What are non-pharmacological therapies?
Non-pharmacological therapies are ways to decrease pain in addition to medicine. Your healthcare provider will help you choose therapies that are right for you. Your provider will explain the advantages for each treatment and which may work best for the cause of your pain. Each person may respond to these therapies differently.
Do non-pharmacological treatments prevent adverse events and major health problems?
In this context, according to the studies selected for this review, different forms of non-pharmacological treatment have been used and tested to prevent adverse events and major health problems for patients, namely oxygen therapy, prone position, inhaled nitric oxide, intravenous infusion, passive immunotherapy, and MSC.
What is non-pharmacological pain management?
Non-pharmacological pain management is the management of pain without medications. This method utilizes ways to alter thoughts and focus concentration to better manage and reduce pain.
What is the difference between pharmacological and nonpharmacological interventions in nursing?
As with pharmacological interventions, nonpharmacological interventions have expected outcomes like a reported or observed decrease in the levels of pain and discomfort and increased levels of comfort as reported by the patient or observed by the nurse.
What are examples of non-pharmacological interventions?
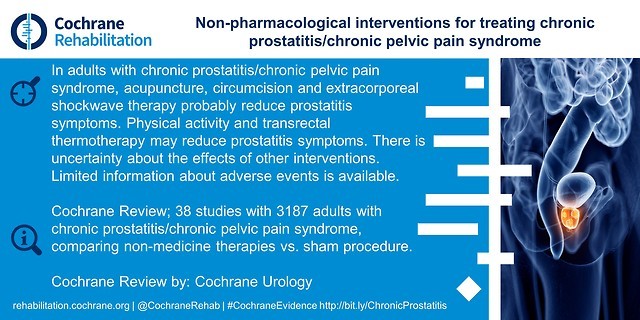
Nonpharmacological approaches to the relief of pain are more commonly associated with nonacute settings and may be classified as follows: (i)psychological interventions (including distraction, stress management, hypnosis, and other cognitive-behavioral interventions), (ii)acupuncture and acupressure, (iii) ...
What is non-pharmacological care?
Non-pharmacological pain management is the management of pain without medications. This method utilizes ways to alter thoughts and focus concentration to better manage and reduce pain.
What is a non-pharmacological therapeutic intervention?
Non-pharmacological intervention: defined as any sort of intervention not directly involving a medication; attempting to optimise a complex patient's healthcare needs21 or to better manage their chronic illness.
What are non-pharmacological forms of pain relief?
What are some common therapies to help control pain?Heat helps decrease pain and muscle spasms. ... Ice helps decrease swelling and pain. ... Massage therapy may help relax tight muscles and decrease pain.Physical therapy teaches you exercises to help improve movement and strength, and to decrease pain.More items...•
What are 4 common non-pharmacological non surgical treatments or therapies that may be considered when managing a client's pain?
physical therapies (such as heat or cold packs, massage, hydrotherapy and exercise) psychological therapies (such as cognitive behavioural therapy, relaxation techniques and meditation) mind and body techniques (such as acupuncture)
Is surgery considered non-pharmacological?
Non-pharmacological treatments can call on various fields of expertise, such as surgery, medical devices, rehabilitation, psychotherapy, and behavioral interventions.
Why should non pharmacologic treatments be considered or used?
Previous research has suggested that using nonpharmacologic therapies to manage chronic pain may be effective not only in decreasing pain and improving function but also in reducing longer-term adverse effects such as substance use disorders and suicide attempts.
What is non-pharmacological treatment of hypertension?
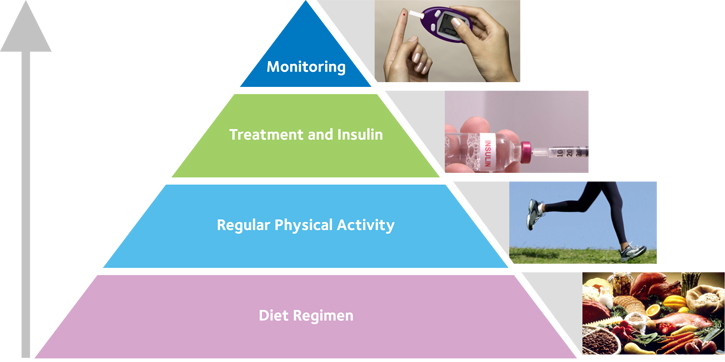
Non-pharmacological interventions help reduce the daily dose of antihypertensive medication and delay the progression from prehypertension to hypertension stage. Non-pharmacological interventions include lifestyle modifications like dietary modifications, exercise, avoiding stress, and minimizing alcohol consumption.
Is oxygen a pharmacological treatment?
Non-pharmacologic treatments include supplemental oxygen, cigarette cessation, nutritional support and others. In addition, several new pharmacologic agents with novel mechanisms of action in early stages of development may be of potential benefit to COPD patients including those in acute exacerbation.
What is the difference between pharmacologic and nonpharmacologic pain relief?
Pharmacological strategies consider the use of drugs to treat and relieve pain. Nonpharmacological strategies favor other modalities of care, especially during the modulation stage of the painful experience.
What are the non-pharmacological management methods for lower back pain?
Several nonpharmacologic, noninvasive therapies are available for low back pain, including exercise, complementary and alternative therapies (such as spinal manipulation, acupuncture, massage, and mind–body interventions), psychological therapies (such as cognitive behavioral and operant therapy), physical techniques ( ...
What is non-pharmacological treatment for depression?
Non-pharmacological interventions include formal psychological therapies such as cognitive behaviour therapy (CBT) and interpersonal psychotherapy (IPT), as well as less formal supportive therapies such as counselling within primary care, mindfulness-based therapy, behavioural activation and self-help strategies.
What Are Non-Pharmacological Therapies For Pain?
Non-pharmacological therapies are ways to decrease pain in addition to medicine. Your healthcare provider will help you choose therapies that are r...
Why Is Pain Control Important?
If pain is not treated, it can decrease your appetite and make it difficult for you to sleep. You may feel that you lack energy or the ability to d...
What Therapies Are Used With Medicine to Help Control Pain?
1. Heat helps decrease pain and muscle spasms. Apply heat to the area for 20 to 30 minutes every 2 hours for as many days as directed. 2. Ice helps...
What Other Therapies May Help Control Or Reduce Pain?
1. Relaxation techniques can help you relax, relieve stress, and decrease pain. Common relaxation techniques include any of the following: 1. Aroma...
Where Can I Find More Information?
1. National Center for Complementary and Alternative Medicine, NIHInformation ClearinghousePO Box 7923Gaithersburg , MD 20898Phone: 1- 888 - 644622...
When Should I Contact My Healthcare Provider?
1. Your pain does not get better, or you have new pain. 2. You have questions or concerns about your condition or care.
What is the best treatment for nonsmall cell bronchial carcinoma?
Surgical treatment is used for both malignant and nonmalignant respiratory disease. It is the treatment of choice for primary nonsmall cell bronchial carcinoma, and gives the best prospect of cure when the tumour appears technically resectable, there is no evidence of metastasis and the patient is fit for the procedure. Depending on the extent and position of the cancer, resection may involve removal of a whole lung (pneumonectomy), one or more lobes (lobectomy) or, less commonly, a lung segment (segmentectomy).
What is NIV in respiratory care?
Ventilation is achieved by delivering air (with or without supplementary oxygen) via a tight-fitting face mask applied to the nose, or nose and mouth (the range of patient ‘interfaces’ is the same as is used for delivering continuous positive airway pressure (CPAP) for treating obstructive sleep apnoea syndrome (OSAS) – see below). In most respiratory departments, NIV is now first-line management for patients requiring ventilatory assistance for acute exacerbations of COPD. It is also increasingly used for long-term nocturnal domiciliary ventilation in certain groups of patients with chronic hypercapnia. It is particularly suitable and effective for chronic respiratory failure due to severe respiratory muscle weakness (e.g. various muscular dystrophies or motor neurone disease/amyotrophic lateral sclerosis) or severe deformity of the chest wall (e.g. scoliosis). Long-term domiciliary NIV is also used in some patients with severe COPD, but its indications in this condition require further investigation.
Is physiotherapy good for bronchial secretions?
Physiotherapy is particularly helpful as an aid to clearing bronchial secretions, for example in acute exacerbations of COPD and in patients with chronic production of infected sputum, as in CF and bronchiectasis. Various techniques are used, including postural drainage and forced expiration; often, these are taught to patients who continue to use them regularly at home. Other important aspects of physiotherapy, including exercise and muscle training, are employed as part of pulmonary rehabilitation (see chapter 29 ).
What are the techniques used in pulmonary rehabilitation?
Various techniques are used, including postural drainage and forced expiration ; often, these are taught to patients who continue to use them regularly at home. Other important aspects of physiotherapy, including exercise and muscle training, are employed as part of pulmonary rehabilitation (see chapter 29 ).
Is radiotherapy used for bronchial carcinoma?
More commonly, radiotherapy is used, sometimes in combination with chemotherapy, in both small and nonsmall cell bronchial carcinoma, with the aim of achieving a partial or, occasionally, complete response, and also as palliative treatment to improve symptoms, particularly haemoptysis or pain due to bone invasion or metastasis.
Can radical radiotherapy be used for nonsmall cell bronchial carcinoma?
In a minority of patients with nonsmall cell bronchial carcinoma, radical radiotherapy is used with the aim of achieving a cure. This approach is only appropriate for patients with small peripheral tumours, with no evidence of spread, and in whom surgical resection is not an option.
What is cognitive behavioural therapy?
Cognitive behavioural therapy (CBT) CBT is based on the propositions that cognitive functioning affects behaviour, can be monitored and changed and that desired behaviour change can be achieved through cognitive change. 3 CBT has demonstrated limited efficacy in reducing depressive symptoms. 4.
What is mindfulness based cognitive therapy?
Mindfulness-based cognitive therapy (MBCT) MBCT is a psychotherapy that has been shown to successfully reduce relapse in depression by up to 34%. 7 It combines psychological and educational aspects of CBT with meditation components of mindfulness-based stress reduction. 8.
Is psychotherapy a treatment for depression?
For patients presenting with mild to moderate depression, psychotherapy is one of the treatment options recommended by NICE. For more severe cases, psychotherapy remains an important aspect of treatment, administered alongside pharmacotherapy. 3.
What is the best treatment for neuropathic pain?
Antiepileptic drugs . Gabapentin and pregabalin are used as first- line therapy in the treatment of neuropathic pain, and are frequently prescribed in daily practice, as neuropathic mechanisms play a critical role in the emergence of lumbosacral radicular pain and neurogenic claudication.[11] .
What are the treatments for CLBP?
Antibiotic therapy, cannabinoids, novel opioids, calcitonin, melatonin, nerve growth factor inhibitors, ketamine and botulinum toxin have been evaluated in several clinical trials for CLBP. Evidence on the effectiveness of some of these treatments is conflicting and some are still limited.
Is it safe to take opioids for long term?
It is shown to be effective in terms of pain relief and improving functionality in short-term use, but long-term effectiveness and safety of use are uncertain. Routine use of opioids is not recommended, as their advantages are small and there are significant risks such as overdose and addictive potential.
Assessing the Client's Need for Palliative Care
As previously stated, according to the National Board for Certification of Hospice and Palliative Nurses, "Hospice and palliative care is the provision of care for the patient with life-limiting illness and their family with the emphasis on their physical, psychosocial, emotional and spiritual needs.
Assessing the Client's Need for Pain Management
Pain is a highly complex phenomenon. Plato described pain as an emotion and not a sensation; Hippocrates believed that pain was the result of a lack of balance in terms of the body's fluids. Neither Hippocrates nor Plato believes that the brain played any role in terms of pain.
Recognizing Differences in the Clients' Perceptions and Responses to Pain
Like all other things, clients vary in terms of their perceptions of pain and their responses to pain. Some of the factors that impact on the clients' perceptions of and responses to pain include:
Incorporating Alternative and Complementary Therapies Into the Client's Plan of Care
As fully described above in the section entitled " Evaluating the Client on Alternative or Homeopathic Health Care Practices ", nurses assess the clients' needs for alternative and complementary therapies such as progressive relaxation and music therapy and then incorporate these therapies into the client's plan of care.
Counseling the Client Regarding Palliative Care
Clients have the innate right to self-determination and to make their own decisions about care without any coercion from members of the health care team. Many clients at the end of life may not be knowledgeable about palliative care and hospice care.
Respecting the Client's Palliative Care Choices
Clients should be provided with complete information about palliative care and they should also have the opportunity to discuss all of their alternatives and options. This education should also include the benefits and risks associated with alternative choices and their choices in the same manner that is done with all informed consents.
Assisting the Client in Receiving Appropriate End of Life Physical Symptom Management
Some of the intervention for hypovolemic shock, in addition to correcting an underlying cause such as bleeding and dehydration, are intravenous fluid replacements with fluids like lactated Ringers, the administration of blood, blood components and plasma expanders, and placing the client in the Trendelenburg position.
What is the goal of chronic pain management?
The overarching goal of chronic pain management is to relieve pain and improve function. The National Pain Strategy (NPS) report recommends that management be integrated, multimodal, interdisciplinary, evidence-based, and tailored to individual patient needs. 5 In addition to addressing biological factors when known, it is thought that optimal management of chronic pain also addresses psychosocial contributors to pain, while taking into account individual susceptibility and treatment responses. Self-care is an important part of chronic pain management. At the same time, the NPS points to the "dual crises" of chronic pain and opioid dependence, overdose, and death as providing important context for consideration and implementation of chronic pain management strategies. A vast array of pharmacologic and nonpharmacological treatments is available for management of chronic pain. An overview of these interventions is briefly presented below.
How long does a systematic review last?
Duration of followup: short term (up to 6 months), intermediate term (6-12 months) and long term (at least 1 year); focus on longer term (>1 year) effects.
