What are the recommendations for the treatment of hypertension in pregnancy?
Recommendations for the treatment of chronic hypertension in pregnancy support the use of anti-hypertensive therapy for BP levels of ≥ 160/110 mm Hg or in the presence of target organ damage, such as left ventricular hypertrophy and renal insufficiency [ 1 ].
What is the best blood pressure medicine for pregnancy?
For the initial treatment of high blood pressure in pregnancy, the three most commonly used medications are labetalol (Normodyne, Trandate), nifedipine (Procardia, Adalat) and methyldopa (Aldomet) and these are recommended above all other medications.
What should my blood pressure be if I am pregnant?
Some women may be on blood pressure lowering medications before they become pregnant. Usually these are started to keep your systolic blood pressure less than 140 (top number) and to keep the diastolic blood pressure less than 90 (bottom number).
Is tight blood pressure control during pregnancy beneficial?
Hypertension is a key risk factor for CVD and its treatment reduces complications over time. 12 However, the benefits of tight blood pressure control during pregnancy are controversial. During pregnancy, the goal of pharmacologic management of hypertension is to prevent acute complications while minimizing risk to the fetus.
When do you start antihypertensive in gestational hypertension?
Acknowledging limitations in evidenced-based data and other concerns discussed above regarding gestational age, we recommend a threshold for treatment of most pregnant hypertensive women of 140 to 150 mm Hg systolic, and/or 95 to 100 mm Hg diastolic to prevent worsening hypertension in the mother.
What blood pressure should be treated in pregnancy?
Several health advocacy groups recommend beginning treatment when blood pressure measures during pregnancy are from 140/90 mm Hg (Canadian guidelines) to 160/110 mm Hg (U.S. guidelines).
What is the first drug of choice for hypertension in pregnancy?
Methyldopa is a drug of first choice for control of mild to moderate hypertension in pregnancy and is the most widely prescribed antihypertensive for this indication in several countries, including the US and the UK.
Is 150 90 blood pressure high during pregnancy?
During pregnancy: Mildly high blood pressure is blood pressure between 140/90 and 149/99 mm Hg (ie the systolic or upper number is between 140 and 149, and/or the lower or diastolic number is between 90 and 99). Moderately high blood pressure is blood pressure between 150/100 and 159/109 mm Hg.
What BP is considered preeclampsia?
Symptoms. Signs of preeclampsia in a pregnant woman include: Blood pressure of 140/90. Systolic blood pressure that rises by 30 mm Hg or more even it if is less than 140.
What is considered high BP in pregnancy?
You have gestational hypertension when: You have a systolic blood pressure of 140 mm Hg or higher and/or a diastolic blood pressure of 90 mm Hg or higher. The high blood pressure first happens after 20 weeks of pregnancy. You had normal blood pressure before pregnancy.
What is normal blood pressure 39 weeks pregnant?
The American College of Obstetricians and Gynecologists (ACOG) state that a pregnant woman's blood pressure should also be within the healthy range of less than 120/80 mm Hg. If blood pressure readings are higher, a pregnant woman may have elevated or high blood pressure.
When should I worry about my blood pressure during pregnancy?
After 20 weeks of pregnancy, blood pressure that exceeds 140/90 mm Hg — documented on two or more occasions, at least four hours apart, without any other organ damage — is considered to be gestational hypertension.
What is considered mild preeclampsia?
Preeclampsia can be categorized as mild or severe. You may be diagnosed with mild preeclampsia if you have high blood pressure plus high levels of protein in your urine. You are diagnosed with severe preeclampsia if you have symptoms of mild preeclampsia plus: Signs of kidney or liver damage (seen in blood work).
What Are The Types of High Blood Pressure During pregnancy?
Sometimes high blood pressure is present before pregnancy. In other cases, high blood pressure develops during pregnancy. 1. Gestational hypertensi...
Why Is High Blood Pressure A Problem During pregnancy?
High blood pressure during pregnancy poses various risks, including: 1. Decreased blood flow to the placenta. If the placenta doesn't get enough bl...
How Will I Know If I Develop Hypertension During pregnancy?
Monitoring your blood pressure is an important part of prenatal care. If you have chronic hypertension, your health care provider will consider the...
How Will I Know If I Develop Preeclampsia?
Besides high blood pressure, other signs and symptoms of preeclampsia include: 1. Excess protein in your urine (proteinuria) or additional signs of...
Is It Safe to Take Blood Pressure Medication During pregnancy?
Some blood pressure medications are considered safe to use during pregnancy, but angiotensin-converting enzyme (ACE) inhibitors, angiotensin II rec...
What Should I Do to Prepare For pregnancy?
If you have high blood pressure, schedule a preconception appointment with the health care provider who'll handle your pregnancy. Also meet with ot...
What Can I Expect During Prenatal Visits?
During pregnancy, you'll see your health care provider often. Your weight and blood pressure will be checked at every visit, and you might need fre...
What Can I Do to Reduce The Risk of Complications?
Taking good care of yourself is the best way to take care of your baby. For example: 1. Keep your prenatal appointments. Visit your health care pro...
What About Labor and Delivery?
Your health care provider might suggest inducing labor before your due date to avoid complications. The timing of your induction is based both on h...
Will I Be Able to Breast-Feed My Baby?
Breast-feeding is encouraged for most women who have high blood pressure, even those who take medication. Discuss medication adjustments you'll nee...
What is the best medication for hypertension during pregnancy?
Drug treatment of hypertension in pregnancy. According to NHBPEP methyldopa, labetalol, beta blockers (other than atenolol), slow release nifedipine, and a diuretic in pre-existing hypertension are considered as appropriate treatment [1].
What is DBP in gestational hypertension?
In gestational hypertension DBP is determined as the disappearance of sound (Korotkoff 5).
What phase is DBP measured in?
Measure DBP as disappearance of sounds (phase V)
When is 24 hour ABPM used?
24 hour ABPM- Useful for the evaluation of early hypertension (<20 weeks gestation) where 1/3 of women will have “white coat” hypertension and half of these women will go on to have ABPM confirm ed hypertension later in pregnancy
What is the most common medical condition during pregnancy?
Similar to the non-pregnant population, hypertension is the most common medical disorder encountered during pregnancy and is estimated to occur in about 6–8% of pregnancies [1]. A recent report highlighted hypertensive disorders as one of the major causes of pregnancy-related maternal deaths in the United States, ...
Which is more favorable, white coat or sustained hypertension?
White-coat hypertension has a more favorable outcome than sustained hypertension diagnosed by ABPM
Is methyldopa safe for pregnancy?
Methyldopa has a long history of use in pregnancy and does not appear teratogenic [27]. Methyldopa has a record of safety in pregnancy, as established by follow-up studies in the 1980’s of children exposed to the drug in utero [31].
What changes blood pressure during pregnancy?
Changes in blood pressure (BP) during normal pregnancy are related to alterations in cardiac output and systemic vascular resistance (SVR). Systemic vasodilation is induced by pregnancy hormones such as estrogen, progesterone, prolactin and relaxin [7], along with a decreased responsiveness to pressor hormones, such as angiotensin II and vasopressin [8]. This systemic vasodilation, combined with the low resistance system of the uteroplacental circuit, results in a marked reduction in SVR. In response to this, there is a gradual increase in plasma volume, accomplished through an increase in plasma renin, accompanied by reduced atrial natriuretic peptide levels [9]. Heart rate increases, mainly due to systemic vasodilation. The overall effect is of increased cardiac output [10]. The sum effect of these hemodynamic changes is an initial decrease in systemic arterial BP by 10 – 15 mmHg in early pregnancy. A nadir in BP usually occurs towards the end of the second trimester. Beginning in the third trimester, BP rises by about 10 mmHg, and returns to the individual’s baseline value by the end of pregnancy [11].
What is the recommended BP for preeclampsia?
With respect to preeclampsia, the current guidelines recommend treatment of diastolic BP levels >105 mmHg or lower in high risk circumstances, such as teenagers with recent diastolic pressures <70 mm Hg, or evidence of cardiac or cerebral decompensation; the level of systolic BP at which anti-hypertensive therapy is indicated was not defined [1]. A study of 29 women who developed a stroke in the setting of severe preeclampsia and eclampsia showed that the diastolic BP was ≥ 105 mm Hg in only 20% of patients, while all patients had a systolic BP >155 mm Hg [41]. The report called for a paradigm shift towards considering anti-hypertensive therapy for these patients when the systolic BP reaches or exceeds 155–160 mm Hg. In addition, PRES seems to occur at lower peak systolic BP values in pregnant compared to non-pregnant patients [42, 18]. In summary, the findings of these studies support medical treatment for a systolic BP ≥ 150 mm Hg in women who develop hypertension during pregnancy, and continuation of therapy in women with chronic hypertension on adequate therapy prior to becoming pregnant. Current clinical practice, for the most part, does not reflect published guidelines. Most investigators agree that anti-hypertensive therapy in a preeclamptic patient should be initiated for a diastolic BP approaching 100 mm Hg, and for BP ≥ 150–160/100 mm Hg [35]. But should this still be the recommended level for initiation of antihypertensive medications?
What is the most common medical condition during pregnancy?
Hypertension is the most common medical condition encountered during pregnancy, occurring in approximately 6–8% of pregnancies [1]. The hypertensive disorders of pregnancy cover a spectrum of conditions, including preeclampsia-eclampsia, gestational hypertension and chronic hypertension . The pooled incidence of preeclampsia in developing countries is reported to be around 3.4% and, in developed countries, ranges from 0.4–2.8% [2]. In the US, the rates of hypertensive pregnancy disorders (HPD) have risen steadily over the last 3 decades, with the most recently reported rates of preeclampsia and gestational hypertension of 29.7 and 32.1 per 1000 deliveries, respectively [3]. As a group, HPD represent the most common direct cause of maternal mortality in both developed countries (16% of all maternal deaths) and developing countries (9–25% of all maternal deaths) [4]. Hypertension in pregnancy is one of the major causes of maternal mortality in the United States (similar to other industrialized countries), accounting for 12.3% of the maternal deaths between 1998 and 2005 [5]. Even in the modern era, hypertension in pregnancy imparts a significant increase in maternal morbidity. In 36,537,061 delivery discharges between 1998 and 2006, as identified by the Nationwide Inpatient Sample of the Healthcare Cost and Utilization Project, there was an increased risk for obstetric complications, such as acute renal failure, pulmonary edema, need for ventilator support, and cerebrovascular complications, for every category of hypertensive pregnancy including mild preeclampsia [6].
What causes a decrease in placental perfusion?
In preeclampsia, the placental spiral arteries fail to lose their musculoelastic layers ultimately leading to decreased placental perfusion [12, 13]. Placental hypoxia is frequently viewed as an early trigger of placental production of soluble factors resulting endothelial dysfunction [14], which may play a central role in the pathogenesis of the maternal syndrome of preeclampsia. Recent studies of vascular endothelial growth factor (VEGF) and its receptors have suggested that down-regulation of VEGF may be the missing link between the ischemic placenta and maternal endothelial dysfunction [15]. Other mechanisms implicated in the pathophysiology of preeclampsia include, oxidative stress, placental steroidogenesis, formation of agonist auto-antibodies against the angiotensin II receptor, exaggeration of the hypercoagulability of pregnancy, and insulin resistance [16, 17]. The end result of this complex interplay between maternal and placental mechanisms is a maternal multi-system disorder, characterized by hypertension, proteinuria, and, in severe cases, multi-organ dysfunction.
Is hypertension a maternal disease?
Hypertensive pregnancy disorders (HPD) are important causes of maternal and fetal morbidity and mortality worldwide. In addition, a history of HPD has been associated with an increased risk for maternal cardiovascular disease later in life, possibly due to irreversible vascular and metabolic changes that persist beyond the affected pregnancies. Therefore, treatment of HPD may not only improve immediate pregnancy outcomes, but also the maternal long-term cardiovascular health. Unlike the recommendations for hypertension treatment in the general population, treatment recommendations of HPD have not changed substantially for more than two decades. This is particularly true for mild to moderate hypertension in pregnancy, defined as a blood pressure of 140–159/90–109 mm Hg.
Is hypertension in the second trimester?
Hypertension occurring in the second trimester in the absence of proteinuria
Does decreased maternal BP affect uteroplacental circulation?
concern that decreased maternal BP may compromise uteroplacental and fetal circulation, thus resulting in small-for-gestational–age (SGA) infants
What is the best medication for high blood pressure during pregnancy?
For the initial treatment of high blood pressure in pregnancy, the three most commonly used medications are labetalol (Normodyne, Trandate), nifedipine (Procardia, Adalat) and methyldopa (Aldomet) and these are recommended above all other medications.
How low should blood pressure be before pregnancy?
Some women may be on blood pressure lowing medications before they become pregnant. Usually these are started to keep your systolic blood pressure less than 140 (top number) and to keep the diastolic blood pressure less than 90 (bottom number).
Why is it important to have a prenatal visit?
For this reason, it is important to attend your prenatal visits. Your doctor may order additional blood and urine tests to help you have a successful pregnancy. The treatment for preeclampsia at full term is to deliver your baby, which will improve your health .
What are the medical problems that women have before they get pregnant?
One of the most common medical problems that women have before they become pregnant is chronic hypertension, also known as chronic high blood pressure.
How to control blood pressure in women?
Some women are able to control their blood pressure with exercise, weight loss, limiting alcohol use, reducing sodium intake and following specific diets that are abundant with fruits and vegetables, low in fat dairy products and high in fiber.
Can you take blood pressure medication while pregnant?
Certain blood pressure medications cannot be used in pregnancy. The use of angiotensin-converting enzyme inhibitors (ACE inhibitors), angiotensin receptor blockers (ARBs), renin inhibitors and mineralocorticoid receptor antagonists are not recommended while you are pregnant.
Can you take antihypertensive while pregnant?
Medications from almost every antihypertensive drug class have been prescribed during pregnancy but the data on safety are incomplete and limited to a few medications. Hypertension that occurs during pregnancy complicates up to 10 percent of all pregnancies. There can be very serious complications to you or your baby when you have high blood ...
What is the term for hypertension before pregnancy?
Chronic hypertension with superimposed preeclampsia. This condition occurs in women with chronic hypertension before pregnancy who develop worsening high blood pressure and protein in the urine or other blood pressure related complications during pregnancy. Preeclampsia. Preeclampsia occurs when hypertension develops after 20 weeks of pregnancy, ...
What are the types of high blood pressure during pregnancy?
Sometimes high blood pressure is present before pregnancy. In other cases, high blood pressure develops during pregnancy.
How will I know if I develop hypertension during pregnancy?
Monitoring your blood pressure is an important part of prenatal care. If you have chronic hypertension, your health care provider will consider these categories for blood pressure measurements:
How will I know if I develop preeclampsia?
Besides high blood pressure, other signs and symptoms of preeclampsia include:
What happens if you have preeclampsia?
Preeclampsia occurs when hypertension develops after 20 weeks of pregnancy, and is associated with signs of damage to other organ systems, including the kidneys, liver, blood or brain. Untreated preeclampsia can lead to serious — even fatal — complications for mother and baby, including development of seizures (eclampsia).
What is considered gestational hypertension?
After 20 weeks of pregnancy, blood pressure that exceeds 140/90 mm Hg — documented on two or more occasions, at least four hours apart, without any other organ damage — is considered to be gestational hypertension .
How long does it take for a woman to develop high blood pressure?
Women with gestational hypertension have high blood pressure that develops after 20 weeks of pregnancy. There is no excess protein in the urine or other signs of organ damage. Some women with gestational hypertension eventually develop preeclampsia. Chronic hypertension.
What to do if you have high blood pressure while pregnant?
If you have high-blood pressure during pregnancy, ACOG recommends regular prenatal check-ups for both you and your baby. Doctors are likely to perform the following tests to monitor your gestational hypertension:
What is the goal of gestational hypertension?
The main goal of treatment is to prevent the development of more serious conditions.
Why is it important to treat pregnancy?
The main goal of treatment is to prevent the development of more serious conditions. Pregnant parents can develop seizures or placental abruption, while their babies can be harmed by fetal growth restriction, pre-term delivery, or stillbirth. 1.
Can gestational hypertension cause preeclampsia?
Up to half of people with gestational hypertension go on to develop preeclampsia or symptoms consistent with it. 1. In choosing a specific treatment plan, details such as blood pressure levels, how far along the pregnancy is, and how well the baby is doing will all be considered. It used to be common for doctors to prescribe bed rest ...
Can hypertension cause hospitalization?
If your hypertension has become severe enough to put you or your baby's health at immediate risk, or getting to regular check-ups is hard, your doctor might recommend hospitalization during certain phases of pregnancy to ensure that you and your child are well cared for. 1.
Can pregnancy cause hypertension?
There are several strategies to treat hypertension that develops during pregnancy. These strategies are similar to those used to treat preeclampia, which is when a pregnant person has gestational hypertension as well as increased levels of protein in their urine. Up to half of people with gestational hypertension go on to develop preeclampsia or symptoms consistent with it. 1
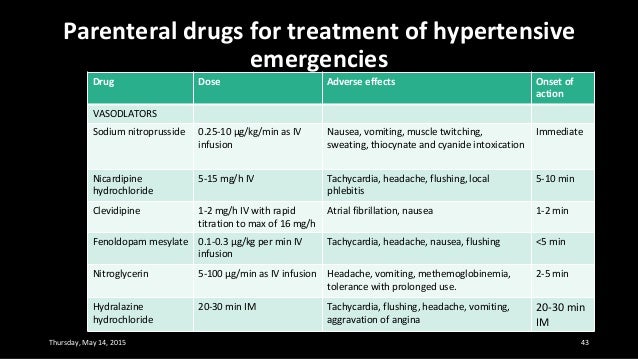
Which blood pressure medication slows down heart rate?
Labetalol: a beta-blocker, which helps to slow your heart rate. Hydralazine: a vasodilator, which relaxes blood vessels to promote blood flow. Nifedipine: a calcium-channel blocker, which also eases the blood vessels to prevent the heart from needing to pump so hard 1.
What is the diagnosis of hypertension during pregnancy?
Disease Spectrum. Hypertension during pregnancy can occur in one of three forms: chronic hypertension, gesta tional hypertension (GH) and preeclampsia (PE). Chronic hypertension is defined as elevated blood pressure known before conception or diagnosed before 20 weeks of gestation. GH is hypertension that develops any time after 20 weeks ...
How can a pregnant woman improve her health?
Pregnancy provides a unique opportunity for both patients and providers to engage in improving overall health. Many studies have shown that women are motivated to change their lifestyle habits during pregnancy and the postpartum period. Obstetricians and cardiologists can improve the cardiovascular health of women through enhanced collaboration. A recent joint presidential advisory from ACOG and the American Heart Association called for a multidisciplinary approach in management incorporating lifestyle and behavioral modifications including diet, exercise and smoking cessation as well as electronic medical record based standardized algorithms targeting cardiovascular risk factors. Shared information between the two disciplines can be used to assess risk, initiate interventions and facilitate significant and lasting lifestyle changes. 22
What medications are used during postpartum period?
Since breastfeeding is strongly encouraged by the American College of Obstetrics and Gynecologists (ACOG), medications that are not excreted into breast milk are preferred. Methyldopa, labetalol and propranolol are considered safe. Beta blockers such as metoprolol and atenolol can achieve high levels in breast milk and should be avoided for this reason. The angiotensin converting enzyme inhibitors captopril and enalapril are considered safe given their low concentrations in breast milk. 2 There are limited data for calcium channel blockers, but nifedipine is commonly used during breastfeeding. Diuretics are discouraged because of the risk of reducing breast milk production. 2,16 Nonsteroidal anti-inflammatories should also be avoided to prevent sodium retention and hypertension.
Does GH affect pregnancy?
Chronic hypertension, GH and PE have been shown to have adverse effects on pregnancy and associations with a higher risk for cardiovascular disease (CVD) outcomes. Many studies have shown an association between PE and CV disease in later life. 3-5 A large meta-analysis from Wu et al. showed that women with a history of PE have a 71% increased risk of CV mortality, a 2.5-fold increase in risk of coronary artery disease (CAD), and a 4-fold increase in the development of heart failure when compared to normal cohorts. 3 The Nurses' Health Study II reported that women with GH and PE had almost a 3-fold and 6-fold increased rate of chronic hypertension, respectively. It also showed that women who were hypertensive during their first pregnancy had a 70% increased risk of type 2 diabetes and 30% increased prevalence of hypercholesterolemia later in life. 6 Recurrent PE is associated with a higher risk of future CVD events including hospitalization from heart failure or cardiac procedures compared with no PE, and significantly shorter time to a first cardiovascular event. 7
Is hypertension a risk factor for CVD?
During pregnancy, the goal of pharmacologic management of hypertension is to prevent acute complications while minimizing risk to the fetus. There is no evidence that treatment of mild to moderate hypertension during pregnancy improves maternal or perinatal outcomes (including preeclampsia, preterm birth and small for gestational age or infant mortality). 13 In fact, most women with mild hypertension can stop their antihypertensive medications during the first and second trimesters due to the physiological drop in blood pressure that occurs during this time. Those who require treatment can continue their medical regimen except for renin angiotensin aldosterone system inhibitors including angiotensin converting enzyme (ACE) inhibitors, angiotensin receptor blockers and direct renin inhibitors. This class of pharmacotherapy is contraindicated during pregnancy due to the increased risk of fetal renal malformations.14 Severe hypertension should be aggressively treated to reduce the risk of progression to preeclampsia and hemorrhagic stroke.