
Can you still get monoclonal antibodies?
Jan 06, 2022 · Monoclonal antibody therapy is a way of treating COVID-19 for people who have tested positive, have had mild symptoms for seven days or less, and are at high risk for developing more serious symptoms. The goal of this therapy is to help prevent hospitalizations, reduce viral loads, and lessen symptom severity.
How soon should you get monoclonal antibodies?
Nov 09, 2021 · A single dose of REGEN-COV, a combination monoclonal antibody therapy, reduced the risk of COVID-19 by 81.6% several months after a single dose. UNC School of Medicine’s Myron Cohen, MD, leads monoclonal antibody research efforts as part of the NIH-sponsored COVID Prevention Network. Regeneron Pharmaceuticals, Inc. announced additional …
How long after Regeneron to get booster?
Dec 22, 2021 · How Long Do Monoclonal Antibodies Last? The mAb treatments have been shown to “reduce the risk of COVID-19 by 81.6% several months after a single dose,” according to the UNC School of Medicine. With recent advancements in healthcare regarding these treatments, it seems mAbs may pave the way to creating a treatment for lasting immunity to COVID. Will …
Are there side effects of monoclonal antibody treatment?
Monoclonal antibody therapy may give you some protection from getting sick again from COVID-19 during those 90 days. However, wearing a mask in public places is still important if you have a weakened immune system or if you are at increased risk for getting very sick.
Can I get the COVID-19 vaccine if I was treated with monoclonal antibodies or convalescent plasma?
If you were treated for COVID-19 symptoms with monoclonal antibodies or convalescent plasma, you should wait 90 days before getting a COVID-19 vaccine.
How long does immunity last after the Pfizer COVID-19 vaccine?
Antibodies able to block the omicron coronavirus variant last four months after a third dose of Pfizer-BioNTech's vaccine, according to a study published Jan. 22 by bioRxiv.Jan 25, 2022
How long does it take to develop immunity after a COVID-19 infection?
Although the immune correlates of protection are not fully understood, evidence indicates that antibody development following infection likely confers some degree of immunity from subsequent infection for at least 6 months.
What are monoclonal antibodies used for during the COVID-19 pandemic?
Monoclonal antibodies are laboratory-made proteins that mimic the immune system's ability to fight off harmful pathogens such as viruses, like SARS-CoV-2. And like other infectious organisms, SARS-CoV-2 can mutate over time, resulting in certain treatments not working against certain variants such as omicron.Jan 24, 2022
How long do COVID-19 vaccines last?
It is normal for virus-fighting antibodies—such as those that are stimulated by a COVID-19 vaccine—to wane over time. Monitoring antibody levels in the blood is one way to measure vaccine efficacy and research has found that protection remains high for six months after the second shot of a Pfizer or Moderna vaccine.Mar 30, 2022
What's the efficacy of the Pfizer COVID-19 vaccine after 90 days?
Among adults who received 2 doses of the Pfizer-BioNTech (BNT162b2) mRNA COVID-19 vaccine, the risk for SARS-CoV-2 infection increased gradually after 90 days, according to results of a study published in BMJ.Dec 16, 2021
How strong is immunity after a COVID-19 infection?
How Strong Is Immunity After a COVID-19 Infection? About 90% of people develop some number of protective antibodies after a COVID-19 infection, according to the CDC. But how high those levels climb appears to be all over the map.Nov 9, 2021
Does your immune system get stronger after COVID-19?
Any time you catch a virus and recover from the illness, you retain antibodies. These antibodies help your body fight off future infections so that you either don't get sick or have milder symptoms.Dec 6, 2021
Can you get COVID-19 if you already had it and have antibodies?
It is important to remember that some people with antibodies to SARS-CoV-2 may become infected after vaccination (vaccine breakthrough infection) or after recovering from a past infection (reinfected).Nov 10, 2021
Are antibodies beneficial during the COVID-19 pandemic?
When reinfections or breakthrough infections happen, having antibodies plays an important role in helping prevent severe illness, hospitalization, and death. For many diseases, including COVID-19, antibodies are expected to decrease or “wane” over time.Nov 10, 2021
Should you still get the COVID-19 vaccine if you were treated with monoclonal antibodies?
If you were treated for COVID-19 with monoclonal antibodies or convalescent plasma, there is no need to delay getting a COVID-19 vaccine.Feb 17, 2022
What is the difference between monoclonal antibodies and the COVID-19 vaccine?
COVID-19 vaccines help stimulate and prepare a person's immune system to respond if they are exposed to the virus. However, monoclonal antibodies boost the immune system only after a person is already sick, speeding up their immune response to prevent COVID-19 from getting worse.Nov 8, 2021
What is Monoclonal Antibody Therapy and How Does it Work?
The U.S. Food and Drug Administration (FDA) defines mAbs as “laboratory-produced molecules that act as substitute antibodies that can restore, enhance, or mimic the immune system’s attack on cells.” In other words, mAbs help your body to stop COVID-19 from causing more serious symptoms that could lead to hospitalization and death.
Who is Eligible for Monoclonal Antibody Treatment?
As of December 2021, the Centers for Disease Control and Prevention (CDC) explains that the mAb COVID treatments are only “for people at high risk of disease progression.” The FDA supports this statement, mentioning that those who are at high risk and who “have been exposed to an individual infected with SARS-CoV-2 consistent with close contact criteria per [the CDC]” may also be eligible for treatment..
When Should You Get the Monoclonal Antibodies Treatment?
Experts at the National Institutes of Health say it is extremely important to get the mAb treatment as soon as you have tested positive for COVID-19 and “within 10 days of symptom onset.” Those who are at high risk and had a recent COVID-19 exposure are also candidates for this treatment and should receive it soon after their exposure.
What You Can Expect When Getting This COVID Treatment
According to the FDA, the mAb treatment received Emergency Use Authorization (EUA) in November 2020. While it has been a year since the emergence of this treatment, it has prompted many questions:
Where Can I Receive The mAb Treatment?
Select healthcare providers in Colorado offer monoclonal antibody treatments. Advanced Urgent Care & Occupational Medicine is partnering with Platte River Medical Clinic in Brighton, Colorado, to offer mAb treatments to those who qualify.
What is the function of antibodies?
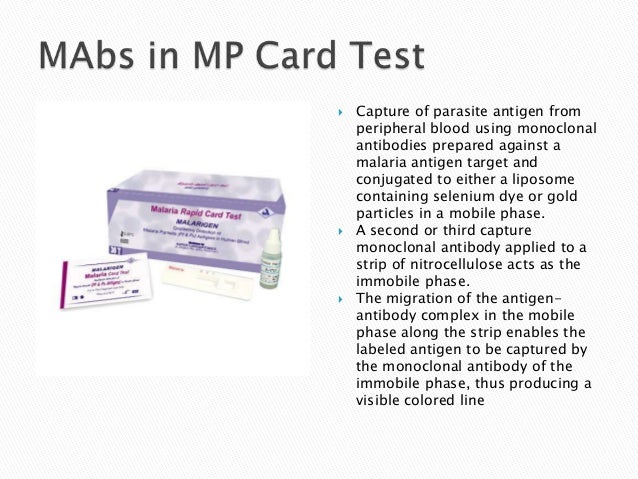
Antibodies are proteins that exist in our bodies as part of our immune system to recognize and defend against harmful viruses and bacteria. Monoclonal antibodies are made in a laboratory and designed to target a specific virus or bacteria.
What antibody is used to block the virus?
Monoclonal antibodies against COVID-19 attach to the virus to block it from entering human cells. The monoclonal antibody protein also “marks” the virus to be broken down by the immune system and cleared from the body.
Can monoclonal antibodies cause nausea?
Most people tolerate monoclonal antibody infusions very well. Some people may experience infusion-related side effects, such as nausea and dizziness, that are short-lived and go away on their own. As with any medication, there is the potential for mild or more severe allergic reactions, which are uncommon.
What exactly is in a monoclonal antibody treatment and how do they work?
In the United States, there are three monoclonal antibody treatments with FDA emergency use authorization for the treatment of COVID-19: bamlanivimab plus etesevimab, developed by Eli Lilly; casirivimab plus imdevimab, made by Regeneron Pharmaceuticals; and sotrovimab, which is manufactured by GlaxoSmithKline.
Who is eligible for monoclonal antibody treatment?
If you believe you are at high risk for progression of severe COVID-19, including hospitalization or death, you may be eligible for the the COVID-19 antibody cocktails.
How effective is it?
Ginde said it can be a life-saving treatment when administered in time. Numerous trials have shown that the treatment can be effective at reducing the risk of hospitalization and death for people at risk of severe COVID.
When do I need to get the treatment in order for it to work?
The monoclonal antibody treatments are meant for mild to moderate COVID cases in adults and children over 12 to prevent the progression of severe COVID.
How can I get a monoclonal antibody treatment for COVID-19?
The ease of access varies state by state, as the Department of Health and Human Services determines how much of the national supply gets distributed on a weekly basis. Then, different state and territorial health departments decide which areas receive it and how much.
Are there side effects?
It’s rare but possible to have side effects. At least 1% of subjects receiving Regeneron’s antibody cocktail in a Phase 3 trial got skin redness and itchiness at the injection site, according to the FDA.
How much does it cost?
The federal government is covering the cost of the monoclonal antibody therapies, so it is free to get, but there might be an administration cost billed to your insurance if you have one.
How long does it take to get monoclonal antibody infusion treatment?
During the procedure, patients are seated in a comfortable chair, hooked up to an IV containing the antibody treatment, and administered the drug cocktail intravenously for approximately 20 minutes.
Where can I find a monoclonal antibody infusion treatment center near me?
There are dozens of hospitals and healthcare providers in the Houston area offering monoclonal antibody infusions. KPRC 2 Investigates has a map below that can guide you to a provider near you. Just hover over one of the colored circles on the map to get the name and address of the provider nearest to you.
What are antibodies?
Antibodies are the result of our immune system fighting an infection or receiving a vaccine. They are unique proteins that help our immune cells (called white blood cells) effectively kill bacteria or viruses. But making them is a process that takes time.
How long does it take to develop COVID-19 antibodies?
As mentioned above, there are two different ways your immune system can learn to make antibodies and memory cells for a virus or bacteria: natural immunity and vaccine-induced immunity.
Does COVID-19 immunity protect against newer strains of the virus?
Researchers in different areas of the world started finding new strains — or variants — of COVID-19 in November 2020. The Delta variant is the predominant strain in the U.S. right now. However, several other variants exist and are being monitored by experts.
Will I need to get the COVID-19 vaccine every year?
It’s possible that we will need regular booster vaccines, but more research is still needed. Currently, a third dose of Pfizer’s Comirnaty vaccine is recommended for certain higher-risk groups and a booster shot is authorized for certain populations.
The bottom line
Antibodies are the proteins our bodies make to fight infections. Antibodies can be created by getting sick or getting vaccinated. This process is part of how we gain immunity to bacteria or viruses.
