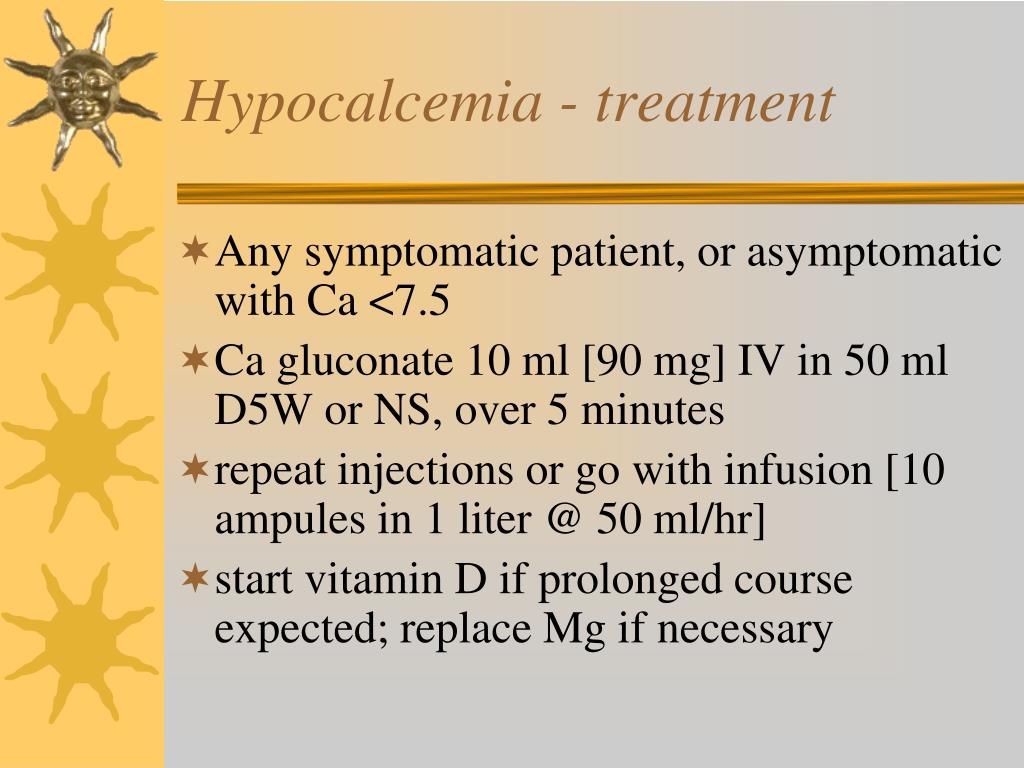
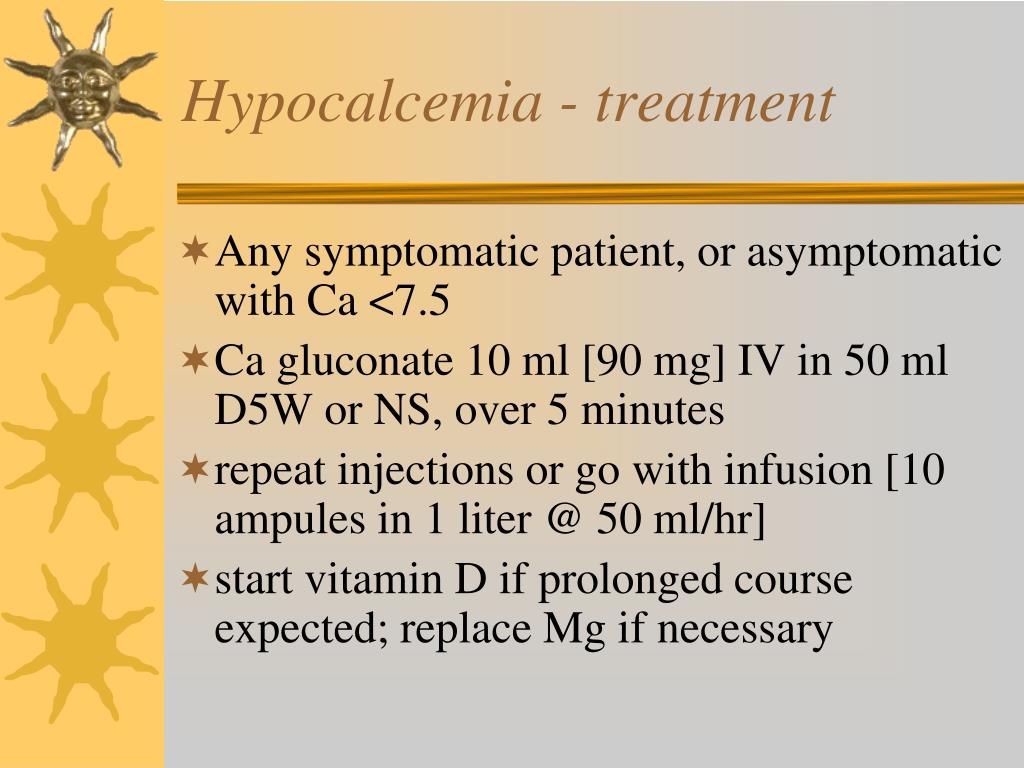
In patients with acute symptomatic hypocalcemia, intravenous (IV) calcium gluconate is the preferred therapy, whereas chronic hypocalcemia is treated with oral calcium and vitamin D supplements. The treatment of hypocalcemia will be reviewed here.
Full Answer
Which medications are used in the treatment of hypercalcemia?
- Close monitoring of the calcium level
- Referral to surgery to have the overactive gland (s) removed
- Starting a medication such as cinacalcet (Sensipar®), which is used to manage hypercalcemia
- Using bisphosphonates, osteoporosis drugs given intravenously (with a needle through the veins) that treat hypercalcemia due to cancer
What are the treatment options for hypocalcemia?
- Ionized calcium
- 24-hour urinary phosphate, calcium, magnesium, and creatinine
- 1,25-dihydroxyvitamin D
- Renal ultrasonography to assess for nephrolithiasis
- DNA sequencing to exclude genetic mutations
- Biochemistry in first-degree family members
Is there a cure for hypocalcemia?
Glucose gel in infants at risk for transitional neonatal hypoglycemia. Am J Perinatol. 2018;35:1050–6. Weston PJ, Harris DL, Harding JE. Dextrose gel treatment does not impair subsequent feeding. Arch Dis Child Fetal Neonatal Ed. 2017;102:F539–41.
What is the prognosis for a patient with hypercalcemia?
The results of treatment for hypercalcemia depend on the underlying cause of the condition. If hypercalcemia is seen in the presence of cancer, the average 30-day survival rate is about 50%. The prognosis is excellent for many of the other causes of hypercalcemia provided the underlying cause is addressed and treated.
How do you fix severe hypocalcemia?
In patients with acute symptomatic hypocalcemia, intravenous (IV) calcium gluconate is the preferred therapy, whereas chronic hypocalcemia is treated with oral calcium and vitamin D supplements.
What level is severe hypocalcemia?
Severe hypocalcemia, defined by a serum calcium <1.9 mmol/L (7.6 mg/dL), is often considered an emergency because of a potential risk of life-threatening cardiac arrhythmias or seizures (6, 7, 8, 9, 10, 11).
What is the first line treatment for hypocalcemia?
In the emergency department, magnesium and calcium (in their many different forms) are the only medications necessary to treat hypocalcemic emergencies.
When should hypocalcemia be corrected?
Patients with severe symptoms of hypocalcemia such as carpopedal spasm, tetany, seizures, decreased cardiac function, or prolonged QT interval need IV calcium replacement to rapidly correct their hypocalcemia. Treat all asymptomatic patients with an acute decrease in serum corrected calcium to ≤7.5 mg/dL (1.9 mmol/L).
What is a critical calcium level?
Although serum calcium levels above 11.5 mg/dL commonly cause symptoms, patients may be asymptomatic at this level. Critical levels are reached above 12 mg/dL, with levels above 15 mg/dL (severe hypercalcemia) being a medical emergency.
How long does it take to treat hypocalcemia?
The onset of action is approximately two weeks, with effects persisting for up to several months, so levels may be checked and doses adjusted every 1-3 months. Calcitriol (1,25 dihydroxy vitamin D) does not require hydroxylation in the liver or the kidney, so it is often used in patients with renal failure.
When do you give IV calcium for hypocalcemia?
Severe symptomatic hypocalcemia (seizure, laryngospasm, tetany): 1 to 2 grams of calcium gluconate should be administered in 10 minutes and repeated in 10 to 60 minutes until symptoms resolve.
Which of the following drugs may be prescribed to treat hypocalcemia?
Drugs used to treat HypocalcemiaDrug nameRatingRx/OTCView information about calcium chloride calcium chlorideRateRxGeneric name: calcium chloride systemic Drug class: minerals and electrolytes For consumers: dosage, interactions, side effectsView information about Natpara NatparaRateRx54 more rows
How much does calcium gluconate raise calcium?
As a guideline, the total calcium will increase by 0.5 mg/dl for every gram of calcium gluconate given intravenously. MAXIMUM CONCENTRATIONS: Calcium gluconate: 1 gm in 50 ml D5W or NS.
When do you calculate corrected calcium?
Thus, the calcium level should be corrected in patients with low serum albumin levels, using the following formula: Corrected calcium (mg/dL) = measured total Ca (mg/dL) + 0.8 (4.0 - serum albumin [g/dL]), where 4.0 represents the average albumin level.
What is normal corrected calcium level?
Normal calcium levels in a healthy adult should fall between 8.8-10.5 in mg/dL and 2.25-2.625 in mmol/L. A lower than normal calcium level is called hypocalcemia, while the state of higher than usual calcium levels is known as hypercalcemia.
What is the difference between calcium and corrected calcium?
Interpretation of total calcium results should always include due consideration of serum albumin concentration. Whichever formula is used, "corrected" calcium is an estimate of the total calcium concentration, had serum protein (albumin) concentration been normal.
What is the best treatment for hypocalcemia?
Thus, the management of hypocalcemia depends upon the severity of symptoms. In patients with acute symptomatic hypocalcemia, intravenous (IV) calcium gluconate is the preferred therapy, whereas chronic hypocalcemia is treated with oral calcium and vitamin D supplements. The treatment of hypocalcemia will be reviewed here.
Is hypocalcemia a life threatening condition?
Hypocalcemia may be associated with a spectrum of clinical manifestations, ranging from few (if any) symptoms if the hypocalcemia is mild and/or chronic to severe life-threatening symptoms if it is severe and/or acute. Thus, the management of hypocalcemia depends upon the severity of symptoms.
Is calcium ionized or free?
As a result, ionized calcium remains the gold standard for assessing calcium status, ...
Is ionized calcium a gold standard?
As a result, ionized calcium remains the gold standard for assessing calcium status, particularly if the diagnosis of hypocalcemia is in doubt, due to hypoalbuminemia, atypical or absent symptoms, or a minimally reduced serum calcium concentration. However, ionized calcium is not performed routinely, because it is more costly ...
What blood test is used to diagnose hypocalcemia?
Definitive diagnosis of hypocalcemia requires a blood test for calcium. Calcium is a common blood test often performed with other tests as part of a basic metabolic panel ( BMP) or a complete metabolic panel ( CMP ). Calcium is usually first assessed through a total calcium blood test.
Why is my calcium level low?
Some of the reasons for this include injury to the parathyroid gland from surgery or radiation treatment, autoimmune disease, or a genetic disease leading to low PTH.
What hormones increase calcium levels?
For example, if your calcium levels are too low, your parathyroid glands will normally release parathyroid hormone (PTH). This hormone works to increase your calcium in different ways, like reducing the amount of calcium released in your urine. Normally, the action of PTH brings the calcium back into a normal range.
Why is calcium important for the heart?
Because of this, your body works to tightly regulate the amount of calcium present in your blood. If it’s too high, it tries to bring it down; if it’s too low, it tries to bring it up.
Where is calcium found in the body?
Most people know that calcium is a component of your bones. But calcium is also found in your blood and inside your body’s cells. In fact, calcium is involved in many important biological processes. For example, it plays roles in blood clotting and in helping certain enzymes to function.
Can magnesium cause hypocalcemia?
For example, abnormal levels of the electrolytes magnesium and phosphate might indirectly cause hypocalcemia. Some other less common causes of hypocalcemia include pancreatitis and cancer which has spread to the bones. 2 . A number of drugs sometimes cause hypocalcemia as a side effect.
Can you take calcium supplements if you have low calcium?
People who have calcium that is not as low can usually take oral calcium supplements instead. You may need to take these over a long period of time. Vitamin D is also often a key component of treatment. Depending on the situation, you might need to take other substances important for calcium metabolism, like magnesium.
Causes of Hypocalcemia
Usually, hypocalcemia happens when large amounts of calcium are put out when you urinate, or too little calcium enters your blood from your bones. This could be caused by certain genetic factors, vitamin deficiencies, or other conditions.
Testing
The way to find out whether or not you have hypocalcemia is by taking a blood test. This test will be able to find out whether or not you have hypocalcemia. It can also help tell you whether or not it is caused by your kidneys or parathyroid.
Treatment
If you simply just have hypocalcemia, usually vitamin C or vitamin D supplementation is all you need to treat it and take away any symptoms. Usually, if symptoms of hypocalcemia spontaneously happen, your provider will give you intravenous (IV) supplementation.
What medications are used to treat elevated calcium levels?
medications, such phenytoin, phenobarbital, rifampin, corticosteroids, and drugs used to treat elevated calcium levels. pancreatitis. hypermagnesemia and hypomagnesemia.
How long does it take for hypocalcemia to occur?
Neonatal hypocalcemia occurs in infants soon after birth. Most cases of neonatal hypocalcemia occur within the first two days after birth. But late onset hypocalcemia can occur three days after birth, or later.
What is the normal calcium level?
Normal calcium levels for adults can range from 8.8 to 10.4 milligrams per deciliter (mg/dL), according to the Merck Manual. You may be at risk for calcium deficiency disease if your calcium level is below 8.8 mg/dL. Children and teens typically have higher blood calcium levels than adults.
Why is calcium important during menopause?
During menopause, women should also increase their calcium intake to reduce the risk of osteoporosis and calcium deficiency disease.
What does a doctor measure for calcium deficiency?
Your doctor will measure your total calcium level, your albumin level, and your ionized or “free” calcium level. Albumin is a protein that binds to calcium and transports it through the blood. Sustained low calcium levels in your blood may confirm a diagnosis of calcium deficiency disease.
How to prevent calcium deficiency?
Be aware that foods high in calcium, such as dairy products, can also be high in saturated fat and trans fat. Choose low-fat or fat-free options to reduce your risk of developing high cholesterol and heart disease.
Why is calcium important?
Calcium is a vital mineral. Your body uses it to build strong bones and teeth. Calcium is also needed for your heart and other muscles to function properly. When you don’t get enough calcium, you increase your risk of developing disorders like: osteoporosis. osteopenia.
What medications are used for hypocalcemia?
In the emergency department, magnesium and calcium (in their many different forms) are the only medications necessary to treat hypocalcemic emergencies.
Why is hypocalcemia important?
Hypocalcemia generally results from another disease process. Awareness of the diseases that cause hypocalcemia is important so that the cause can be identified and managed early. Most hypocalcemic emergencies are mild and require only supportive treatment and further laboratory evaluation. On occasion, severe hypocalcemia may result in seizures, ...
What are the symptoms of hypocalcemia?
Patients with chronic hypocalcemia should be educated about the early symptoms of hypocalcemia, such as paresthesias and muscle weakness, so that they can obtain care before more severe symptoms develop. Given the variety of causes that hypocalcemia may have, multiple consultations may be necessary.
Is IV replacement necessary for hypocalcemia?
Check ionized calcium and other pertinent screening laboratory tests. IV replacement is recommended in symptomatic or severe hypocalce mia with cardiac arrhythmias or tetany.
Does vitamin D help with calcium absorption?
Active vitamin D (calcitriol) enhances the absorption of calcium. Finally, the calcium in the dialysate bath can be increased. Nutritional vitamin D deficiency from lack of sunlight exposure or poor oral intake of vitamin D responds to treatment with ultraviolet light or sunlight exposure. [ 49] .
Is calcium chloride 10% intravenously?
Caution should be used when giving calcium chloride intravenously. Calcium chloride 10% solution delivers higher amounts of calcium and is advantageous when rapid correction is needed, but it should be administered via central venous access.
Is an internist appropriate for hypocalcemia?
Although uncommon, outpatient evaluation by an endocrinologist or an internist is appropriate in some patients who present to the ED with hypocalcemia. Patients with diseases that predispose them to the development of hypocalcemia should have scheduled appointments with an outpatient provider. Previous. Medication.
What is the best treatment for hypocalcemia?
Intravenous calcium infusion is essential to raise calcium levels and resolve or minimize symptoms in the setting of acute hypocalcemia. Oral calcium and/or vitamin D supplementation is the most frequently used as treatment of chronic hypocalcemia.
What is the calcium level of hypocalcaemia?
Calcium is essential for muscle contraction and neurotransmitter release, but clinical manifestations of hypocalcaemia (serum calcium level <8 mg/dl; 2.12 mmol/L) may involve almost any organ and system and may range from asymptomatic to life-threating conditions.
What is the best way to bring calcium levels back to normal?
Medicines will be given to bring your calcium and vitamin D levels back to normal. You may also need medicines to prevent bone loss. Take your medicine as directed. Contact your healthcare provider if you think your medicine is not helping or if you have side effects.
How often should I check my calcium levels?
Follow up with your doctor or endocrinologist every 3 to 6 months, or as directed: You will need to return to have your calcium levels checked. Bring a list of any questions you have so you remember to ask them during your visits.
What foods can you eat to get calcium?
Eat foods rich in calcium: Foods that contain calcium include milk, yogurt, cereals, and cheese. Leafy green vegetables, oranges, canned salmon, shrimp, and peanuts also contain calcium. Do not have caffeine or alcohol. These can slow your body's ability to absorb calcium.
What does it mean when your body loses too much calcium?
WHAT YOU NEED TO KNOW: Hypocalcemia is a low level of calcium in your blood. It occurs when your body loses too much calcium or does not absorb enough from the foods you eat.