Disorders and Drugs Associated with Acute Febrile Neutrophilic Dermatosis
| Classification | Disorder/Drug |
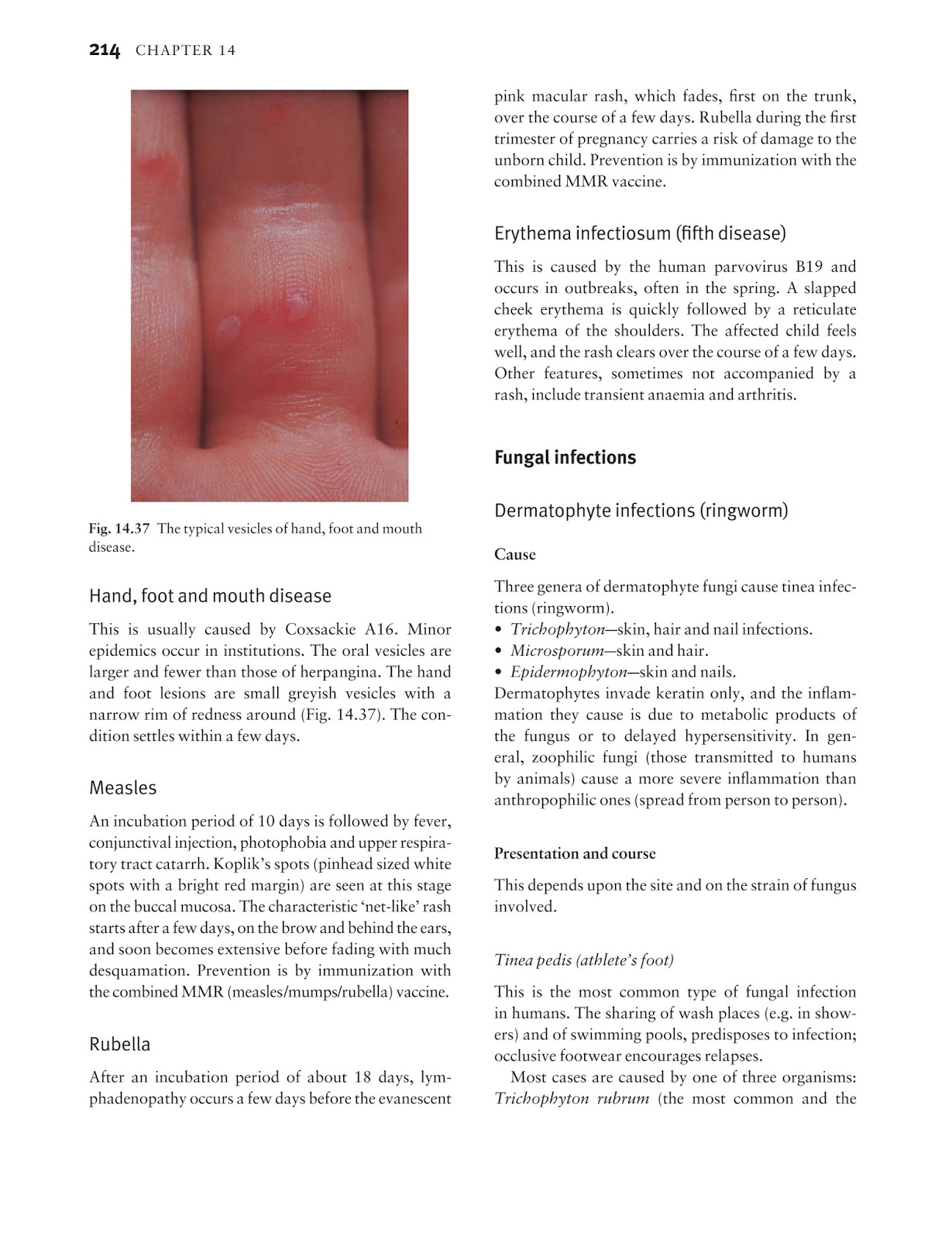
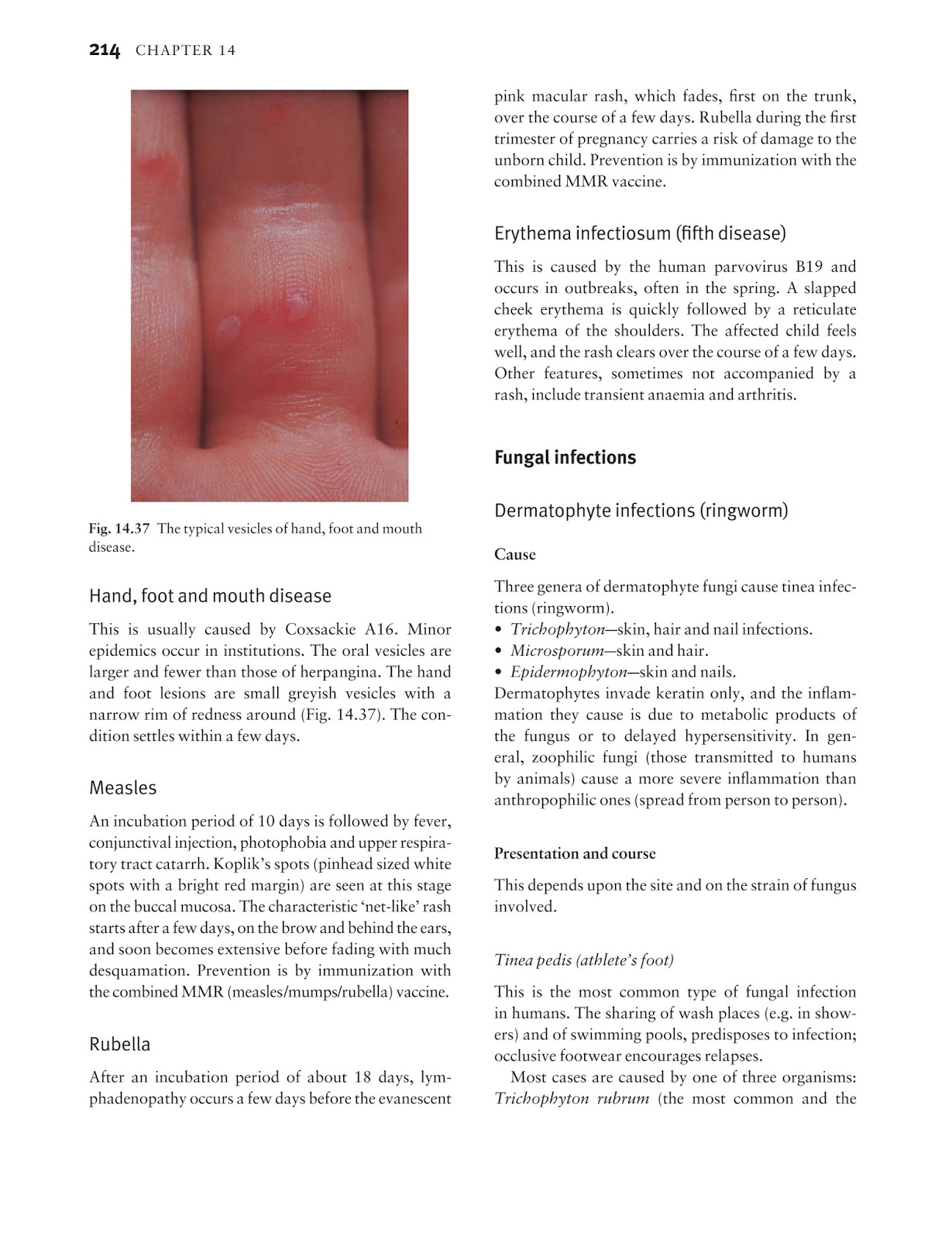
| Classical | Acute respiratory illness Gastrointestin ... |
| Cancer-associated | Acute myeloid leukemia Acute Myeloid Leu ... |
| Drug-induced | Granulocyte colony-stimulating factor (G ... |
Full Answer
What are neutrophilic dermatoses?
Sweet syndrome, pyoderma gangrenosum, and subcorneal pustular dermatosis are neutrophilic dermatoses - conditions that have an inflammatory infiltrate consisting of mature polymorphonuclear leukocytes. The neutrophils are usually located within the dermis in Sweet syndrome and pyoderma gangrenosum; …
What are the treatment options for neutrophilic dermatosis associated with rheumatoid arthritis?
NUD often occurs in a setting of underlying systemic disease. The most commonly associated diseases are adult-onset Still's disease, Schnitzler syndrome, lupus erythematosus and cryopyrin-associated periodic syndromes. Treatment of NUD depends on the clinical context. Dapsone and colchicine are often effective.
What tests are used to diagnose neutrophilic dermatosis?
Feb 01, 2021 · The exact cause of acute febrile neutrophilic dermatosis often isn't known. It is suspected that it can be a reaction of the body to certain exposures (sun), infections ( Streptococcus bacteria , C ampylobacter ), or medications ( azathioprine , nonsteroidal anti-inflammatory medications ).
What are the symptoms of febrile neutrophilic dermatosis?
Aug 11, 2021 · INTRODUCTION. The neutrophilic dermatoses are a group of disorders characterized by skin lesions for which histologic examination reveals intense epidermal, dermal, or hypodermal infiltrates composed primarily of neutrophils with no evidence of infection or true vasculitis [ 1 ]. Classification of the neutrophilic dermatoses is based upon the recognition of …
How do you treat neutrophilic dermatosis?
Treatment of acute febrile neutrophilic dermatosis involves systemic corticosteroids, chiefly prednisone 0.5 to 1.5 mg/kg orally once a day tapered over 3 weeks. Colchicine 0.5 mg orally 3 times a day or potassium iodide 300 mg orally 3 times a day are alternative treatments. Antipyretics are also recommended.
What does neutrophilic dermatosis look like?
The most obvious signs of acute febrile neutrophilic dermatosis are distinctive skin lesions that usually develop according to a specific pattern. Typically, a series of small red bumps appear suddenly on the back, neck, arms and face, often after a fever or upper respiratory infection.
How do you treat a sweety infection?
Occasionally, Sweet syndrome resolves on its own without any medical treatment. For most people, treatment involves systemic (whole body) corticosteroid medications, like prednisone. These medications reduce inflammation and curb immune system activity.Feb 27, 2018
Can Sweets syndrome be cured?
Sweet's syndrome might go away without treatment. But medications can speed the process. The most common medications used for this condition are corticosteroids: Pills.Dec 19, 2020
What causes neutrophilic dermatosis?
Sweet's syndrome, also called acute febrile neutrophilic dermatosis, is an uncommon skin condition. It causes fever and a painful skin rash that appears mostly on the arms, face and neck. The cause of Sweet's syndrome isn't known, but it's sometimes triggered by an infection, illness or medication.Dec 19, 2020
Are neutrophilic dermatoses autoinflammatory disorders?
Due to similarities in terms of clinical manifestations, pathogenesis and therapeutic approach, neutrophilic dermatoses have recently been suggested to be part of a spectrum of autoinflammatory disorders.Nov 30, 2016
Can Stomach cause skin problems?
Overview. Ulcerative colitis (UC) is a chronic inflammatory bowel disease (IBD) that affects the large intestine, but it can also cause skin issues. These can include painful rashes. Skin issues affect about 15 percent of all people with different types of IBD.
What is panniculitis and what causes it?
Panniculitis an umbrella term that describes inflammation in the bottom layers of the skin. It can be caused by a variety of infections, diseases, or external stimuli.Apr 13, 2021
What drugs can cause Sweet syndrome?
Which medications cause acute febrile neutrophilic dermatosis (Sweet syndrome)?Lithium.Furosemide.Hydralazine.Carbamazepine.Oral contraceptives.Mirena intrauterine device.COX-2 inhibitors.Azathioprine.More items...
Is Sweet syndrome serious?
These symptoms can point to a number of health conditions, including one you may never have heard of: Sweet syndrome. Usually, this rare skin condition (also known as acute febrile neutrophilic dermatosis) isn't serious and clears up without treatment.Mar 9, 2021
How long does Sweet syndrome last?
Attacks usually last between two and four weeks and may recur during the fall and spring for several years. (For more information on this disorder, choose “erythema multiforme” as your search term in the Rare Disease Database.)
Can Sweet syndrome cause death?
The recurrence of Sweet syndrome may coincide with or precede a hematological relapse. No transformation into acute myeloid leukemia occurred in our cases. However, 7 of the 9 patients died in a follow-up period of 3 to 9 years, confirming the poor prognosis of Sweet syndrome associated with myelodysplasia.
Where are neutrophils located?
There may also be oral ulcers. Acute febrile neutrophilic dermatosis arising on the back of the hands is sometimes called pustular vasculitis.
What is a febrile rash?
Acute febrile neutrophilic dermatosis or Sweet disease presents acutely as a rash accompanied by systemic symptoms. The skin lesions are rapidly evolving juicy often ‘pseudo- vesicular ’ plaques or nodules accompanied by fever, leukocytosis, conjunctivitis and arthralgia. The lesions are most often located asymmetrically on the upper extremities, neck and face and may be painful. There may also be oral ulcers.
What is a pyoderma gangrenosum?
Pyoderma gangrenosum is associated with inflammatory bowel disease, rheumatoid arthritis and haematological malignancies but occasionally arises in otherwise healthy individuals . Pyoderma gangrenosum results in acute and often severe ulceration characterised by an overhanging purple or black necrotic edge and severe pain.
How to tell if you have febrile neutrophilic dermatosis?
The most obvious signs of acute febrile neutrophilic dermatosis are distinctive skin lesions that usually develop according to a specific pattern. Typically, a series of small red bumps appear suddenly on the back, neck, arms and face, often after a fever or upper respiratory infection. The bumps grow quickly in size, spreading into clusters called plaques that may be a centimeter in diameter or larger. The eruptions are tender or painful and may develop blisters, pustules or even ulcers. Lesions may persist for weeks to months and then disappear on their own, without medication. With medical treatment, the skin lesions may resolve in just a few days. [1]
What is febrile dermatosis?
Acute febrile neutrophilic dermatosis is a skin condition characterized by fever, inflammation of the joints ( arthritis ), and painful skin lesions that appear mainly on the face, neck, back and arms. [1] [2] Although middle-aged women are most likely to develop this condition, it may also affect men, older adults and even infants.
What is the HPO database?
People with the same disease may not have all the symptoms listed. This information comes from a database called the Human Phenotype Ontology (HPO) . The HPO collects information on symptoms that have been described in medical resources.
How long do bumps last?
The eruptions are tender or painful and may develop blisters, pustules or even ulcers. Lesions may persist for weeks to months and then disappear on their own, without medication.
Can azathioprine cause cancer?
It is suspected that it can be a reaction of the body to certain exposures (sun), infections ( Streptococcus bacteria, C ampylobacter ), or medications ( azathioprine, nonsteroidal anti-inflammatory medications ). This condition can also occur with some types of cancer and other serious health problems.
How long does it take for a skin lesions to disappear?
Medications, such as corticosteroids ( prednisone or prednisolone), can improve skin lesions and associated symptoms in just two or three days, with the worst of the lesions disappearing within one to four weeks. Doctors usually prescribe systemic corticosteroids (which are taken by mouth) to treat this condition.
Is febrile neutrophilic dermatosis idiopathic?
In many cases, the cause of acute febrile neutrophilic dermatosis is unknown (idiopathic). [1] [2] But sometimes, it can be a sign of an immune system response to one of the following: [1] [3] [4]
What is a neutrophilic dermatosis?
Neutrophilic dermatoses are skin conditions characterised by dense infiltration of inflammatory cells ( neutrophils) in the affected tissue. They arise in reaction to some underlying systemic illness. A neutrophilic dermatosis may be seen in isolation or more than one type may occur in the same individual.
What is the name of the dermatosis of the hands?
Neutrophilic dermatosis of the hands was previously known as ‘ pustular vasculitis ’ of the hands, because inflamed blood vessels are seen on biopsy as well as an infiltration of neutrophil white cells. Neutrophilic dermatosis of the hands. Pustular vasculitis. Pustular vasculitis. Pustular vasculitis.
What does it mean when your hands are red?
Neutrophilic dermatosis of the hands may be the presenting sign of a serious blood condition. A full blood count may reveal raised or reduced numbers of red cells, white cells and/or platelets. Further investigation may require bone marrow examination.
How long does it take for a steroid to clear up?
Within a few days the fever, skin lesions and other symptoms clear up. However, lower doses of steroids are often required for several weeks to months to prevent relapse. Several other medications may be tried when steroids are ineffective or contraindicated. These include: Dapsone.
What are neutrophilic dermatoses?
The neutrophilic dermatoses are a related set of disorders that share common features. These disorders are not directly related to infection and are considered forms of “sterile” neutrophilic inflammation. They can occur with an associated systemic disease or as a primary cutaneous process. Subcorneal pustular dermatosis, Sweet’s syndrome, erythema elevatum diutinum, bowel-associated dermatosis-arthritis syndrome, pyoderma gangrenosum, and neutrophilic eccrine hidradenitis represent the most common of these disorders. This review highlights the salient features of the neutrophilic dermatoses with an emphasis on clinical features, evaluation, and management.
What is a subcorneal pustular dermatosis?
Subcorneal pustular dermatosis (SPD), also eponymously known as Sneddon-Wilkinson disease, is an uncommon, relapsing pustular eruption presenting with erythematous plaques studded with small pustules exhibiting an affinity for the upper trunk, flexures, and intertriginous skin. Annular and serpiginous configurations are commonly observed, and because of the superficial nature of the infiltrate, pustules rupture easily and may be difficult to detect. An almost pathognomonic feature of SPD is the so-called half-half blister in which an undisturbed vesicle contains both purulent and serous fluid that appear distinctly compartmentalized [ 3 ]. Acute flares of disease are often unaccompanied by constitutional signs and symptoms which contrasts with most other pustular eruptions including pustular psoriasis, acute generalized exanthematous pustulosis, and other neutrophilic dermatoses. SPD commonly afflicts middle-aged and elderly women. Microscopically, lesions demonstrate a subcorneal pustule filled with neutrophils which appear to sit atop a relatively undisturbed epidermis [ 3 ]. A superficial perivascular neutrophilic infiltrate may accompany the epidermal changes.
Is IVIG a primary modality?
Its role as a primary modality is uncertain, as it has been exclusively studied as an adjunct. In a retrospective analysis, seven of ten patients with recalcitrant PG treated with 2 g/kg infused over three consecutive days per month demonstrated clearance after one to three cycles [ 99 ]. Nausea, headaches, and, in one case, aseptic meningitis were the reported side effects. The high cost associated with the need for ongoing infusions may preclude its use.
What is Sweet's syndrome?
First described by Robert Sweet in 1964 [ 16 ], Sweet’s syndrome (SS), or acute febrile neutrophilic dermatosis, is prototypic among the neutrophilic dermatoses in terms of clinicopathologic features and disease associations. Sweet’s syndrome classically presents abruptly with painful, red-violet papules, plaques, and nodules favoring the head, neck, upper extremities, and proximal trunk. Lesions can display a pseudovesicular appearance corresponding to the massive dermal edema often noted histopathologically. Frank pustule formation is uncommon [ 17 ]. During the acute phase of disease, pyrexia, constitutional symptoms, and peripheral blood leukocytosis are invariably present. Extracutaneous disease complicates up to half of cases and can involve virtually any organ including the eye, bone, muscle, synovium, central nervous system, kidney, lung, heart, gastrointestinal (GI) tract, and liver [ 2 •, 18 – 20, 21 ••]. Infiltration of visceral organs leads to dysfunction that can be irreversible. Consistent with other neutrophilic dermatoses, young and middle-aged women are most commonly affected with SS, and cutaneous pathergy, the phenomenon whereby lesions occur at sites of traumatic or iatrogenic skin injury, may be a prominent feature [ 20 ]. In most cases, SS remits over several weeks irrespective of treatment although some patients experience a relapsing course. Uncommonly, SS may appear generalized, involve the oral mucosa, and form blisters; these atypical features may herald an occult malignancy [ 17, 22, 23 ]. A variant of SS with strict localization to the dorsal hands has been described and has been also referred to as neutrophilic dermatosis of the hands [ 24, 25 ]. An acute necrotizing form of SS with fascial plane involvement has been described [ 26 ]. Although rare, it remains an important diagnostic consideration, particularly in the hospital setting, as necrotizing SS can be mistaken for necrotizing fasciitis.
Can NSAIDs be used for pyrexia?
Spontaneous resolution of lesions of NEH without scarring is observed in the majority of cases making therapy unnecessary [ 74 ]. NSAIDs can be useful for pyrexia during acute flares. In the instance of recurrence during repeated cycles of chemotherapy for malignancy-associated NEH, prophylactic use of dapsone can prevent relapse.
What is bowel dermatosis?
First described by Jorizzo and others in 1983 [ 57 ], bowel-associated dermatosis-arthritis syndrome (BADAS) is a rare neutrophilic dermatosis characterized by pustular skin lesions and non-deforming polyarthritis occurring in the context of a GI disorder. Bowel-bypass syndrome (BBS) represents a subtype of BADAS uniquely occurring after gastric bypass surgery performed for morbid obesity. Bowel-bypass syndrome shares clinicopathologic features with BADAS and is thought to relate to circulating immune complexes that form as a result of bacterial overgrowth in bypassed and blind loops of bowel [ 58 ]. Skin lesions of both disorders appear as erythematous macules evolving into urticarial plaques and pustules that develop on the trunk and proximal extremities. Erythema nodosum-like lesions have also been described [ 57, 59 ]. During acute flares of disease, patients experience a serum sickness-like illness with fevers, malaise, and arthralgias. Non-erosive arthritis of the small joints commonly accompanies the flare. Skin lesions recede in a few weeks but, without intervention, recur in a predictable fashion that parallels the activity of the GI disease.
Is neutrophilic dermatosis heterogeneous?
Although clinically heterogeneous, the neutrophilic dermatoses are an uncommon, often reactive group of inflammatory skin diseases unified by their similar histopathologic features and underlying disease associations that are best considered various expressions along a disease continuum [ 1, 2 •, 101 ]. Attention to the history and clinical phenotype is helpful to suggest a specific secondary cause, but all newly diagnosed cases require investigation to detect or exclude this possibility. Evaluation should be methodical and comprehensive. Therapeutic management is similar for many of these disorders and can be escalated in a step-wise fashion according to disease response.
How to treat dermatosis?
apply a corticosteroid ointment (hydrocortisone), to the affected areas to reduce dermatosis symptoms. take or apply medications, such as antibiotics or antifungals, as prescribed by a doctor. apply a soothing ointment, such as coconut oil or aloe, to reduce skin dryness. keep the affected area clean and dry.
What is dermatosis skin?
Skin has several layers, including the epidermis, the dermis, and the subcutaneous tissue. A dermatosis may involve changes in any or all of these skin layers. Terms you may hear to describe dermatosis of the skin include: rash: a wide variety of skin conditions that are red and raised. lesion: an area of skin that is abnormal.
What are the most common skin conditions?
Common skin conditions. There are thousands of different skin conditions. Some of the most common forms of dermatosis include: acne: when the oil glands in skin cause pimples and scarring. impetigo: a skin infection caused by bacteria. melanoma: the most serious form of skin cancer.
Is dermatosis the same as acne?
Treatments for dermatosis are often specific to the underlying condition. The treatments for hair loss related to alo pecia areata are understandably not the same as those for acne. However, there are guidelines to keep in mind when you have a dermatosis-related skin condition.
What is the color of ashy dermatosis?
ashy dermatosis: gray- or bluish-brown colored macules that develop on the body. rheumatoid neutrophilic dermatosis: a skin manifestation of rheumatoid arthritis. dermatosis papulosa nigra: many small, benign, dark skin lesions on the face, often in dark-skinned people.
What is the most common form of skin cancer?
melanoma: the most serious form of skin cancer. basal cell carcinoma: the most common form of skin cancer that strikes in the top layer of the epidermis. moles: dark growths on the skin. actinic keratosis: crusty pre-cancerous growths caused by sun damage.
What causes a rash on the face?
lupus erythrematosus: an autoimmune disease that may create a “butterfly” rash on the face. morphea: localized scleroderma, or hardened patches of skin. vitiligo: white of patches of skin. tinea: fungal infection of skin that leaves round marks.
