
What are the surgical options for treatment of hydrocephalus?
Hydrocephalus is treated with one of two surgical options: A shunt (tube) is surgically inserted into the brain and connected to a flexible tube placed under the skin to drain the excess fluid into either the chest cavity or the abdomen so it can be absorbed by the body.
How to diagnose NPH?
Feb 01, 1942 · nonobstructive hydrocephalus: treatment by endoscopic cauterization of the choroid plexuses
Is there a cure for hydrocephalus?
Feb 05, 2016 · Because CSF dynamics are affected in obstructive forms of hydrocephalus, beginning in the 1950s and 1960s researchers have sought to treat hydrocephalus by reducing CSF production. Acetazolamide. Acetazolamide, a carbonic anhydrase inhibitor, decreases CSF flow and ICP in rabbits and cats [42–44]. This was initially thought to be a diuretic and …
How do you treat hydrocephalus?
Some individuals with non-communicating (obstructive) hydrocephalus can have a surgical procedure called an endoscopic third ventriculostomy (ETV). This surgery creates an opening to allow CSF to flow in and around the brain as it would …

What is non obstructive hydrocephalus?
Also known as non-obstructive hydrocephalus, communicating hydrocephalus occurs when the flow of cerebrospinal fluid (CSF) is blocked after it exits the ventricles. This form is called communicating because the CSF can still flow between the ventricles, which remain open.
How is non communicating hydrocephalus treated?
Some individuals with non-communicating (obstructive) hydrocephalus can have a surgical procedure called an endoscopic third ventriculostomy (ETV). This surgery creates an opening to allow CSF to flow in and around the brain as it would do under normal circumstances. Information you can trust!
Can hydrocephalus be treated without surgery?
There is currently no definitive cure. Most patients are managed by shunting using a silicone tube and valve system, where CSF is diverted from the cerebral ventricles to another body site [3].Feb 5, 2016
What is the latest treatment for hydrocephalus?
The current standard treatment for hydrocephalus is the surgical implantation of a shunt. A shunt redirects cerebrospinal fluid to another part of the body. This lets the brain's enlarged ventricles return to a more normal size in an effort to relieve the symptoms of hydrocephalus.
What is the difference between communicating and Noncommunicating hydrocephalus?
The word “communicating” refers to the fact that CSF can still flow between the ventricles, which remain open. Non-communicating hydrocephalus - also called obstructive hydrocephalus - occurs when the flow of CSF is blocked along one or more of the narrow passages connecting the ventricles.
What medication is commonly used to treat hydrocephalus?
Medication Summary Acetazolamide (ACZ) and furosemide (FUR) treat posthemorrhagic hydrocephalus in neonates. Both are diuretics that also appear to decrease secretion of CSF at the level of the choroid plexus. ACZ can be used alone or in conjunction with FUR.Jun 4, 2018
Can you treat hydrocephalus without a shunt?
An alternative procedure to shunt surgery is an endoscopic third ventriculostomy (ETV). Instead of inserting a shunt, the surgeon makes a hole in the floor of your brain to allow the trapped cerebrospinal fluid (CSF) to escape to the brain's surface, where it can be absorbed.
Who needs a VP shunt?
VP shunts are placed to treat hydrocephalus. Hydrocephalus (hi-droh-SEF-eh-less) happens when CSF does not drain out of the hollow spaces inside the brain (called ventricles) as it should. VP shunts drain the extra fluid and help prevent pressure from getting too high in the brain.
Will I always need a shunt?
New, long-term treatments using small endoscopes may eliminate the need for a shunt. All patients with hydrocephalus should be seen by a neurosurgeon at least every one to two years. Most people with Spina Bifida and shunted hydrocephalus will need the shunt for life.
What is non-communicating hydrocephalus?
Non-communicating hydrocephalus happens when the flow of CSF is blocked along one or more of the narrow passages connecting the ventricles. Two additional types of hydrocephalus include: Hydrocephalus ex-vacuo results from brain damage caused by stroke or injury.
What are the two types of hydrocephalus?
The two major types of hydrocephalus are called communicating hydrocephalus and non-communicating hydrocephalus. Communicating hydrocephalus occurs when the flow of CSF is blocked after it exits the ventricles. This form is called communicating because the CSF can still flow between the ventricles, the passages between which remain open.
Why do babies get hydrocephalus?
In these cases, hydrocephalus may be caused by: inherited genetic abnormalities that block the flow of CSF. developmental disorders such as those associated with birth defects in the brain, spine, or spinal cord.
What is the difference between CSF and hydrocephalus?
What is hydrocephalus? Hydrocephalus is an abnormal buildup of fluid in the ventricles (cavities) deep within the brain. This excess fluid causes the ventricles to widen, putting pressure on the brain’s tissues. Cerebrospinal fluid (CSF) is the clear, colorless fluid that protects and cushions the brain and spine.
Can hydrocephalus be fatal?
If left untreated, hydrocephalus can be fatal. Early diagnosis and successful treatment improve the chance for a good recovery. With the benefits of surgery, rehabilitative therapies, and educational interventions, many people with hydrocephalus live relatively normal lives.
Is hydrocephalus a developmental disorder?
Hydrocephalus is a relatively common developmental abnormality, but its underlying mechanisms are not well understood. NINDS supports a wide range of studies that explore the complex mechanisms of normal and abnormal brain development.
What is NINDS research?
NINDS is a component of the National Institutes of Health ( NIH ), the leading supporter of biomedical research in the world. NINDS conducts research and clinical studies to find better ways to prevent, treat, and ultimately cure disorders such as hydrocephalus.
What causes hydrocephalus?
Congenital hydrocephalus is caused by a birth defect or genetic disorder; acquired hydrocephalus has other causes, such as a hemorrhage, infection, or tumor. 1 Obstructive hydrocephalus is caused by an obstruction of CSF drainage by a tumor, congenital defect, or infection. 6 Most cases of hydrocephalus are obstructive.
How to tell if you have hydrocephalus?
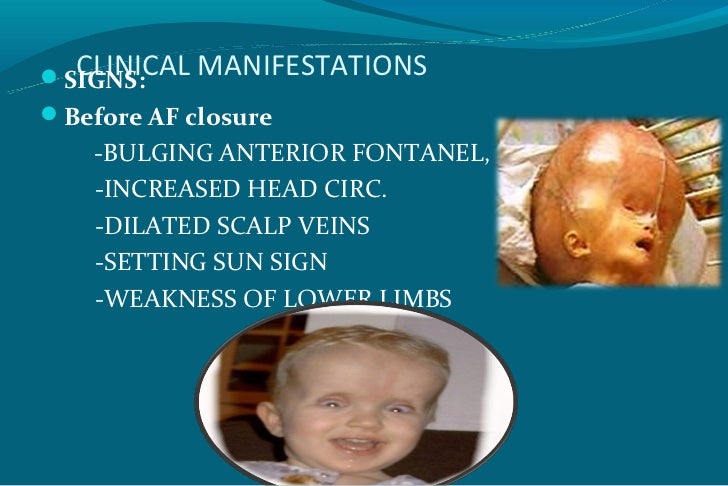
It is difficult to detect hydrocephalus because of its varied signs and symptoms, which commonly overlap with those of other diseases. Infants are likely to have a different disease progression from that of children and adults. Nausea and vomiting are common in infants and adults. In infants, fussiness and poor appetite are common indicators of hydrocephalus; however, the most prominent sign is a distended skull. 1,3 The sutures in infant skulls are soft and not fully developed, which allows them to expand upon increased pressure from CSF accumulation. 1,3 The increased intracranial pressure commonly causes headaches in adults and children, as their skull bones are not flexible. Difficulty with concentration and memory, a lack of balance, decreased bladder control, and a downward gaze are the most obvious signs in adults and children. 1
Where is the shunt placed for hydrocephalus?
Shunt Placement: As noted above, the standard treatment for hydrocephalus is shunt placement. Shunts are usually placed in the lateral ventricle and can have one of three different drainage points.
How can hydrocephalus be prevented?
A few of the causes of hydrocephalus can be prevented: To help avoid severe head injury, wear appropriate protective gear when participating in contact sports or other activities, such as skiing, riding a bike and sledding, with a risk of head trauma.
What causes hydrocephalus?
Obstructive (non-communicating) hydrocephalus is caused by a blockage in the system of cavities (ventricles) in the brain. The blockage prevents the cerebrospinal fluid from flowing (or "communicating") with the area that surrounds the brain and spinal cord (subarachnoid space), as it normally should. Blockages can be present at birth ...
What is the water on the brain called?
Hydrocephalus, also known as "water on the brain," is a condition in which there is extra cerebrospinal fluid around the brain and spinal cord. Cerebrospinal fluid acts as a cushion for the brain and spinal cord, supplies nutrients, and takes away waste products. Hydrocephalus can be present at birth (congenital) or can develop later (acquired).
How do you know if you have hydrocephalus?
The most common symptoms of hydrocephalus vary depending on the age of onset. In infants, symptoms include: A large head that is growing too rapidly. A bulging "soft spot" on top of head (anterior fontanelle) Irritability. Seizures. Delays in development. In older children and adults, symptoms include: Headache.
What is the most common type of hydrocephalus?
One of the most common types is aqueductal stenosis, which occurs because of narrowing of the aqueduct of Sylvius, a channel that connects two of the ventricles together. Non-obstructive (communicating) hydrocephalus results from problems with cerebrospinal fluid being produced or absorbed.
Can hydrocephalus cause brain damage?
The outlook depends on the cause of hydrocephalus and usually is better if the problem is diagnosed and treated early. If hydrocephalus gets worse rapidly or lasts a long time, it can cause brain damage and death. Children with hydrocephalus are more likely to have various developmental disabilities.
What is hydrocephalus associated with?
Hydrocephalus is associated with gradual destruction of periventricular white matter leading to a disconnection syndrome. In the circumstance of the immature brain, hydrocephalus also interferes with developmental processes including cell genesis and myelination [ 201, 230 ]. In the situation of progressive ventricular enlargement wherein shunt therapy is likely necessary, drugs might be used to protect the brain temporarily prior to shunting. Considering the overlap in pathophysiology between hydrocephalus, stroke, and trauma, it is anticipated that candidates from the latter two diseases should be considered for protecting the hydrocephalic brain. In neonatal hypoxic-ischemic brain injury, a variety of potential early therapeutics have broadly been categorized into anti-oxidative, anti-inflammatory, anti-apoptotic, and anti-excitotoxic mechanisms, with melatonin and erythropoietin covering multiple mechanisms [ 231 ]. Additional file 1: Table 1 summarizes the experiments conducted to date in hydrocephalic animals including the rationale, strengths, and weaknesses.
What is the brain damage caused by hydrocephalus?
A poorly studied aspect of hydrocephalus-associated brain damage is that due to disruption of the periventricular germinal matrix [ 269 ], which is the zone of proliferating cells that gives rise to neuron and glial precursors during human fetal life (or during the postnatal life of extremely premature infants).
What is the function of plasminogen activator?
Tissue plasminogen activator (tPA) is a serine proteinase that binds to fibrin in clotted blood and converts plasminogen to plasmin, thereby initiating fibrinolysis and dissolution of the blood clot. Urokinase (or urokinase-type plasminogen activator/uPA) is a proteolytic enzyme present in urine, blood, and extracellular matrix; it is also capable of activating plasminogen and it can digest extracellular matrix proteins [ 107 ]. Streptokinase is a bacterial enzyme capable of cleaving plasminogen, although it is less discriminate and can activate plasminogen that is not associated with blood clots [ 108 ]. Thrombolytic therapies for ischemic stroke were first pursued in the 1970s; intravascular recombinant tPA is an important intervention for some adults with early ischemic stroke [ 109 ]. However, tPA can have adverse effects in the brain parenchyma [ 110 ].
How is hydrocephalus modeled?
Hydrocephalus can be modeled in a wide range of animal species by injection of blood or kaolin into the CSF pathway, or by genetic manipulation [ 280 ]. Many of the models reflect the pathogenesis of hydrocephalus in human disorders. Several pharmacologic interventions appear to alleviate experimental hydrocephalus over relatively short terms (i.e. weeks). Manipulation of water balance or CSF production by osmotic agents or ion channel antagonists also works transiently in humans. However, poorly controlled clinical studies and rare randomized trials show no overall benefit in the management of hydrocephalic patients. CBF response to acetazolamide challenge appears to have a role as a test for predicting shunt responsiveness in adults with NPH. There may be some opportunity for revisiting acetazolamide with proper dosing in accordance with its pharmacodynamics or development of agents that more selectively inhibit the choroid plexus.
Who is Dr. Del Bigio?
Dr. Del Bigio holds the Canada Research Chair in Developmental Neuropathology (funded by the Canadian Institutes of Health Research). Mr. Di Curzio is funded by a studentship from Research Manitoba.
What is TGF beta?
Considering the marginal successes of blood lysis and anti-inflammatory agents for managing hydrocephalus, a more targeted molecular approach seems worth considering. Transforming growth factor beta (TGF-β) is a growth factor released from platelets at sites of blood clotting whereupon it regulates proliferation of fibroblasts (and other cell types), as well as the synthesis of extracellular matrix proteins. In 1994, high levels of TGF-β1 in the CSF of adults with subarachnoid hemorrhage were shown to be associated with enlargement of the cerebral ventricles [ 159, 160 ]. A similar association was later shown in premature infants with IVH [ 161, 162 ]. However, it must be noted that recent data obtained from a CSF assay study failed to support a critical role for TGF β1 and TGF β2 in the development of posthemorrhagic hydrocephalus in adults [ 163 ].
Does furosemide affect kidney function?
Furosemide is a diuretic agent that inhibits the Na–K–2Cl symporter located in the distal tubules of kidney. Furosemide has minimal effect on CSF formation in healthy cats and dogs [ 44, 68 ], but CSF formation was reduced in preterm rabbits and in adult rabbits, albeit much less potently than acetazolamide [ 69, 70 ]. Vinas mentioned use of furosemide in management of a hydrocephalic child [ 71 ]. Chaplin and coworkers claimed to have arrested the progression of hydrocephalus in 4/7 infants with posthemorrhagic hydrocephalus by repeated CSF drainage and administration of oral acetazolamide and furosemide [ 72 ]. Shinnar et al. [ 73] gave the drug combination to 49 hydrocephalic children; they reported a 57 % success rate (avoidance of shunt) in non-myelomeningocele patients but only 26 % success in infants with myelomeningocele. An uncontrolled trial conducted from 1982–86 also hinted at benefit [ 74, 75 ]. A randomized control trial of the acetazolamide/furosemide combination for premature infants with posthemorrhagic ventricular dilatation was conducted from 1992–96. Unfortunately it failed to show benefit [ 76 – 78 ]. This trial was criticized for its failure to prove a solid rationale and safety background before starting [ 79 ].
What is non-communicating hydrocephalus?
Non-communicating hydrocephalus, also known as obstructive hydrocephalus, occurs when the flow of CSF is blocked along one of or more of the narrow passages connecting the ventricles.
What causes hydrocephalus in the brain?
This type of hydrocephalus may result from a thickening of the arachnoid around the base of the brain , which blocks the flow of CSF from the spinal to the cortical subarachnoid spaces. CSF normally flows unrestricted through the ventricles and into the subarachnoid space.
What is the cause of communicating hydrocephalus?
Communicating hydrocephalus (non-obstructive hydrocephalus) is caused by inadequate reabsorption of CSF. The excessive accumulation of CSF results in an abnormal enlargement of the spaces in the brain called ventricles. This causes potentially harmful pressure on the tissues of the brain.
What is the water in the brain called?
Hydrocephalus was once known as “water” on the brain. The “water” is actually cerebrospinal fluid (CSF), a clear fluid surrounding the brain and spinal cord. The CSF protects the brain and spinal cord from injury by providing a liquid cushion, and is continually being produced, circulated and absorbed.
Is hydrocephalus a neurosurgeon?
However, neurosurgeons are often unfamiliar with the unique aspects of diagnosing communicating hydrocephalus in MPS and related diseases, creating a frustrating situation for parents. Hydrocephalus was once known as “water” on the brain.
Can hydrocephalus be a problem in MPS?
Communicating hydrocephalus (increased fluid in the ventricles of the brain) is a common, but often undiagnosed, problem in individuals with MPS I, MPS II, MPS VI and MPS VII and may be associated with some cortical atrophy (loss of brain cells). Children with greater neurological involvement have a greater risk of developing hydrocephalus. Early detection and treatment of hydrocephalus is believed to improve quality of life. However, neurosurgeons are often unfamiliar with the unique aspects of diagnosing communicating hydrocephalus in MPS and related diseases, creating a frustrating situation for parents.
What are the risk factors for hydrocephalus?
Risk Factors of Obstructive Hydrocephalus 1 The condition is most common in adults over the age of 60 or in young children; it is estimated that 1 in 500 children are affected by the condition. 2 It is also known to be a congenital condition, meaning it can be present at birth. 3 This will often stem from a genetic disorder, such as spina bifida. 4 In cases concerning the elderly, the hydrocephalus is usually due to an infection (such as meningitis), head injury or a brain tumor/cyst.
Why do elderly people get hydrocephalus?
In cases concerning the elderly, the hydrocephalus is usually due to an infection (such as meningitis), head injury or a brain tumor/cyst.
What are the symptoms of a symtom?
Other symptoms which are noticeable in both children and adults are nausea, headaches, poor coordination and loss of concentration. Adults may also experience impaired vision, vomiting and bladder control problems.
How common is a syphilis in children?
The condition is most common in adults over the age of 60 or in young children; it is estimated that 1 in 500 children are affected by the condition.
Where is CSF stored?
CSF is produced and stored in ventricles before being absorbed into the bloodstream via the venous system. If the CSF pathways become obstructed or damaged, CSF can accumulate within the ventricular system, which can cause the ventricles to dilate and the cerebral mantle to thin and stretch. When this happens, the condition is known as obstructive ...
Can hydrocephalus be seen in adults?
Symptoms of obstructive hydrocephalus can be seen in both adults and kids, but they are often more visually noticeable in infants. Because infants' skulls are not fully developed, the buildup of fluid can cause their head to enlarge.
How early can you treat hydrocephalus?
Early treatment (before age 4 months) is important to help limit or prevent brain damage. However, congenital hydrocephalus is now often diagnosed before birth through a routine ultrasound. Treatment focuses on reducing the amount of fluid in the brain to relieve pressure.
What is non-communicating hydrocephalus?
Non-communicating hydrocephalus — also called obstructive hydrocephalus — occurs when the flow of cerebrospinal fluid (CSF) is blocked along one or more of the narrow passages connecting the ventricles.
Why is communicating hydrocephalus called communicating?
Also known as non-obstructive hydrocephalus, communicating hydrocephalus occurs when the flow of cerebrospinal fluid (CSF) is blocked after it exits the ventricles. This form is called communicating because the CSF can still flow between the ventricles, which remain open.
What are the two types of hydrocephalus?
Types of Hydrocephalus. There are two main classifications for hydrocephalus: Communicating (or non-obstructive) Non-communicating (or obstructive) Both communicating and non-communicating hydrocephali can be subdivided into congenital (present at birth) and acquired (occurs following birth). Communicating hydrocephalus can also be subdivided ...
How does NPH develop?
It may develop after a stroke or injury. As opposed to other types of hydrocephalus, NPH develops slowly due to the gradual blocking of CSF drainage, which subsequently causes slow fluid buildup over time. The enlarged ventricles then press on the brain and cause symptoms. These include dementia-like signs similar to Alzheimer’s disease, and walking difficulties that resemble Parkinson’s disease. That’s why the diagnosis is often problematic. The good news, however, is that unlike those conditions, NPH can be resolved.
How does congenital hydrocephalus affect a newborn?
Congenital hydrocephalus is a buildup of excess cerebrospinal fluid (CSF). The extra fluid can increase pressure in the baby’s brain , which then causes brain damage and physical as well as mental problems. Discovering the condition early and treating it quickly can help limit any long-term problems. But long-term effects greatly depend on the cause of the fluid buildup, how bad it gets, and how the baby responds to treatment. Early treatment (before age 4 months) is important to help limit or prevent brain damage. However, congenital hydrocephalus is now often diagnosed before birth through a routine ultrasound. Treatment focuses on reducing the amount of fluid in the brain to relieve pressure.
What causes hydrocephalus ex-vacuo?
Hydrocephalus ex-vacuo occurs from brain damage caused by stroke or injury. In this condition, there may be an actual shrinkage of brain substance. Although there is more cerebrospinal fluid (CSF) than usual, and the ventricles are enlarged, the CSF pressure may or may not be elevated in hydrocephalus ex-vacuo.
Classification
- A diagnosis of hydrocephalus is usually based on: 1. Your answers to the doctor's questions about signs and symptoms 2. A general physical exam 3. A neurological exam 4. Brain-imaging tests
Detection and Diagnosis
Treatment Options
Long-Term Prognosis
Conclusion
- It is difficult to detect hydrocephalus because of its varied signsand symptoms, which commonly overlap with those of other diseases.Infants are likely to have a different disease progression from that ofchildren and adults. Nausea and vomiting are common in infants andadults. In infants, fussiness and poor appetite are common indicators ofhydrocephalus; however, the most promin…
What Is Hydrocephalus?
- Although many causes of hydrocephalus exist, the number of treatmentsis limited. All successful, long-term treatments are surgical. There islittle use for medication in hydrocephalus. In some acquired cases, aswith tumors and infections, resolving the underlying condition willresolve the hydrocephalus, but most patients still require surgicalinterv...
Symptoms
- The treatment of hydrocephalus requires long-term care and lifelongfollow-up. This is especially true for children and neonates whosehydrocephalus has a congenital cause. Even after appropriate placementof a shunt, annual neurologic visits are required.11Complications, including shunt collapse, infection, and occlusions, cancause a rise in CSF pressure that may lead to sym…
Diagnosis
- Hydrocephalus is a complicated condition to diagnose, and treatmentoptions are limited. Current long-term treatment options are restrictedto surgical interventions, including shunt placement and ETV. Even ifthe underlying disease state, such as an infection or tumor, isresolved, most patients will require surgical intervention and long-termfollow-up.
Expected Duration
Prevention
Treatment
When to Call A Professional
Prognosis
Further Information
- Treatment of hydrocephalus depends on its cause and the severity. Occasionally, medications are used to slow the rate of cerebrospinal fluid production temporarily. However, this has not been successful for long-term treatment. Most cases require drainage of the excess fluid. A tube called a shunt is inserted into one of the cavities in the brain t...