Explore
Follow the ACLS Pulseless Arrest Algorithm for asystole: Check the patient's rhythm, taking less than 10 seconds to assess. Verify the presence of asystole in at least two leads. Resume CPR at a compression rate from 100-120 per minute. As soon as IV …
Which intervention is most appropriate for the treatment of a patient in asystole?
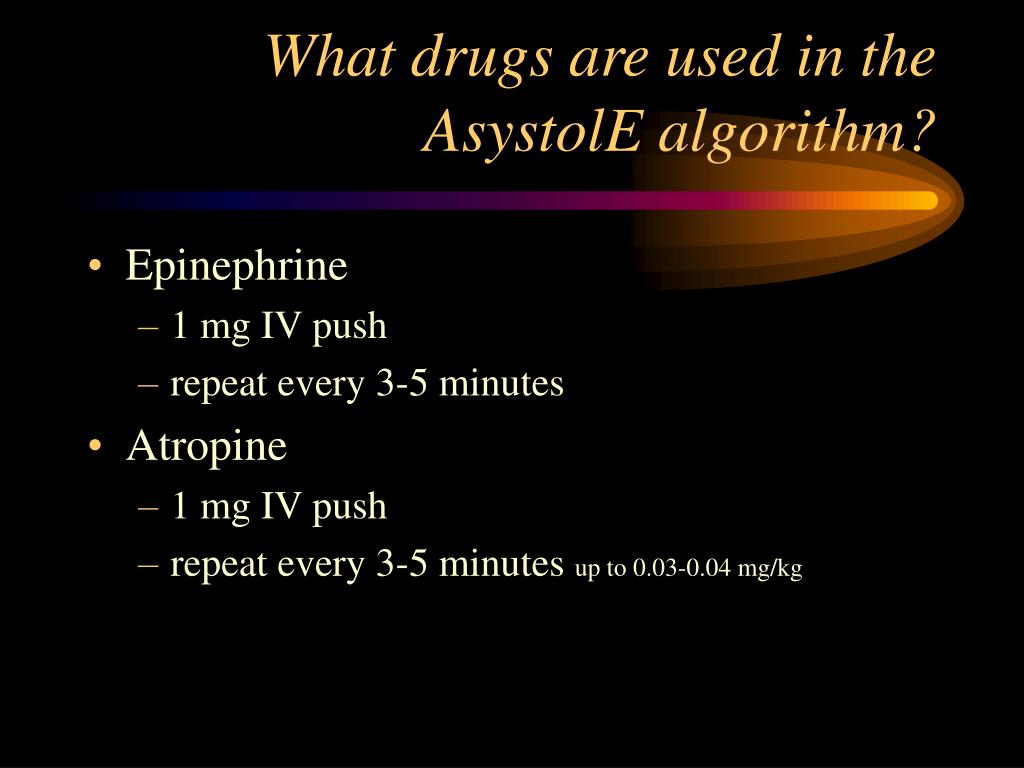
When treating asystole, epinephrine can be given as soon as possible but its administration should not delay initiation or continuation of CPR. After the initial dose, epinephrine is given every 3-5 minutes. Rhythm checks should be performed after 2 minutes (5 cycles) of CPR.
What is asystole and why should I worry about it?
For asystole, the standard medication to use is epinephrine. While treating asystole, epinephrine should be administered as soon as possible without delaying the start or continuation of CPR. Following the initial dose, epinephrine is given every 3-5 minutes as needed. During CPR, a rhythm check should be done every 2 minutes (5 cycles).
Can You shock a patient in asystole?
Asystole is treated by cardiopulmonary resuscitation (CPR) combined with an intravenous vasopressor such as epinephrine (a.k.a. adrenaline). Can you recover from asystole? Resuscitation is generally successful in cases of cardiac arrest due to choking on food or due to pacemaker failure.
Should we shock patients in asystole?
Feb 04, 2020 · Asystole is treated by cardiopulmonary resuscitation (CPR) combined with an intravenous vasopressor such as epinephrine (a.k.a. adrenaline). Sometimes an underlying reversible cause can be detected and treated (the so-called "Hs …
What is the treatment for asystole?
What is the first treatment for asystole?
Which intervention is most appropriate for the treatment of a patient in asystole ?'?
What is the ACLS protocol for asystole?
CPR needs to be initiated first. Asystole is not a shockable rhythm and treatment for Asystole involves high quality CPR, airway management, IV or IO therapy, and medication therapy which is 1mg epinephrine 1:10,000 every 3-5 minutes rapid IV or IO push.
When is it recommended to administer epinephrine to a patient with asystole?
Administer first dose at the onset of cardiac resuscitation.Mar 24, 2010
How is asystole diagnosis?
What is the most appropriate action when you view a patient with ventricular fibrillation?
Can you do CPR on asystole?
Why defibrillation is not recommended in asystole?
How is SVT ACLS treated?
- Attempt vagal maneuvers.
- If unsuccessful, administer adenosine 6 mg IV bolus followed by a rapid normal saline flush.
- If unsuccessful, administer adenosine 12 mg IV bolus followed by a rapid normal saline flush.
How is V-tach ACLS treated?
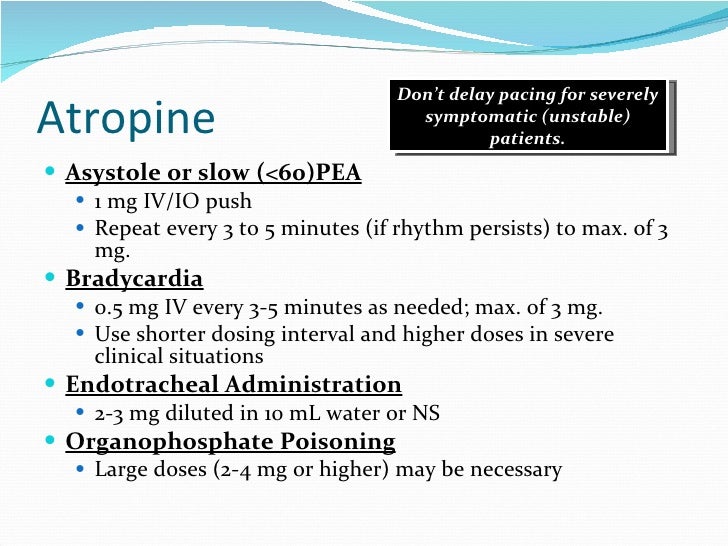
Is atropine used for asystole?
What is the definition of asystole?
Asystole is defined as a cardiac arrest rhythm in which there is no discernible electrical activity on the ECG monitor. Consequently, it is sometimes referred to as a “flat line.” Confirmation that a “flat line” is truly asystole is an important step in the ACLS protocol.
Which branch of the cardiac arrest algorithm is used for asystole?
Asystole is treated using the right branch of the Cardiac Arrest Algorithm. Click below to view the Cardiac Arrest Algorithm diagram. When done click again to close the diagram.
Why should ACLS be reviewed?
The H’s and T’s of ACLS should be reviewed to identify any underlying cause that could have precipitated the asystole. Some of the most common reasons to stop or withhold resuscitative efforts are: Asystole is treated using the right branch of the Cardiac Arrest Algorithm.
Is asystole a good outcome?
Asystole for many patients is the result of a prolonged illness or cardiac arrest, and prognosis is very poor. Few patients will likely have a positive outcome and successful treatment of cardiac arrest with asystole will usually involve the identification and correction of an underlying cause of the asystole.
What is the best medicine for asystole?
For asystole, the standard medication to use is epinephrine.
What is an asystole?
Asystole, otherwise known as a flatline, is a state of cardiac standstill in which all electrical activity has ceased.
What does it mean when you have apparent asystole?
Apparent asystole may be the result of a user or technical error. If you believe the rhythm may be incorrect, ensure patches have good contact with the individual, leads are connected, the gain is set appropriately, and the power is on.
Is defibrillation effective for asystole?
Because asystole is not a shockable rhythm, defibrillation is not an effective asystole treatment. Researchers estimate that less than two percent of people who suffer asystole outside of the hospital will survive - even with trained emergency intervention.
Is asystole a flatline?
Identifying Asystole. Confirmation that the rhythm is indeed a flatline, and not a false positive, is an important part of the asystole treatment algorithm. For most patients, true asystole is the result of a prolonged illness or cardiac arrest, and prognosis is very poor.
What is the treatment for asystole?
Asystole is treated by cardiopulmonary resuscitation (CPR) combined with an intravenous vasopressor such as epinephrine (a.k.a. adrenaline).
Is PEA shockable?
If the patient is in asystole or PEA, this is NOT a shockable rhythm.
What is the treatment for asystole?
Asystole is treated by cardiopulmonary resuscitation (CPR) combined with an intravenous vasopressor such as epinephrine (a.k.a. adrenaline). Sometimes an underlying reversible cause can be detected and treated (the so-called "Hs and Ts", an example of which is hypokalaemia).
What is the treatment for bradycardia?
Bradycardia with poor perfusion can be life-threatening in some cases. Initial treatment includes airway support to make sure the patient is ventilating adequately .
How many people survive asystole?
That’s a machine that uses an electric pulse to get your heartbeat back to normal. But it doesn’t usually help in real life. Typically, less than 2% of people survive asystole. Your odds depend on what causes your heart to stop.
What is asystole in medical terms?
Medically Reviewed by James Beckerman, MD, FACC on February 11, 2020. Asystole (ay-sis-stuh-lee) is when there’s no electricity or movement in your heart. That means you don’t have a heartbeat. It’s also known as flatline.
What causes asystole in the body?
But some conditions raise your chances of it happening early. One of them is certain types of arrhythmia, or irregular heartbeat. A heart injury or genetics -- something that runs in your family -- could also lead to asystole.
Can a VFIB cause asystole?
This is cardiac arrest. Ventricular arrhythmias that may lead to asystole are: Ventricular fibrillation. With VFib, the lower chambers tremble, or fibrillate, instead of contracting normally. If it’s not treated within a few minutes, you can die. Your chances of VFib are higher if you: Have a weak heart muscle ( cardiomyopathy)
What is the best medicine for asystole?
The only two drugs recommended or acceptable by the American Heart Association (AHA) for adults in asystole are epinephrine and vasopressin. Atropine is no longer recommended for young children and infants since 2005, and for adults since 2010 for pulseless electrical activity (PEA) and asystole.
How to prevent primary asystole?
Primary asystole may be prevented by the appropriate use of a permanent pacemaker in those patients who have high-grade heart block or sinus arrest. Prevention of secondary asystole requires early recognition and treatment of the preceding event.
What is the appropriate disposition for the occasional patient who survives bradyasystolic cardiopulmonary arrest
The intensive care unit is the appropriate disposition for the occasional patient who survives bradyasystolic cardiopulmonary arrest and requires further treatment and diagnostic evaluation. In the past decade, survivors who achieved electrical and hemodynamic stability but remained comatose and were modestly cooled to 32-34°C for the first 24 hours showed improvement in overall neurologic outcome. [ 24] The studies were conducted on prehospital arrests with ventricular fibrillation as the presenting rhythm, but results could be generalized to bradyasystolic survivors. [ 24]
What is the mainstay of treatment in the emergency department?
Mainstays of treatment in the emergency department are providing oxygenation and ventilation via endotracheal intubation and circulation via cardiopulmonary resuscitation (CPR), attempts at transcutaneous or transvenous pacing (that have some small potential to be fruitful in primary asystole that has just occurred), and administration of pharmacologic agents.
How many patients survived asystole?
Of the 528 patients with asystole in the study, 12 patients in the vasopressin group survived to discharge compared with 4 in the standard therapy group. [ 19] In this study, the odds ratio stated may not be statistically significant, and there was also a nonstatistically significant trend toward worse results for ventricular fibrillation (VF) and PEA. [ 19]
Can you use a defibrillator in asystole?
Electrical defibrillation should not be applied indiscriminately to the patient in asystole. This is not only fruitless, but also detrimental, eliminating any possibility of recovering a rhythm. Asystole following electrical defibrillation has an even worse outcome than that in a patient whose first documented rhythm was asystole. [ 23] One caution is that, following defibrillation, a brief spurious asystole can occur using manual monitoring through the defibrillator paddles. This does not occur with the rhythm monitoring leads or hands-off monitor pads. If not taken into consideration, it could lead to a delay in defibrillation, when indeed VF is present.
What is the treatment for asystole?
Asystole is not a shockable rhythm and treatment for Asystole involves high quality CPR, airway management, IV or IO therapy, and medication therapy which is 1mg epinephrine 1:10,000 every 3-5 minutes rapid IV or IO push.
Is asystole a shock?
Asystole is not a shockable rhythm and treatment for Asystole involves high quality CPR, airway management, IV or IO therapy, and medication therapy which is 1mg epinephrine 1:10,000 every 3-5 minutes rapid IV or IO push.
Is asystole a shockable rhythm?
Asystole is not a shockable rhythm. So, treatment will involve high-quality CPR, airway management, IV or IO therapy, and medication therapy – specifically 1mg of epinephrine 1:10,000 concentration every 3 to 5 minutes via rapid IV or IO push.
Can asystole be reversed?
It is rare for asystole to be reversed, especially after a long duration. If the patient does not respond to the BLS and ACLS treatments, the rescue team will need to decide when to stop resuscitative efforts. If there is a high degree of certainty that the patient will not respond to further ACLS interventions, it would be appropriate to stop.