Pan-retinal photocoagulation (PRP): The first line of proliferative diabetic retinopathy
Diabetic Retinopathy
A complication of diabetes where blood vessels in the eye are damaged.
Full Answer
How do you treat diabetic retinopathy with laser?
Mar 15, 2018 · The aim of laser PRP treatment is to destroy the areas where there is capillary non‐perfusion and retinal ischaemia as it is in these ischaemic areas where VEGF, a permeability and angiogenic factor, is produced. Lasers act by inducing thermal damage after absorption of energy by tissue pigments.
What are the treatment options for Proliferative retinopathy without laser?
Feb 02, 2022 · If you have advanced diabetic retinopathy, your doctor may use a type of laser treatment called scatter laser surgery as part of your treatment plan. In scatter laser surgery (sometimes called panretinal photocoagulation), your doctor will use a medical laser to shrink blood vessels in your eye that are causing vision problems. You may also need other …
What is the first-line treatment for Proliferative diabetic retinopathy?
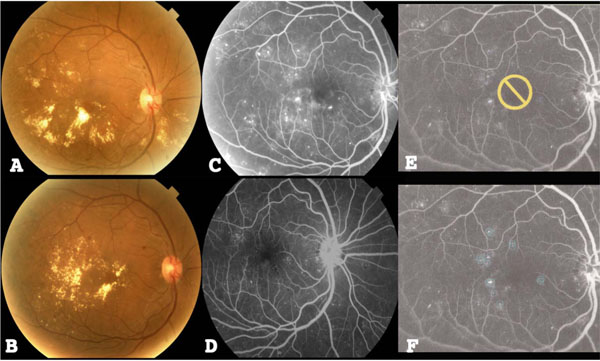
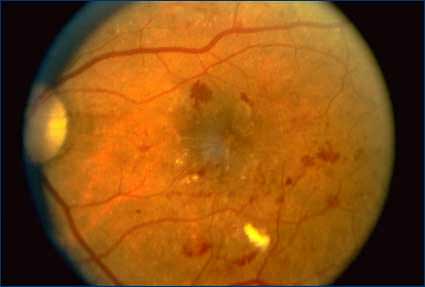
Abstract. Background: Diabetic retinopathy (DR) is a chronic progressive disease of the retinal microvasculature associated with prolonged hyperglycaemia. Proliferative DR (PDR) is a sight-threatening complication of DR and is characterised by the development of abnormal new vessels in the retina, optic nerve head or anterior segment of the eye. Argon laser photocoagulation …
Is laser photocoagulation effective for diabetic retinopathy and diabetic macular edema?
Oct 22, 2013 · Conventional retinal laser photocoagulation for diabetic retinopathy is typically performed with a continuous wave (cw) laser at 514 or 532 nm with exposure durations from 100 to 200 ms, spot sizes from 100 to 500 µm, and powers from 250 to 750 mW.
What type of laser treatment is used for diabetic retinopathy?
If you have diabetic retinopathy, your doctor may use a type of laser treatment called scatter laser surgery as part of your treatment plan. You may also need other treatments, like injections, in addition to laser treatments.
What is the treatment for diabetic retinopathy?
If you have diabetic retinopathy, your doctor may use a type of laser treatment called scatter laser surgery as part of your treatment plan. You may also need other treatments, like injections, in addition to laser treatments. Learn more about diabetic retinopathy. Scatter laser surgery (sometimes called panretinal photocoagulation) ...
Can you see light with scatter laser?
Your vision will be blurry for the rest of the day, so you’ll need someone to drive you home. You may need more than 1 session of scatter laser surgery. Like any surgery, this treatment has risks. It can cause loss of peripheral (side) ...
Can you see light with laser eye surgery?
Your vision will be blurry for the rest of the day, so you’ll need someone to drive you home. You may need more than 1 session of scatter laser surgery. Like any surgery, this treatment has risks.
Is scatter laser surgery safe?
Like any surgery, this treatment has risks. It can cause loss of peripheral (side) vision, color vision, and night vision. But for many people, the benefits of this treatment outweigh the risks. Talk with your doctor to decide if scatter laser surgery is right for you. Last updated: May 29, 2019.
Can scatter laser surgery cause night vision?
But for many people, the benefits of this treatment outweigh the risks. Talk with your doctor to decide if scatter laser surgery is right for you. Last updated: May 29, 2019.
How to get rid of blurry vision?
Your vision will be blurry for the rest of the day, so you’ll need someone to drive you home. You may need more than 1 session of scatter laser surgery.
Is laser photocoagulation effective for PDR?
Small clinical studies suggested laser photocoagulation was a promising modality for treating PDR, and the Diabetic Retinopathy Study (DRS) in the 1970s established panretinal photocoagulation (PRP) as an effective treatment for PDR.
Can laser therapy cause retinal scarring?
Laser therapy is typically titrated to a visible clinical effect (graying or whitening of the retina), which corresponds to necrosis of the photoreceptors, and at higher settings, to the inner retina. Although clinically highly effective at halting angiogenesis, this can lead to unwanted side effects, including significant discomfort during application for many patients, permanent retinal scarring, and decreased peripheral, color, and night vision. Systematic clinicopathological analysis of laser-induced retinal lesions over time has demonstrated that exposures of 100 ms and longer typically produce retinal lesions that affect not only RPE and photoreceptors, but also the inner nuclear layer (INL), ganglion cell layer (GCL), and nerve fiber layer (NFL). Arcuate nerve fiber and visual field defects can result from laser lesions that affect the inner retina. PRP can also exacerbate diabetic macular edema (DME).
What is laser therapy?
Laser therapy is typically titrated to a visible clinical effect (graying or whitening of the retina), which corresponds to necrosis of the photoreceptors, and at higher settings, to the inner retina.
What is the DRS?
The DRS was the seminal work establishing PRP as an efficacious treatment for PDR. The DRS was a prospective, multicenter, randomized-controlled trial sponsored by the National Eye Institute. It began in 1971 and included over 1700 patients at 15 centers. One eye of each patient was randomly assigned to immediate laser treatment with either a xenon arc or argon laser and the second eye served as a control without treatment. Treated eyes received photocoagulation to neovascularization of the retina elsewhere (NVE) and scatter photocoagulation in 1 or 2 sessions to beyond the vortex vein ampulae (the equator), with burns separated by 1 burn diameter. Argon laser treatment also involved localized treatment to NVD. Argon treatment specified 800 to 1600 spots, 500 µm burn diameter, and 100 millisecond (ms) pulse duration. Xenon arc patients were treated with 400–800 spots of 3 degrees or 200–400 spots of 4.5 degrees. Patients were included if they had a best-corrected visual acuity (BCVA) of 20/100 or better in both eyes and the presence of PDR in one eye or severe nonproliferative diabetic retinopathy in both eyes. The primary outcome measurement was severe vision loss, defined as BCVA less than 5/200 at 2 consecutive visits 4 months apart.
Abstract
This review highlights indications and evidence on laser therapy in the management of diabetic retinopathy and diabetic macular edema.
Introduction
Laser (Light Amplification by Stimulated Emission of Radiation) therapy is utilized widely in nearly all fields of medicine including ophthalmology, particularly in the treatment of retinal vascular diseases such as proliferative diabetic retinopathy (PDR), diabetic macular edema (DME), retinal vein occlusions, central serous chorioretinopathy, choroidal neovascularization, and vascular tumors [ 1 ].
How Does Retinal Laser Therapy Treat Diabetic Eye Disease?
The principle of retinal laser therapy resulting in therapeutic effects in the target retinal tissue is based upon the absorption of light by ocular pigments, predominantly in the retinal pigment epithelium (RPE) and choroid [ 9, 10] melanin and hemoglobin.
Conventional Photocoagulation
Conventional laser photocoagulation has numerous applications in the treatment of retinal disease, including diabetic retinopathy, retinal vein occlusions, sickle cell retinopathy, and retinal tears.
Modern Scanning Laser Photocoagulation
As laser technology has evolved and improved over the last several decades, emphasis has been placed on developing modifications to conventional retinal laser therapy in order to minimize retinal damage and adverse side effects, while maintaining the excellent therapeutic effect of the conventional approach.
Selective Retinal Therapy
As noted above, conventional retinal photocoagulation is limited in its use for macular conditions because of the risk of vision loss from central scars (resulting in scotomas) and expansion of the laser scar over time.
Subthreshold Diode Micropulse Laser
Subthreshold diode micropulse (SDM) laser is another novel laser modality for photocoagulation designed to minimize collateral tissue damage for treatment of the macula.
Do you need a laser for pre-proliferative retinopathy?
Nearly all eyes with severe pre-proliferative retinopathy needed laser, but increasingly anti-VEGF injections are taking over. Eyes with mild pre-proliferative do not need laser;
Is laser used for retinopathy?
Laser for pre-proliferative (none-proliferative) retinopathy. Sometimes laser is needed for pre-proliferative retinopathy: the treatment is similar to that of maculopathy and proliferative retinopathy. Nearly all eyes with severe pre-proliferative retinopathy needed laser, but increasingly anti-VEGF injections are taking over.
Can you use a laser for diabetic maculopathy?
Laser for diabetic maculopathy. Anti -VEGF injections are taking over in the treatment of maculopathy, but this treatment is still needed occasionally or when injections are not possible . Laser for diabetic maculopathy is also discussed here . An average of 300 burns are needed. This type of laser is not particularly painful, ...
Can you have retinopathy without laser?
Without laser proliferative retinopathy is often blinding, so both patients and doctors may be left with little alternative to enduring and carrying out this often unpleasant treatment. Again, control of diabetes as for maculopathy above is very helpful where possible in the long term.
Where is laser eye exam done?
Laser is usually carried out in a darkened room in clinic. Anaesthetic drops are dropped into your eye, a contact lens is placed on your eye, and you have to sit at a laser slit lamp. This is virtually the same machine as that used for the regular examination, but a laser has been added on.
How long does a laser flash last?
Each bright flash lasts for about 0.02 seconds. The commonest laser is Argon Green, wavelength 530nm, but other wavelengths can be used and most are equally effective. Other types of light were used before laser was introduced.
Do you need anti-VEGF injections instead of laser?
Anti-VEGF injections (and less often intravitreal steroids) are often needed in addtion or instead of laser: they do not seem to have a significant permanent benefit for most patients. Regular anti-VEGF injections usually reduce macular oedema and improve vision in ~50% of patients. Treat and exxtend protocol.
