Medication
The most common causes of atelectasis and their treatments include: Surgery: Nurses or respiratory therapists will guide you in breathing exercises and sitting or standing upright as soon... Chest pressure: Using surgery or medicine, doctors can remove the source of the pressure. Blocked airway: ...
Procedures
Nov 10, 2021 · Depending on the underlying cause, a healthcare professional might suggest one or more of these treatments: Chest physiotherapy. This involves moving your body in different positions and using tapping motions, vibrations, or... Bronchoscopy. A healthcare professional can insert a small tube through ...
Therapy
Atelectasis treatments include: Bronchoscopy to clear blockages like mucus Medicine that you breathe in through an inhaler Physiotherapy such as tapping on your chest to break up mucus, lying on one side or with your head lower than your chest... A breathing tube or continuous positive airway ...
Nutrition
Mild atelectasis or a small pneumothorax may heal, and the lung may re-inflate on its own. If not, there are a variety of techniques for clearing blockages, removing excess air and healing the lung. In cases of atelectasis, your physician may recommend: Percussion on the chest to loosen mucus plugs in the airway
Which medications are used in the treatment of atelectasis?
These include: Lying down on the healthy side will enable the collapsed portion to re-expand under the impact of gravity. Periodic changes of position while lying down. Performing deep breathing exercises. The doctor might suggest the use of reward spirometry devices while performing... If there is ...
How do you fix atelectasis?
What are the treatment options for atelectasis?
What is atelectasis, and what are the treatments?

How to diagnose atelectasis?
To diagnose atelectasis, doctors usually start with X-rays (a test that provides pictures of the inside of your chest). Another test called a computed tomography (CT) scan can provide more detailed pictures. In more severe cases, a doctor may use a procedure called a bronchoscopy to see inside your airway.
How to tell if you have atelectasis?
If atelectasis affects only a small area of the lungs, you may not have any symptoms. But if it affects larger areas, the lungs cannot fill with enough air, and the oxygen level in your blood may go down. When this happens, uncomfortable symptoms can occur, including: 1 Trouble breathing (shortness of breath) 2 Increased heart rate 3 Coughing 4 Chest pain 5 Skin and lips turning blue
What causes a collapsed lung?
Atelectasis has many causes. Any condition that makes it hard to take deep breaths or cough can lead to a collapse in the lung. People may call atelectasis or other conditions a “ collapsed lung .”. Another condition that commonly causes a collapsed lung is pneumothorax.
What is the term for a collapse of one or more areas in the lung?
Atelectasis (pronounced at-uh-LEK-tuh-sis) is the term for a collapse of one or more areas in the lung. When you breathe in, your lungs fill up with air. This air travels to air sacs in your lungs (alveoli), where the oxygen moves into your blood. The blood delivers the oxygen to organs and tissues throughout your body.
Why do air sacs deflate?
When air sacs become deflated because of atelectasis, they cannot inflate properly or take in enough air and oxygen. If enough of the lung is affected, your blood may not receive enough oxygen, which can cause health problems. Atelectasis often develops after surgery.
What is the procedure called to check for blockage in the airway?
In more severe cases, a doctor may use a procedure called a bronchoscopy to see inside your airway. In this test, the doctor sends a small tube called a bronchoscope down the throat to look for a blockage or other issue. The test is fairly painless.
How to remove chest pressure?
Chest pressure: Using surgery or medicine, doctors can remove the source of the pressure. Blocked airway: Usually, during a bronchoscopy, doctors will remove the blockage so you can breathe freely again. Lung condition: Doctors may treat the condition with medicine or a procedure to relieve pressure on your lung.
Treatment for mild atelectasis
If you’re experiencing mild atelectasis, your doctor may recommend the following treatments:
Surgical procedures for atelectasis
If your atelectasis isn’t severe enough to require treatment at home, your doctor may recommend a surgical procedure to prevent it from getting worse.
Surgery for mild atelectasis
A surgical procedure may be performed to prevent mild atelectasis that isn’t severe enough to require a home treatment plan.
Surgery for moderate or severe atelectasis
If your atelectasis is severe enough, you may require a surgical procedure to prevent it from getting worse.
Preventing atelectasis
You can prevent atelectasis by avoiding certain activities and eating smaller meals. For example, you may be able to avoid lying down when you exhale by changing your posture more often.
Outcome of atelectasis
Having mild atelectasis or moderate or severe atelectasis doesn’t always mean you’ll need surgery, but it can be a serious condition.
Mild atelectasis
If you have mild atelectasis, your atelectasis may be temporary and mild enough to resolve with conservative treatments.
How to treat atelectasis?
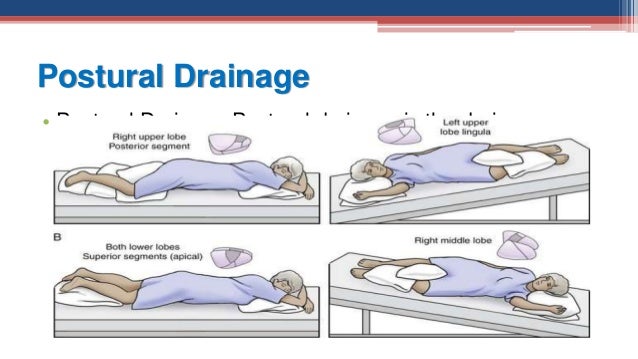
Most cases of atelectasis don’t require surgery. Depending on the underlying cause, your doctor might suggest one or a combination of these treatments: 1 Chest physiotherapy. This involves moving your body into different positions and using tapping motions, vibrations, or wearing a vibrating vest to help loosen and drain mucus. It’s generally used for obstructive or postsurgical atelectasis. This treatment is commonly used in people with cystic fibrosis as well. 2 Bronchoscopy. Your doctor can insert a small tube through your nose or mouth into your lungs to remove a foreign object or clear a mucus plug. This can also be used to remove a tissue sample from a mass so that your doctor can figure out what is causing the problem. 3 Breathing exercises. Exercises or devices, such as an incentive spirometer, that force you to breathe in deeply and help to open up your alveoli. This is especially useful for postsurgical atelectasis. 4 Drainage. If your atelectasis is due to pneumothorax or pleural effusion, your doctor may need to drain air or fluid from your chest. To remove fluid, they’ll likely insert a needle through your back, between your ribs, and into the pocket of fluid. To remove air, they may need to insert a plastic tube, called a chest tube, to remove extra air or fluid. The chest tube may need to be left in for several days in more severe cases.
How to remove fluid from atelectasis?
If your atelectasis is due to pneumothorax or pleural effusion, your doctor may need to drain air or fluid from your chest. To remove fluid, they’ll likely insert a needle through your back, between your ribs, and into the pocket of fluid.
How to check oxygen level in blood?
check your blood oxygen level with an oximeter, a small device that fits on the end of your finger. take blood from an artery, usually in your wrist, and check its oxygen, carbon dioxide levels, and blood chemistry with a blood gas test. order a chest X-ray.
What happens if you have low oxygen?
Having low blood oxygen can lead to: trouble breathing. sharp chest pain, especially when taking a deep breath or coughing. rapid breathing. increased heart rate. blue-colored skin, lips, fingernails, or toenails. Sometimes, pneumonia develops in the affected part of your lung.
Why do pleural effusions separate?
A pleural effusion causes the linings to separate and lose contact with each other. This allows the elastic tissue in your lung to pull inward, driving air out of your alveoli.
What causes atelectasis in the lung?
Atelectasis that affects most of your lung or happens quickly is almost always caused by a life-threatening condition , such as blockage of a major airway or when a large amount or fluid or air is compressing one or both lungs. Last medically reviewed on July 6, 2018.
What is chest physiotherapy?
This involves moving your body into different positions and using tapping motions, vibrations, or wearing a vibrating vest to help loosen and drain mucus. It’s generally used for obstructive or postsurgical atelectasis. This treatment is commonly used in people with cystic fibrosis as well.
How to reduce the risk of atelectasis?
Some research suggests that certain breathing exercises and muscle training may lower the risk of atelectasis after certain surgeries. By Mayo Clinic Staff.
How to prevent atelectasis in children?
Prevention. Atelectasis in children is often caused by a blockage in the airway. To decrease atelectasis risk, keep small objects out of reach of children. In adults, atelectasis most commonly occurs after major surgery. If you're scheduled for surgery, talk with your doctor about strategies to reduce your risk.
What is the most common respiratory complication after surgery?
Atelectasis is one of the most common breathing (respiratory) complications after surgery. It's also a possible complication of other respiratory problems, including cystic fibrosis, lung tumors, chest injuries, fluid in the lung and respiratory weakness. You may develop atelectasis if you breathe in a foreign object.
What is the term for a complete collapse of the lung?
Atelectasis (at-uh-LEK-tuh-sis) is a complete or partial collapse of the entire lung or area (lobe) of the lung. It occurs when the tiny air sacs (alveoli) within the lung become deflated or possibly filled with alveolar fluid.
Why does atelectasis occur after heart surgery?
A mucus plug is a buildup of mucus in your airways. It commonly occurs during and after surgery because you can't cough.
What are the complications of atelectasis?
The following complications may result from atelectasis: Low blood oxygen (hypoxemia). Atelectasis makes it more difficult for your lungs to get oxygen to the air sacs (alveoli). Pneumonia. Your risk for pneumonia continues until the atelectasis goes away. Mucus in a collapsed lung may lead to infection.
What causes nonobstructive atelectasis?
Possible causes of nonobstructive atelectasis include: Injury. Chest trauma — from a fall or car accident, for example — can cause you to avoid taking deep breaths (due to the pain), which can result in compression of your lungs. Pleural effusion.
How to treat atelectasis?
Atelectasis treatments include: Bronchoscopy to clear blockages like mucus. Medicine that you breathe in through an inhaler. Physiotherapy such as tapping on your chest to break up mucus, lying on one side or with your head lower than your chest to drain mucus, and exercises to help you breathe better.
What are the two types of atelectasis?
Types of Atelectasis. The two main types of atelectasis are obstructive (also called resorptive) and nonobstructive. Obstructive atelectasis happens when something physically blocks your airway. Types of nonobstructive atelectasis include: Relaxation or compressive.
What is it called when your airways don't expand?
What Is Atelectasis ? Atelectasis is a lung condition that happens when your airways or the tiny sacs at the end of them don’t expand the way they should when you breathe. Your lungs are where your body takes in oxygen and gets rid of carbon dioxide. When you breathe in, air flows into your windpipe, or trachea.
What is the name of the tube that separates the airways in the lungs?
When you breathe in, air flows into your windpipe, or trachea. The trachea splits into two channels called bronchi, and each bronchus goes to a lung. Inside your lungs, those airways divide again and again into smaller tubes called bronchioles. At the end of the smallest bronchioles are tiny sacs called alveoli.
What happens when air builds up in the lungs?
But if fluid or air builds up and separates them, your lungs can pull inward, and your alveoli can lose air. Depending on where this happens in your lung, it's either relaxation or compressive atelectasis. Adhesive. The fluid that lines the alveoli in your lungs has a material in it called pulmonary surfactant.
What is the tube that goes down your throat and into your airways?
A bronchoscope is a thin tube with a light and a camera that goes down your throat and into your airways. Oximetry or blood gas test. These measure how much oxygen is getting into your blood. Atelectasis Treatment and Recovery. If a tumor or another health condition is causing the problem, your doctor will treat it.
What is the sac at the end of the bronchioles?
At the end of the smallest bronchioles are tiny sacs called alveoli. Here, your blood dumps carbon dioxide and picks up fresh oxygen to carry to the cells in your body. When you breathe in and out, your lungs inflate and deflate like balloons.
How to get rid of atelectasis?
In cases of atelectasis, your physician may recommend: Percussion on the chest to loosen mucus plugs in the airway. Deep breathing exercises with an incentive spirometer. Removal of any blockages through bronchoscopy or another interventional pulmonology procedure.
Why do you need a chest tube for pneumothorax?
If a pneumothorax is large, your surgeon may need to place a chest tube between the ribs and into the space around the lungs in order to drain the air and let the affected lung (s) re-inflate. Depending on the severity of the pneumothorax, lung surgery may be necessary for treatment or even prevention of future collapses of the lung.
Can atelectasis heal on its own?
Atelectasis and Pneumothorax Treatments. Mild atelectasis or a small pneumothorax may heal, and the lung may re-inflate on its own. If not, there are a variety of techniques for clearing blockages, removing excess air and healing the lung.
How to treat atelectasis?
Treatment is typically restricted to dealing with the underlying condition that has actually caused the atelectasis to occur. Specific actions nevertheless, may be required to supply symptomatic relief. These include: 1 Lying down on the healthy side will enable the collapsed portion to re-expand under the impact of gravity. 2 Periodic changes of position while lying down. 3 Performing deep breathing exercises. The doctor might suggest the use of reward spirometry devices while performing these exercises. 4 If there is congestion of the bronchial passages, clapping on the chest areas might avoid the buildup of mucus plugs which can even more intensify the condition. 5 A bronchoscope might be used to clear the air passages of any accumulated mucus if needed.
What happens if you have atelectasis?
In case the atelectasis is severe, then the organs tend to be denied of oxygen and it can result in additional complications. Mild subsegmental atelectasis is a kind of atelectasis where the left lobe of the lungs gets affected. In this type, linear fissures appear on the lung and show up under chest X-rays.
What is gravity dependant atelectasis?
Of these various types of atelectasis, dependant atelectasis or gravity dependant atelectasis is a fairly benign kind of atelectasis that normally requires no treatment. It is caused by small areas of your lung being unable to broaden totally when you are lying down.
What is lung disease?
lung disorders like respiratory distress syndrome, lung cancer, chronic obstructive lung disease (when dependant atelectasis occurs in lung base), cystic fibrosis and in uncommon cases, even asthma. a physical obstruction like breathing in a peanut or a badly positioned ventilator tube.
What is it called when the lungs do not work?
When lungs do not operate at their best, organs start to get impacted since of the decline in oxygen being provided. Atelectasis is the condition when the lungs do not work effectively. Atelectasis is likewise known as a collapsed lung or partly collapsed lung.
What is atelectasis in lung?
The meaning of the term atelectasis implies a partial or total collapse of the lung resulting in a reduced lung capability. There are many different types of atelectasis. They are categorized as obstructive and non-obstructive atelectasis, depending upon the underlying cause.
What causes mucus to recede from the bottom of the lungs?
These generally include pain relievers, breathed in bronchodilators and acetylcysteine.

Overview
Symptoms
Causes
Risk Factors
Specialist to consult
Complications
Prevention
- Treatment of atelectasis depends on the cause. Mild atelectasis may go away without treatment. Sometimes, medications are used to loosen and thin mucus. If the condition is due to a blockage, surgery or other treatments may be needed.