What is the optimal duration of antibiotic therapy?
- consider microbiological testing to direct therapy (e.g. ...
- use the current version of Therapeutic Guidelines: Antibiotic, or available local guidelines
- know why you are prescribing the antibiotic (document indication and duration in the medical record)
Do antibiotics increase the risk of sepsis?
adverse drug events (ADE) CDC Infectious Disease sepsis. New research from the Centers for Disease Control and Prevention (CDC) shows that treatment with antibiotics can increase the risk of sepsis among patients. The CDC research was presented last week at IDWeek, a joint annual meeting of the Infectious Disease Society of America, the Society for Healthcare Epidemiology of American, the HIV Medicine Association, and the Pediatric Infectious Diseases Society.
How long does sepsis take, after infection?
On average, the recovery period from this condition takes about three to ten days, depending on the appropriate treatment response, including medication. Severe sepsis requires immediate treatment in the critical care area for a period of one month or more. Recovery is achievable, but it takes a longer time.
How is sepsis diagnosed and treated?
- Rapid tests for common infections (strep throat, influenza, and skin infections)
- Urine or stool testing
- Sputum testing
- Pus culture (if the patient has a wound)
- Coagulation tests to detect coagulopathy due to sepsis
- Cerebrospinal fluid (CSF) study to rule out meningitis

How long do you take antibiotics for sepsis?
Ideally, antibiotic treatment should start within an hour of diagnosis to reduce the risk of serious complications or death. Intravenous antibiotics are usually replaced by tablets after two to four days. You may have to take them for 7 to 10 days or longer, depending on the severity of your condition.
How long does sepsis last with treatment?
In mild sepsis, complete recovery is possible at a quicker rate. On average, the recovery period from this condition takes about three to ten days, depending on the appropriate treatment response, including medication.
How long does it take to get better from sepsis?
This is known as Post Sepsis Syndrome (PSS) and usually lasts between 6 and 18 months, sometimes longer. Because you may look well, others (including your employer, doctor, or family) may be unaware of the problems and expect you to be better now. Don't suffer in silence.
Do antibiotics always cure sepsis?
Antibiotics alone won't treat sepsis; you also need fluids. The body needs extra fluids to help keep the blood pressure from dropping dangerously low, causing shock.
How long is hospital stay for sepsis?
Average sepsis-related hospital length of stay improved from 3.35 days to 3.19 days to 2.94 days, a 4.8% and 12.1% reduction, respectively, relative to the pre-implementation baseline, and remained consistent at 2.92 days in the post-implementation steady-state period.
Can sepsis come back after antibiotics?
Recurrent sepsis is a common cause of hospital readmission after sepsis. Our study demonstrates that, while two-thirds of recurrent sepsis hospitalizations had the same site of infection, just one fifth were confirmed to be the same site and same organism as the initial sepsis hospitalization.
What is the best antibiotic for sepsis?
The majority of broad-spectrum agents administered for sepsis have activity against Gram-positive organisms such as methicillin-susceptible Staphylococcus aureus, or MSSA, and Streptococcal species. This includes the antibiotics piperacillin/tazobactam, ceftriaxone, cefepime, meropenem, and imipenem/cilastatin.
What is the fastest way to cure sepsis?
Doctors and nurses should treat sepsis with antibiotics as soon as possible. Antibiotics are critical tools for treating life-threatening infections, like those that can lead to sepsis.
Can you walk again after sepsis?
Physical Rehabilitation After Sepsis After a patient has sepsis, they will usually begin rehabilitation in the hospital to build up strength and regain their muscle movement. The hospital staff will assist with bathing, sitting up, standing, walking, and taking the patient to the restroom.
How long do IV antibiotics take to work?
Antibiotics begin to work right after you start taking them. However, you might not feel better for 2 to 3 days. How quickly you get better after antibiotic treatment varies. It also depends on the type of infection you're treating.
What are the signs of recovery from sepsis?
Recovering from sepsisfeeling very tired and weak, and difficulty sleeping.lack of appetite.getting ill more often.changes in your mood, or anxiety or depression.nightmares or flashbacks.post-traumatic stress disorder (PTSD)
What happens if the antibiotics don't work with sepsis?
If not treated quickly it can lead to organ failure or death. Early symptoms can include a high temperature and a fast heartbeat.
Is sepsis a medical emergency?
Sepsis is a medical emergency and life-threatening condition due to a dysregulated host response to infection, which is time-dependent and associated with unacceptably high mortality. Thus, when treating suspicious or confirmed cases of sepsis, clinicians must initiate broad-spectrum antimicrobials ….
Is sepsis a life threatening condition?
Sepsis is a medical emergency and life-threatening condition due to a dysregulated host response to infection, which is time- dependent and associated with unacceptably high mortality. Thus, when treating suspicious or confirmed cases of sepsis, clinicians must initiate broad-spectrum antimicrobials within the first hour of diagnosis.
How many days of antibiotics for cystitis?
Early studies in patients with cystitis noted that single-dose therapy was suboptimal compared to multiday therapy [ 33 ], establishing that most serious infection would presumably at least require multiple days of antibiotics.
What is source control in sepsis?
Source control of septic foci has long been recognized as a key intervention in the nonantimicrobial management of sepsis [ 63–65 ], and typically refers to procedures such as draining infected fluid collections, debriding infected tissues, removing infected devices or foreign materials, and correction of anatomic abnormalities which either predispose to microbial contamination or reduce antimicrobial exposure. On a macroscopic level, these procedures reduce microbial burden and facilitate antibiotic penetration into sequestered sites, which could otherwise serve as reservoirs of persistent infection and acquisition of drug resistance. The importance of source control is weighted in the SSC guidelines as a best practice statement, with emphasis on early implementation as soon as medically and logistically feasible [ 18 ]. Inability to achieve control of a known source is an accepted indication for extending duration of therapy, and indeed nearly all trials of shortened treatment durations have explicitly excluded patients with an uncontrolled source or those requiring active drainage.
What is the most studied biomarker for use in the diagnosis of bacterial infections and guidance of antibiotic therapy?
Procalcitonin has been the most extensively studied biomarker for use in the diagnosis of bacterial infections and guidance of antibiotic therapy. Procalcitonin is a short-lived hormone (precursor to calcitonin) that is rapidly induced by the inflammatory cytokines associated with bacterial infection.
Does de-escalation decrease duration of therapy?
Interestingly, de-escalation was not associated with decreased duration of therapy, although 1 study did report fewer days of antipseudomonal β-lactam and broad-spectrum gram-positive antibiotics associated with de-escalation [ 94 ].
Is there a trial on antibiotics for sepsis?
There is a notable lack of trials on the duration of antibiotic therapy in sepsis. As previously mentioned, none of the landmark sepsis trials which have shaped current sepsis management [ 4–6, 24–26] reported any specific antibiotic regimens, durations, or microbiologic data.
Optimal Antimicrobial Treatment Duration in Sepsis
There is limited guidance on the optimal duration of antimicrobial therapy for sepsis patients.
CONCLUSIONS
There is a lack of data to aid the clinician on the frequency, classes of agents to use and duration of antimicrobial therapy in sepsis patients
How long should you use antibiotics for septic shock?
Use combination therapy (multiple drugs active against the same organisms, through different mechanisms of action) when appropriate, but for only a limited time (3-5 days). Combination therapy is recommended by the Surviving Sepsis Campaign for patients with septic shock ...
How long can you use antimicrobials?
When using combination therapy empirically (without positive culture data or a clear site of infection), limit use to 3-5 days, then eliminate one or more of the antimicrobials being used. If positive cultures and sensitivity data are available sooner than 3-5 days, narrow antibiotic use as soon as data are available.
What should be chosen to cover all the likely pathogens?
Antimicrobials should be chosen that cover all the likely causative pathogens -- nearly always including bacteria, but sometimes also fungi and/or viruses. Antimicrobials should be selected that are expected to penetrate into the presumed infected tissues.
Is PulmCCM affiliated with the Surviving Sepsis Guidelines?
PulmCCM is not affiliated with the Surviving Sepsis Guidelines or the Surviving Sepsis Campaign. Get our weekly email update , and explore our library of practice updates and review articles. PulmCCM is an independent publication not affiliated with or endorsed by any organization, society or journal referenced on the website.
What is septic shock?
Septic shock was defined as patients needing vasopressors or an initial lactate greater than four. Severe sepsis was defined based on signs of end organ dysfunction, including laboratory abnormalities, one or more episodes of hypotension, or need for mechanical or noninvasive ventilation.
Is it a case by case decision to delay antibiotics?
It is a decision to be made on a case-by-case basis, is dependent on the patient’s presentation and co-morbidities, and the risk of delaying antibiotics must be balanced with the potential harm of giving unnecessary antibiotics. A potential harm that is still relatively unclear.
Is it better to take antibiotics after sepsis?
Early antibiotics appear to be better, but again, this is for patients with “recognized” sepsis and not necessarily all undifferentiated patients who meet SIRS criteria. Take Home Points. Current guidelines and quality measures stress the importance of timely antibiotics after recognition of sepsis.
Is antibiotics important for sepsis?
Antibiotics are clearly an important part of sepsis management, with earlier antibiotics appearing to be most important in patients with septic shock. However, the data are currently insufficient to specify an exact time point for initiation of antibiotics in septic patients.
Can sepsis be identified in retrospect?
Most of the above studies identified patients with sepsis in retrospect, separated them from those that were determined to have an inflammatory or viral process, and studied timing of antibiotics in the septic patients alone.
Do antibiotics affect sepsis?
Early antibiotics seem to affect mortality in sepsis, and this effect appears larger in patients with septic shock. If the patient is hypotensive and there is concern for infection, antibiotics are warranted.
How long does it take to get antibiotics?
The median time to antibiotics was 26 minutes (interquartile range 19-34) before emergency department arrival for the intervention group and 70 minutes (interquartile range 36-128) after arrival for the control group.
What is the mortality rate for septic shock?
Outcomes have improved over the years in line with a focus on intravenous fluids, appropriate antimicrobials, and other supportive measures, but for septic shock, mortality remains at 30% to 50%. The 2017 Surviving Sepsis Campaign guidelines ...
Should antibiotics be given in septic shock?
Countries with longer response time should still consider giving antibiotics, especially in patients with septic shock. Although the PHANTASi trial did not reveal a benefit to prehospital antibiotics for cases identified by systemic inflammatory response syndrome criteria, feasibility of prehospital recognition and treatment ...
Abstract
Sepsis is a common consequence of infection, associated with a mortality rate > 25%. Although community-acquired sepsis is more common, hospital-acquired infection is more lethal. The most common site of infection is the lung, followed by abdominal infection, catheter-associated blood steam infection and urinary tract infection.
Background
Sepsis is a common and life-threatening illness in the ICU, requiring timely and effective antimicrobial therapy. The aims of this review are to identify the most common sites of sepsis, the likely pathogens, and the optimal approach to antimicrobial therapy.
Sepsis epidemiology, infection site and pathogens
Sepsis is a life-threatening organ dysfunction syndrome caused by a dysregulated host response to infection, associated with a mortality rate over 25%, that has been designated a global health priority [ 1 – 3 ]. The majority of sepsis is community-acquired, and progression can be insidious, making diagnosis difficult [ 3, 4 ].
The importance of early appropriate and timely therapy
Timely administration of appropriate antibiotic therapy (i.e., with activity in vitro against the causative pathogens) is the cornerstone of the management of serious ICU infections [ 1 ]. Observational, prospective and retrospective studies support the use of appropriate empiric antibiotic therapy in sepsis and septic shock [ 16 – 19 ].
Biomarkers to guide sepsis therapy
Clinical and biological signs of sepsis are neither sensitive nor specific, particularly in older patients and the immunocompromised, making decisions about starting and stopping antibiotics challenging in ICU patients [ 5 ].
Antibiotic therapy: principles of use and new agents
While appropriate therapy refers to the use of an antimicrobial agent to which the etiologic pathogen is sensitive, it is also necessary to administer the right dose, at the optimal time, that penetrates into the site of infection.
Pneumonia: initial empiric therapy for CAP, HAP, VAP
Severe community acquired pneumonia (CAP) [ 56 – 59 ].
How to treat sepsis quickly?
Research shows that rapid, effective sepsis treatment includes: Giving appropriate treatment, including antibiotics . Maintaining blood flow to organs. Sometimes surgery is required to remove tissue damaged by the infection. Doctors and nurses should treat sepsis with antibiotics as soon as possible.
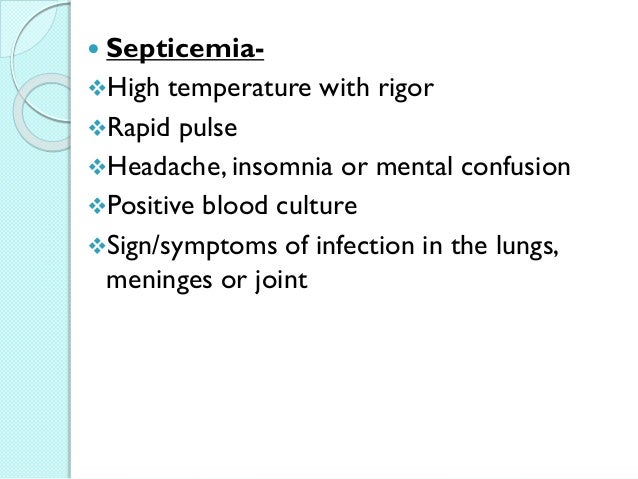
What are the symptoms of sepsis?
Fever. Low blood pressure. Increased heart rate. Difficulty breathing. Doctors also perform lab tests that check for signs of infection or organ damage. Doctors also perform specific tests to identify the germ that caused the infection that led to sepsis.
Can antibiotics help with sepsis?
Doctors and nurses should treat sepsis with antibiotics as soon as possible. Antibiotics are critical tools for treating life-threatening infections, like those that can lead to sepsis. However, as antibiotic resistance grows, infections are becoming more difficult to treat.
