019. Decompensated heart failure, also called Acute Decompensated Heart Failure (ADHF), occurs in patients with pre-existing heart failure. It refers to a worsening of symptoms due to fluid retention (volume overload). 1 These symptoms can impair the day-to-day quality of your life.
Why is heart failure decompensated?
Chronic heart failure that has been well-managed and stable can rapidly decompensate for many reasons. A severe illness, heart attack, or not being compliant with treatment can lead to a heart failure decompensation. 2 For example, changes in diet (eating more salt), increased fluid intake, and not taking medications as prescribed can be causes of decompensated heart failure. Decompensation can also occur because of any worsening of other chronic conditions. For example, high blood sugars in diabetics, COPD exacerbations, infections, or kidney problems. Underlying cardiac conditions can worsen and may also contribute to decompensation, such as a heart attack, poorly controlled blood pressure, or arrhythmias. 2,4
What are the symptoms of ADHF?
Symptoms of ADHF include shortness of breath, fatigue, and fluid retention. Shortness of breath, dyspnea, and difficulty breathing can get worse with ADHF. 3,5 You may experience: Other symptoms include angina (chest pain), arrhythmias, nausea, weight loss, fatigue, or a change in urinary output could also be signs of advancing heart failure.
What is decompensated HF?
Decompensated and compensated HF. In medicine, the term decompensation refers to the deterioration of a structure or system that was previously functioning. This means the heart can no longer continue to compensate for its defects. A system that is compensated can function despite the presence of stressors or defects.
What are the clinical details of decompensation?
Clinical details about the causes of decompensation can influence treatment choices, including medication selection. Your provider will evaluate you based on the self-reporting of symptoms, physical findings, lab tests, evaluation of ventricular function, and, if necessary, more invasive testing. 2.
How does decompensated heart failure work?
Treating decompensated heart failure involves improving symptoms, managing underlying medical conditions, preserving renal function, and preventing further heart damage. 1,2,4 It also involves hemodynamic management. This includes monitoring blood pressure, blood flow, and oxygenation levels, all of which can affect the function of the heart. 3,6
What are the symptoms of advancing heart failure?
Edema- increased swelling. Other symptoms include angina (chest pain), arrhythmias, nausea, weight loss, fatigue, or a change in urinary output could also be signs of advancing heart failure.
Overview
Heart failure is a life-threatening condition. When it occurs, your heart is still working, but it cannot deliver oxygen-rich blood throughout your body. With acute heart failure, you experience a sudden, rapid decline in heart functioning and the amount of blood your heart can pump to the rest of your body.
Symptoms and Causes
One of the most common symptoms is shortness of breath (dyspnea). You may experience:
Management and Treatment
Emergency treatment for acute heart failure restores blood flow and oxygen levels. Care often includes:
Prevention
Living a heart-healthy lifestyle can lower your risk of acute heart failure.
Living With
Life after acute heart failure often includes changes, like getting more physical activity. You may also need to avoid certain foods and limit salt and fat intake.