What are the treatment options for LIS?
Other courses of treatment are often symptomatic. Assistive computer interface technologies such as Dasher, combined with eye tracking, may be used to help people with LIS communicate with their environment. It is extremely rare for any significant motor function to return.
What is lis in nursing?
The American Congress of Rehabilitation Medicine (1995) defines LiS as a syndrome characterized by preserved awareness, relatively intact cognitive functions, and by the ability to communicate while being paralysed and voiceless. Bauer described three categories of LIS (Bauer et al., 1979).
What is the definition of lis syndrome?
The American Congress of Rehabilitation Medicine (1995) defines LiS as a syndrome characterized by preserved awareness, relatively intact cognitive functions, and by the ability to communicate while being paralysed and voiceless. Bauer described three categories of LIS (Bauer et al., 1979). Complete or total LIS: Quadriplegia and anarthria.
What are the different types of lis?
Bauer described three categories of LIS (Bauer et al., 1979). Complete or total LIS: Quadriplegia and anarthria. No eye movement. Classic LIS: Preserved vertical eye movement and blinking.
What is LIS procedure?
Lateral internal sphincterotomy is surgery to help heal an anal fissure that has not improved with medicine or other treatments. An anal fissure is a tear in the lining of the anus. During the surgery, the doctor puts a lighted tube (called an anoscope, or scope) into the anus.
Is LIS surgery painful?
You will likely have some pain with bowel movements at first, but it should be less than what you had before the surgery. You may notice some blood on your toilet paper after you have a bowel movement for the first few weeks after surgery.
How is LIS surgery performed?
In an open sphincterotomy, a 0.5- to 1-cm incision is made in the intersphincteric plane. The internal sphincter is then looped on a right angle and brought up into the incision. The internal sphincter is then cut under direct visualization. The two ends are allowed to fall back after being cut.
Is LIS surgery permanent?
Yes, a sphincterotomy is permanent. It is surgery to permanently release the sphincter muscle of your anus.
What are the side effects of fissure surgery?
Side effects may include: dizziness, lightheadedness, nausea, sedation, vomiting, if these side effects occur, it may help if you lie down after taking the medication. Avoid strenuous activity for 1 week after your procedure.
Is lateral internal sphincterotomy worth it?
Conclusion: Although lateral internal sphincterotomy heals and relieves symptoms of chronic anal fissure in nearly all patients (96 percent), incontinence occurs frequently.
How successful is fissure surgery?
The success rate for fissure healing following surgery was 92 %, being significantly more likely in patients with textbook symptoms (p = 0.016) and those with chronic disease (p = 0.006). The overall complication rate was 13.2 %.
What are the risks of sphincterotomy?
Talk to your doctor if you experience these complications from an anal fissure:Constant bleeding (you'll likely see the blood on toilet paper after you wipe)Pain or discomfort.Trouble passing stool.Clotting.Inability to control gas or bowel movements.Reduced quality of life.
Can fissures come back after surgery?
Approximately 1-6% of patients have a recurrence of their anal fissure after sphincterotomy. The recurrence rate is higher after a sphincter stretch. If a patient develops a recurrence after a sphincterotomy, it could be from recurrent disease or from an improperly or incompletely performed initial sphincterotomy.
Which surgery is best for fissure?
Lateral internal sphincterotomy is currently the procedure of choice for surgical treatment of chronic anal fissures. It is indicated in the presence of persistent pain, bleeding, and lack of response to medical management. More than 90% of fissures heal after lateral internal sphincterotomy.
Is lateral internal sphincterotomy painful?
You will likely have some pain with bowel movements at first, but it should be less than what you had before the surgery. You may notice some blood on your toilet paper after you have a bowel movement for the first few weeks after surgery.
Is laser treatment good for fissure?
Laser treatment for fissure is generally performed under general anesthesia can provide pain relief from the fissure and also reduces strain during the motion. Laser treatment for fissure is highly sought after because of its advantages over traditional open surgery.
What Is Lateral Internal Sphincterotomy?
A lateral internal sphincterotomy is a surgery that repairs an anal fissure. It helps reduce pressure inside the anus that can cause spasms and increases blood flow to the area to help the tissue heal.
Reasons to Consider Surgery
Once you've experienced a tear, it can lead to a repeated injury called a chronic anal fissure. It's the result of muscle spasms in your sphincter. Spasms are not only painful but can pull the unhealed fissure apart, making the wound worse. These spasms can cause even more tearing when you use the bathroom.
What to Expect
A lateral internal sphincterotomy is a short surgery, lasting an average of 30 minutes. Most of the time, you'll return home the same day.
Complications
The most common complication after surgery is anal incontinence. Around half of patients experience this after surgery, but for most, it resolves over time. This can show up as the loss of stool or the inability to control your gas. Other minor complications include:
When should you seek medical advice for LIS?
Locked-In Syndrome (LIS): When should one seek medical advice? Seek medical advice immediately (as soon as possible). It is recommended that whenever the patient has the symptoms, make sure to rush them to a hospital where the facilities are available. In the case of a stroke or a head injury or poisoning, the earlier you present to the hospital, the better the outcome.
What are the symptoms of the locked-in syndrome (LIS)?
A coma-like condition where the subject only can share or respond with others by eye movements. Affected individuals are utterly reliant on caregivers and bedridden. Cognitive function is unaffected despite physical paralysis. Individuals with locked-in syndrome are aware and vigilant of their environment. They can see, hear and have protected sleep-wake cycles.
How to prevent locked in syndrome?
You can prevent it by managing hyper tension, blood pressure, sugar, eating food on time, eating fruits and vegetables, low cholesterol diet, exercising.
Does OnlymyHealth.com take any liability for the same?
All possible measures have been taken to ensure accuracy, reliability, timeliness and authenticity of the information; however Onlymyhealth.com does not take any liability for the same. Using any information provided by the website is solely at the viewers’ discretion. In case of any medical exigencies/ persistent health issues, we advise you to seek a qualified medical practitioner before putting to use any advice/tips given by our team or any third party in form of answers/comments on the above mentioned website.
What is LIS in psychiatry?
Neurology, Psychiatry. Locked-in syndrome ( LIS ), also known as pseudocoma, is a condition in which a patient is aware but cannot move or communicate verbally due to complete paralysis of nearly all voluntary muscles in the body except for vertical eye movements and blinking. The individual is conscious and sufficiently intact cognitively ...
How does Curare poisoning work?
Curare poisoning mimics a total locked-in syndrome by causing paralysis of all voluntarily controlled skeletal muscles. The respiratory muscles are also paralyzed, but the victim can be kept alive by artificial respiration .
What is the name of the condition where a patient cannot move or communicate verbally?
Locked-in syndrome. Locked-in syndrome can be caused by a stroke at the level of the basilar artery denying blood to the pons, among other causes. Locked-in syndrome ( LIS ), also known as pseudocoma, is a condition in which a patient is aware but cannot move or communicate verbally due to complete paralysis of nearly all voluntary muscles in ...
Is there a cure for muscle resuscitation?
Neither a standard treatment nor a cure is available. Stimulation of muscle reflexes with electrodes ( NMES) has been known to help patients regain some muscle function. Other courses of treatment are often symptomatic. Assistive computer interface technologies such as Dasher, combined with eye tracking, may be used to help people with LIS communicate with their environment.
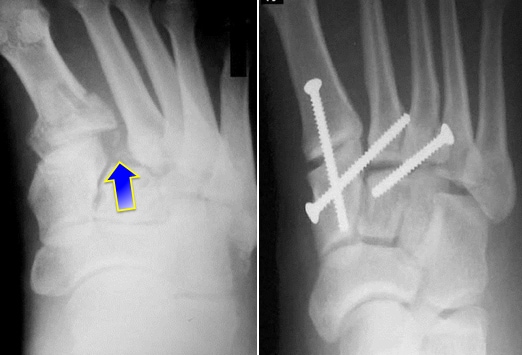
How to heal a Lisfranc foot?
You may undergo a surgical procedure called internal fixation, where the bones of your foot are repositioned and held in place with screws or plates in order to heal. Alternatively, you may undergo a fusion treatment.
What is a Lisfranc fracture?
A Lisfranc fracture occurs when there are either torn ligaments or broken bones in the midfoot area of one or both feet. The midfoot is the area of your foot that makes up the arch, where the forefoot (bones of the toes) and hindfoot (bones including the ankle and heel bone) connect. Your midfoot contains the Lisfranc joint and ...
Why are Lisfranc fractures mistaken for sprains?
Lisfranc fractures are commonly mistaken for simple sprains due to their location and because they typically occur from a twisting fall.
What is a Lisfranc injury?
Lisfranc (midfoot) injuries result if bones in the midfoot are broken or ligaments that support the midfoot are torn. The severity of the injury can vary from simple to complex, involving many joints and bones in the midfoot. A Lisfranc injury is often mistaken for a simple sprain, especially if the injury is a result of a straightforward twist ...
What is a CT scan for Lisfranc?
Computerized tomography scan (CT ) scan. These scans are more detailed than x-rays and can create cross-section images of the foot. This test is not required to diagnose a Lisfranc injury. Because a CT scan will help evaluate the exact extent of the injury and the number of joints that have been injured, a surgeon may order this test to help plan surgery.
Can a Lisfranc sprain be walked off?
However, injury to the Lisfranc joint is not a simple sprain that should be simply "walked off.". It is a severe injury that may take many months to heal and may require surgery to treat.
Can an x-ray show a Lisfranc joint?
An x-ray also can show the alignment of the Lisfranc joint. Any change in the normal joint may suggest injury to the ligaments. If the injury happened after a simple twist and fall (a low-energy injury), the doctor may ask that an x-ray be taken with the patient standing.
Is MRI needed for Lisfranc?
Magnetic resonance imaging (MRI) scan. These studies can create better images of soft tissues like the tendons. This test is not required to diagnose a Lisfranc injury. It may be ordered in cases where the diagnosis may be in doubt.
Can Lisfranc damage the midfoot?
Lisfranc injuries tend to damage the cartilage of the midfoot joints. Cartilage covers the ends of bones in the joints, allowing the joints to move smoothly. If severe midfoot injuries are not treated with surgery, then damage to the cartilage and increased stress at the midfoot joints will result in both collapse of the arch and arthritis, which require complex surgery to correct. Even with successful surgery for the Lisfranc injury, arthritis can still develop in later life.
What is the best treatment for lice and nits?
Spinosad (Natroba). Spinosad is approved for use with people age 6 months or older. It can be applied to dry hair and rinsed with warm water after 10 minutes. It kills lice and nits and usually doesn't need repeated treatment. Malathion. Malathion is approved for use with people age 6 or older.
What is the OTC for lice?
Over-the-counter (OTC) products. OTC medications are based on pyrethrin, a chemical compound extracted from the chrysanthemum flower that is toxic to lice. Wash your child's hair with shampoo with no conditioner before using one of these treatments.
How to find nits in kids hair?
Your doctor will also look for nits in your child's hair. To find nits, he or she may use a specialized light called a Wood's light, which causes nits to appear bluish. But the identification of nits does not necessarily confirm the diagnosis of an active lice infestation.
How to know if your child has lice?
Preparing for your appointment. See your family doctor or pediatrician if you suspect your child has head lice. Your doctor will examine your child's scalp and look for a live nymph or adult louse to determine if he or she has an active head-lice infestation. Your doctor can carefully inspect your child's hair and, if necessary, ...
What is the gold standard for diagnosing head lice?
According to the American Academy of Pediatrics guidelines, the gold standard for diagnosing an active head-lice infestation is the identification of a live nymph or adult louse.
Does OTC kill lice?
Your doctor will likely recommend an over-the-counter (OTC) medication that kills lice and some of the nits. These medications may not kill recently laid eggs. Therefore, an appropriately timed second treatment is usually necessary to kill nymphs after they hatch but before they become adult lice.
Does Permethrin kill nits?
Permethrin is a synthetic version of pyrethrin. Permethrin does not kill nits, and treatment needs to be repeated nine to 10 days after first application. Side effects may include redness and itching of the scalp. Pyrethrin with additives (Rid).
When Is Lisping a Concern?
Many young children have some kind of lisp as they learn to talk. It is one of the most common speech impediments. About 23% of speech-language pathologist clients have lisps.
What are the different types of lisps?
Types of Lisps. There are four types of lisps: Frontal lisp. This lisp occurs when you push your tongue too far forward, making a "th" sound when trying to words with S or Z in them. Lateral lisp. Extra air slides over your tongue when making S and Z sounds, making it sound like there is excess saliva. Palatal lisp.
How do speech pathologists work with lisps?
Speech pathologists work with people who have lisps to help them recognize what their lisp sounds like and how to position their tongue in the correct place to make the sound. They do this by giving them exercises to do, like saying specific words or phrases with the sounds in them.
What is a lisp in speech?
A lisp is a speech impediment that specifically relates to making the sounds associated with the letters S and Z. Lisps usually develop during childhood and often go away on their own. But some persist and require treatment. Another name for lisping is sigmatism.
Why does my child not get a lisp?
Additionally, each child that uses a pacifier doesn't get a lisp. Other possible causes of lisps include: Tongue-tie — a condition where the tongue is tethered to the bottom of the mouth. This restricts its movement. Another name for a tongue-tie is ankyloglossia. Problems with jaw alignment.
What sound does lambdacism use?
Lambdacism. Trouble saying the letter L. People with lambdacism often use the R sound as a substitute.
How long does it take for a child to get rid of a lisp?
They will evaluate what type of lisp your child has and then help them with it over a period of time. It can take anywhere from a few months to a few years to get rid of a lisp. If a child is older when they start working with a speech-language pathologist, it may take a longer time.
Overview
Treatment
Signs and symptoms
Causes
Diagnosis
Prognosis
Neither a standard treatment nor a cure is available. Stimulation of muscle reflexes with electrodes (NMES) has been known to help patients regain some muscle function. Other courses of treatment are often symptomatic. Assistive computer interface technologies such as Dasher, combined with eye tracking, may be used to help people with LIS communicate with their environment.
Research
Locked-in syndrome is usually characterized by quadriplegia (loss of limb function) and the inability to speak in otherwise cognitively intact individuals. Those with locked-in syndrome may be able to communicate with others through coded messages by blinking or moving their eyes, which are often not affected by the paralysis. The symptoms are similar to those of sleep paralysis. Patients who have locked-in syndrome are conscious and aware, with no loss of cognitive functi…
See also
Unlike persistent vegetative state, in which the upper portions of the brain are damaged and the lower portions are spared, locked-in syndrome is essentially the opposite, caused by damage to specific portions of the lower brain and brainstem, with no damage to the upper brain.
Possible causes of locked-in syndrome include: