What is the best treatment for PID?
PID is usually treated with antibiotics to provide empiric, broad spectrum coverage of likely pathogens.
What is the first line treatment for PID?
The CDC recommends the following for first-line treatment for outpatient therapy: Doxycycline (100 mg orally twice a day for 2 weeks) plus ceftriaxone 500 mg intramuscularly (IM) for one dose or cefoxitin 2 g IM with probenecid (1g orally) for one dose or another parenteral third-generation cephalosporin.May 13, 2021
Can I take doxycycline and flagyl together?
No interactions were found between doxycycline and Flagyl.
What is the main treatment for a female patient with pelvic inflammatory disease?
But there's no way to reverse any scarring or damage to the reproductive tract that PID might have caused. Treatment for PID most often includes: Antibiotics. Your doctor will prescribe a combination of antibiotics to start immediately.Apr 23, 2020
Diagnostic Considerations
Acute PID is difficult to diagnose because of the considerable variation in symptoms and signs associated with this condition. Women with PID often have subtle or nonspecific symptoms or are asymptomatic. Delay in diagnosis and treatment probably contributes to inflammatory sequelae in the upper genital tract.
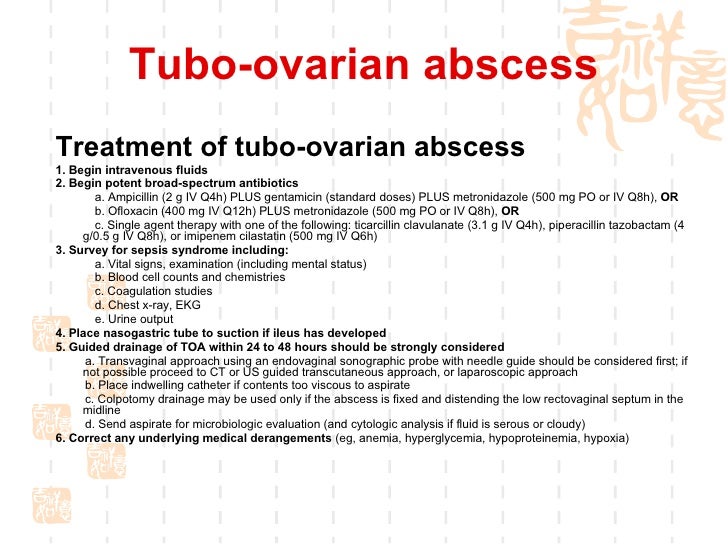
Treatment
PID treatment regimens should provide empiric, broad-spectrum coverage of likely pathogens. Multiple parenteral and oral antimicrobial regimens have been effective in achieving clinical and microbiologic cure in randomized clinical trials with short-term follow-up ( 1171 – 1173 ).
Intramuscular or Oral Treatment
IM or oral therapy can be considered for women with mild-to-moderate acute PID because the clinical outcomes among women treated with these regimens are similar to those treated with IV therapy ( 1158 ). Women who do not respond to IM or oral therapy within 72 hours should be reevaluated to confirm the diagnosis and be administered therapy IV.
Other Management Considerations
To minimize disease transmission, women should be instructed to abstain from sexual intercourse until therapy is complete, symptoms have resolved, and sex partners have been treated (see Chlamydial Infections; Gonococcal Infections). All women who receive a diagnosis of PID should be tested for gonorrhea, chlamydia, HIV, and syphilis.
Follow-Up
Women should demonstrate clinical improvement (e.g., defervescence; reduction in direct or rebound abdominal tenderness; and reduction in uterine, adnexal, and cervical motion tenderness) <3 days after therapy initiation.
Management of Sex Partners
Persons who have had sexual contact with a partner with PID during the 60 days preceding symptom onset should be evaluated, tested, and presumptively treated for chlamydia and gonorrhea, regardless of the PID etiology or pathogens isolated.
Special Considerations
The risk for penicillin cross-reactivity is highest with first-generation cephalosporins but is negligible between the majority of second-generation (e.g., cefoxitin) and all third-generation (e.g., ceftriaxone) cephalosporins ( 619, 631, 653, 656) (see Management of Persons Who Have a History of Penicillin Allergy).
What is the current management of PID?
Current management of PID requires easily reproducible investigations and antibiotics adapted to STI and vaginal microbiota. Current management of PID requires easily reproducible investigations and antibiotics adapted to STI and vaginal microbiota.
When to use condoms after PID?
The use of condoms is recommended (grade B). Vaginal sampling for microbiological diagnosis is recommended 3 to 6months after PID (grade C), before the insertion of an intra-uterine device (grade B), before elective termination of pregnancy or hysterosalpingography.
Why is PID important?
PID is of particular clinical and public health importance because it is associated with significant short- and long-term sequelae. Short-term sequelae include the development of tubo-ovarian abscesses requiring triple antibiotic therapy, perihepatitis, periappendicitis, and protracted hospitalization. Long-term sequelae include ectopic pregnancy, ...
What are the long term complications of PID?
Long-term sequelae include ectopic pregnancy, chronic pelvic pain (CPP), and tubal infertility because of scarring. Further, each episode of PID increases the risk of these long-term complications. Available international data have shown that the impact of PID among women in developing countries also is significant.
What are the consequences of PID?
Common adverse reproductive health consequences associated with PID include tubal infertility, chronic pelvic pain, and ectopic pregnancy. Centers for Disease Control and Prevention (CDC) provides evidence-based and expert-driven treatment guidelines for effective management of PID, but clinician adherence to the guidelines has been poor.
What is a PID?
The term PID refers to a spectrum of clinical disorders of the upper reproductive tract, including endometritis, salpingitis, tubo-ovarian abscesses, and pelvic peritonitis. These health states are caused when organisms ascend from the lower reproductive tract (vagina/cervix) into the endometrium, fallopian tubes, and related structures. Although PID is classified as a sexually transmitted infection and occurs rarely in female patients who have never initiated intercourse, the polymicrobial etiology of PID may include STIs, genital flora, enteric organisms, and agents typically causing respiratory infections. The role of N. gonorrhoeae and C trachomatis as causative agents in PID has been well established in the literature; however, new data from women clinically diagnosed as having mild-moderate PID indicates that almost 70% of patients have non– C trachomatis /non- N. gonorrhoeae PID. ( 8)
What is the purpose of a pediatric speculum examination?
However, it is still important that the pediatric clinician be prepared and equipped to perform a complete and thorough evaluation, including a speculum examination for visualization of the cervix and vagina and collection of endocervical and vaginal specimens, followed by a bimanual examination.
Is PID a sexually transmitted infection?
Although PID is classified as a sexually transmitted infection and occurs rarely in female patients who have never initiated intercourse, the polymicrobial etiology of PID may include STIs, genital flora, enteric organisms, and agents typically causing respiratory infections.
Is PID a clinical diagnosis?
The clinical diagnosis of PID is notoriously imprecise, but the use of surgical procedures that allow for greater precision (such as la paroscopy) are no longer considered a part of standard assessment. To complicate matters further, patients often do not present with the classically described PID presentation. An acute presentation with severe lower abdominal pain resulting in a shuffling gait or the “chandelier sign” on clinical examination is rare. The heterogeneity of infectious agents now causing PID is thought to contribute to the varied clinical presentations for which symptoms can range from mild to severe. Although infertility as an adverse outcome has been well documented in patients who have PID both prospectively and in retrospective studies of women with infertility, there is an additional subset of infertile women who experience the sequelae of PID without the classic findings.
What is the prevention of PID?
Prevention of PID includes screening for C. trachomatis and N. gonorrhoeae in all women younger than 25 years and those who are at risk or pregnant, plus intensive behavioral counseling for all adolescents and adults at increased risk of sexually transmitted infections.
Why is PID underdiagnosed?
PID is often underdiagnosed because of the wide variation and severity of symptoms. 8 Patients may be asymptomatic. Many women with tubal factor infertility have histologic evidence of PID despite having no previous diagnosis. 11, 12 The cardinal symptom of PID is the abrupt onset of lower abdominal or pelvic pain in a sexually active woman. 8 Symptoms can be subtle with mild bilateral lower abdominal pain that worsens with coitus, abnormal uterine bleeding, increased urinary frequency, dysuria, or abnormal vaginal discharge. Fever may also occur, but it is not the dominant symptom. Right upper quadrant pain that is worse with movement and breathing is caused by inflammation and adhesions of the liver capsule, such as in perihepatitis (i.e., Fitz-Hugh–Curtis syndrome).
What is PID in a sex?
Pelvic inflammatory disease (PID) includes an array of infectious processes that damage the endometrium, fallopian tubes, ovaries, and pelvic peritoneum. Sexually transmitted infections (STIs) cause most PID cases, but organisms associated with bacterial vaginosis (BV) have also been implicated.
What is empiric treatment for sex?
The diagnosis is made primarily on clinical suspicion, and empiric treatment is recommended in sexually active young women or women at risk for sexually transmitted infections who have unexplained lower abdominal or pelvic pain and cervical motion, uterine, or adnexal tenderness on examination.
What is PID in medical terms?
The diagnosis of PID is clinical, with imaging and more invasive studies reserved for cases of diagnostic uncertainty or concern for complications (e.g., tubo-ovarian abscess). 8, 13 Therefore, physicians should make the diagnosis and initiate treatment for PID if no other diagnosis is more likely in sexually active women younger than 25 years or in older women at risk for STIs who present with pain in the lower abdomen or pelvis and one or more of the clinical findings shown in Figure 1. 8
What is the function of Chlamydia trachomatis?
Damage to the epithelium by infection (typically Chlamydia trachomatis or N. gonorrhoeae) allows organisms to ascend the upper genital tract from the cervix. A variety of microbes have been isolated in PID. 9 The role of Mycoplasma genitalium, Gardnerella vaginalis, and Ureaplasma urealyticum in PID is not clear.
Do women with PID have HIV?
Women with PID who also have HIV have similar symptoms and respond similarly to treatment as those without HIV; however, women with HIV are at increased risk of tubo-ovarian abscesses and have higher rates of mycoplasma and streptococcal infections. Therefore, they need to be followed closely for response to treatment. 30
References
Workowski KA, et al. Centers for Disease Control and Prevention. Sexually transmitted infections treatment guidelines, 2021. MMWR Recomm Rep 2021;70:1-187.
Pediatric Empiric Antimicrobial Therapy Guidelines
This is a subsection of the UCSF Benioff Children’s Hospitals Empiric Antimicrobial Therapy Guidelines, developed by the Pediatric Antimicrobial Stewardship Programs at each campus to inform initial selection of empiric antimicrobial therapy for children at the UCSF Benioff Children’s Hospitals and affiliated outpatient sites.
What is the most important feature of PID?
Presence of a pelvic mass. PID can present with a vast array of clinical manifestations. Salpingitis is the most important feature of PID. Infection and inflammation of the endometrium, blood vessels and lymphatics without visually recognized salpingitis.
Is PID invasive?
The exact incidence of PID is unknown, because the disease cannot be diagnosed reliably from clinical symptoms and signs. Direct visualization of the fallopian tubes by laparoscopy is the best single diagnostic test, but it is invasive, lacks sensitivity, and is not used routinely in clinical practice.