
...
Options for certain conditions caused by cystic fibrosis include:
- Nasal and sinus surgery. ...
- Oxygen therapy. ...
- Noninvasive ventilation. ...
- Feeding tube. ...
- Bowel surgery. ...
- Lung transplant.
Medication
Nov 17, 2021 · One of the primary goals of cystic fibrosis treatment is to clear mucus from the lungs using physical therapy combined with mucus thinners taken through an inhaler or nebulizer. Mucolytics, such as dornase alfa, break up substances in the mucus, making it less sticky and easier to expel.
Procedures
22 rows · May 01, 2016 · Treatment for cystic fibrosis (CF) has conventionally targeted downstream consequences of the ...
Therapy
Medication. Digestive Treatments. Chest Physical Therapy (CPT) Exercise. Gene Therapy. Clinical Trials. Surgery. There’s no cure for cystic fibrosis …
Nutrition
Jul 15, 2019 · Yoga, meditation, exercise, hanging out with friends, and hobbies are all popular and effective ways to manage stress, anxiety, and depression. Lung transplant When the lungs are beginning to fail, a person with CF may qualify for a lung transplant. Complementary and alternative medicine
See more
Nov 26, 2019 · Recently developed treatments, called modulators as a class, restore the ability of cells to make the cystic fibrosis protein work to maintain …
Who is the longest living person with cystic fibrosis?
Physiotherapy is vital to people with CF, principally in developing and maintaining optimal airway clearance but also across a range of other vital functions including sinus management, exercise and even help with ingesting medicines. Because your condition is unique to you, your physiotherapist will help you develop a bespoke treatment regimen.
What is routine care of patients with cystic fibrosis include?
Nov 21, 2017 · The antibiotics chlortetracycline and oxytetracycline are the first-choices for treating infections. Stronger doses in combination with antibiotics chloramphenicol and erythromycin are used for more dangerous infections. 1980s IV antibiotics gentamicin and tobramycin are used widely for CF patients. 1990s
What is the prognosis for cystic fibrosis?
Trikafta is the first approved treatment that is effective for cystic fibrosis patients 12 years and older with at least one F508del mutation, which affects 90% of the population with cystic...
How to prevent cystic fibrosis?
Cystic fibrosis is a progressive, genetic disease that causes long-lasting lung infections and limits the ability to breathe over time. More than 30,000 children and adults in the United States have CF (70,000 worldwide) and CF affects people of every racial and ethnic group.
Who treats cystic fibrosis?
This team will include pulmonologists, gastroenterologists, endocrinologists, nutritionists, nurses, and physical therapists.
What are the treatments for fibrosis?
Cystic fibrosis affects systems and organs throughout the body, so many other types of drugs will be relied on to treat symptoms, such as anti-inflammatory medications, prokinetics to treat gastroesophageal reflux, laxatives for intestinal obstruction, bile acids for liver blockage, and insulin for diabetes.
Why is mucus sticky in the lungs?
This is the basic mechanism responsible for cystic-fibrosis-related diseases throughout the body: Mucus in the lungs is too sticky to clear out and provides a rich environment for bacteria growth , resulting in chronic lung infections, bronchial damage (bronchiectasis), and scarring (fibrosis).
What causes mucus to be sticky?
Cystic fibrosis (or mu coviscidosis) is an inherited condition that reduces the water content of secretions within the body, causing thick and sticky mucus which fills up and blocks the lungs and other organs. It is one of the most common heritable genetic disorder in Caucasians in the US.
How many mutations are there in cystic fibrosis?
There are over 2000 genetic mutations that are responsible for cystic fibrosis. All are related to the CFTR protein. Based on the type of mutation, cystic fibrosis is divided into five classes of decreasing severity. Class 1 CF means cells are unable to produce working copies of CFTR proteins.
How to clear mucus from lungs?
One of the primary goals of cystic fibrosis treatment is to clear mucus from the lungs using physical therapy combined with mucus thinners taken through an inhaler or nebulizer. Mucolytics, such as dornase alfa, break up substances in the mucus, making it less sticky and easier to expel. Secretolytics, such as inhaled hypertonic saline solution, make mucus more watery by drawing water out of the tissues and into the airways. The effects of mucus thinners are temporary, so cystic fibrosis patients need to perform physical airway clearance to clear the thinned mucus.
Can a sweat test show CF?
A sweat test might show higher than normal salt levels, but not high enough for a CF diagnosis. A DNA test will then be used that looks for at least two copies of a cystic fibrosis mutation. There must be one copy on both chromosomes. The disease usually does not manifest if only one mutated gene is present.
What to do if you have CF?
These might include: Sinus surgery: Many people with CF have inflamed or infected sinuses. Your doctor may need to remove nasal polyps (growths inside your nasal passages). They can also do a procedure called an “ endoscopy and lavage” that suctions mucus from your airways. This will make it easier for you to breathe.
How to help a lung infection?
They may also help reduce the number of lung infections you get. For instance, clapping or pounding on your chest and back helps loosen mucus so you can cough more of it out. You can do different types of ACTs at home with the help of a family member or friend. Or, you might prefer to use a medical device.
Is there a cure for cystic fibrosis?
There’s no cure for cystic fibrosis (CF). But many treatments can reduce your symptoms and improve your quality of life. Here’s an overview of the most common.
How to help cystic fibrosis patients?
That’s why it’s important to find ways to manage stress. Yoga, meditation, exercise, hanging out with friends, and hobbies are all popular and effective ways to manage stress, anxiety, ...
How to help CF?
Exercise. Among its many benefits for people with CF, exercise builds lung capacity, helps with airway clearance, builds strong bones, and strengthens the heart and breathing muscles. Dedication to daily exercise keeps people with CF healthier, longer.
How far away should you be from someone with cystic fibrosis?
The 6-foot rule. People with cystic fibrosis are especially vulnerable to lung infections carried by other people with CF. That is why it’s important for people with CF to keep a distance of 6 feet from others with CF from a different household.
Why do people with CF need extra calories?
But these can’t just be empty calories. Due to their gastrointestinal system not digesting food properly, a condition called malabsorption, people with CF need extra nutrition to prevent malnutrition and failure to thrive as children. 3
How much time do you spend on CF?
It varies by individual, but the average amount of time an adult with CF spends on their treatments (medications, enzymes, and airway clearance) is 108 minutes per day, regardless of the severity of their disease. Caregivers of children with CF report 74 minutes ...
What is airway clearance?
Airway clearance helps loosen the thick, sticky mucus that tends to clog the lungs of people with CF. The type of airway clearance technique (ACT) used varies by age and which method the person with CF prefers. Parents must perform ACTs for infants and toddlers, while older children and adults perform their own.
What is the treatment for cystic fibrosis?
Recently developed treatments, called modulators as a class, restore the ability of cells to make the cystic fibrosis protein work to maintain normal levels of fluid in body secretions. This prevents the accumulation of mucus.
Why is cystic fibrosis monitored?
People of any age who have cystic fibrosis are typically monitored close ly to detect early changes in health status. This allows their care team to intervene before significant complications occur.
What is the condition that causes mucus to accumulate in the airways?
Cystic fibrosis is a multi-organ disease that affects the quality of body secretions and fluids. The condition is especially problematic in the respiratory tract. Cystic fibrosis causes thick mucus to accumulate in the airways. People who have the condition are also more prone to infections.
How long does cystic fibrosis live?
Life expectancy for people with cystic fibrosis in the United States is now reaching 50 years. Great advances in life expectancy have happened because of decades of research and hard work at all levels.
Is there a fixed regimen for respiratory disease?
Treatment options change and need to be tailored based on the degree of disease progression and severity in an individual person. There is no fixed regimen that applies across the board. For some people with more advanced respiratory disease, the treatment regimen will be more intensive than it would be for people with less severe forms of the disease.
Is cystic fibrosis inherited?
Cystic fibrosis is an inherited genetic condition . For an individual to be affected, two defective, or “mutated,” cystic fibrosis genes have to be inherited, one from each parent. The cystic fibrosis gene provides the instructions for a protein called cystic fibrosis transmembrane conductance regulator (CFTR). The CFTR protein is very important for cells in many organs to control the amount of salt and fluid that covers their surface.
Why is physiotherapy important for CF patients?
Physiotherapy is vital to people with CF, principally in developing and maintaining optimal airway clearance but also across a range of other vital functions including sinus management, exercise and even help with ingesting medicines.
Is lung transplant life saving?
For those who are receiving lessening effectiveness from existing treatments and therapies, a lung transplant is a daunting but life saving option. This could even be extended to transplantation of other organs such as the liver where the disease has critically affected their ability to function properly.
What is the best diet for CF patients?
Pathologist Dorothy Andersen advises for CF patients: “A low-fat, high-protein diet with a liberal allowance of vegetables, fruits and sugar and moderate restriction of starch. Supplementary vitamin A is essential and pancreatin and vitamin B complex are given.”
What supplements are used for CF?
Supplements would soon be widely used for extra calories, fat, and protein in the CF diet. Acid-resistant enzymes, Creon and Pancrease, are released. They are more effective than predecessor Cotazym, which was a powder whose absorption was affected by stomach acid.
What is azithromycin used for?
2000s. Azithromycin is used for patients with chronic bacteria Pseudomonas aeruginosa and for those with severe inflammation. IV antibiotics are used more often in early stages of infections rather than as a last resort. An inhaled medicine called Cayston is created to fight Pseudomonas.
When was the CF gene identified?
1980s. The CF Gene is identified in 1989. It is named the cystic fibrosis transmembrane conductance regulator (CFTR). The causes of CF are now better understood and the push for a cure gains momentum. The life expectancy for a CF patient is 12 in the United States and 20 in Canada.
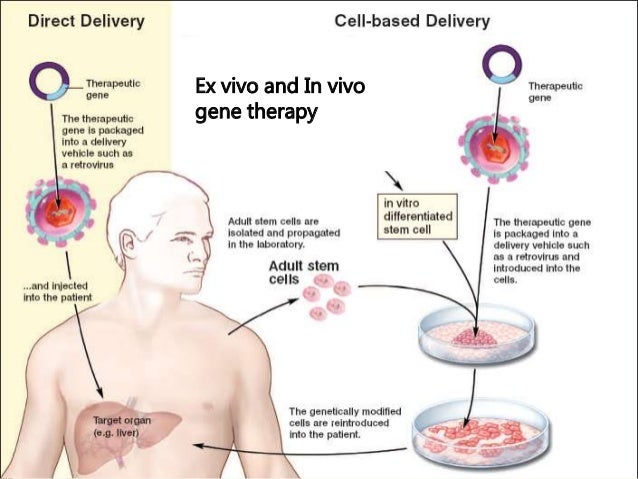
When were CF defects corrected?
CF defects are corrected in the lab in 1990. The idea is applied to three mouse models with varying but disappointing results. The mouse models opened the door to further in vivo experimentation of CFTR function and gene transfers. Gene therapy is thought to be the answer for a cure.
Where does Brad Dell live?
He received a double-lung transplant from UC San Francisco in January 2017, then cochlear implants nine months later. He now lives in Hawaii, where he was raised. Usually he's traveling the world, chugging coffee, mentoring college students, or studying theology. Otherwise, he's working as the director of columns at BioNews, the publisher of CF News Today. (OK, he's still drinking coffee while he works.) He writes to undo the taboos surrounding lung transplantation. You can learn more about his story by following @coffee.cats_ on Instagram or by visiting www.adamantiumjoy.com
What is Trikafta used for?
Food and Drug Administration today approved Trikafta (elexacaftor/ivacaftor/tezacaftor), the first triple combination therapy available to treat patients with the most common cystic fibrosis mutation.
Is Trikafta an orphan drug?
Trikafta also received orphan drug designation, which provides incentives to assist and encourage the development of drugs for rare diseases. Drugs approved under expedited programs are held to the same approval standards as other FDA approvals. Because of Trikafta’s benefit to the cystic fibrosis community, the FDA reviewed ...
Is Trikafta approved for cystic fibrosis?
Trikafta is approved for patients 12 years and older with cystic fibrosis who have at least one F508del mutation in the cystic fibrosis transmembra ne conductance regulator (CFTR) gene, which is estimated to represent 90% of the cystic fibrosis population.

Treatment
Clinical Trials
Coping and Support
Preparing For Your Appointment