
How do you get rid of vascular calcifications?
Doctors treat plaque-clogged blood vessels in a variety of ways, including vascular surgery and medicine. Lifestyle changes — quitting smoking, eating healthier foods, and starting to exercise — can decrease the chances of plaque and calcifications forming.
Can vascular calcification be reversed?
Strategies to control Ca and P levels in patients with ESRD have met with early success in preventing progression of vascular calcification. Whether or not vascular calcification can be reversed is not yet known, but exciting new studies suggest that this may be possible in the future.
How can calcification be treated?
Treatment. People with painless joint or tendon calcification typically do not need treatment. No treatments can remove calcium deposits from the cartilage of the joints, so doctors tend to rely on glucocorticoid injections, oral colchicine, and NSAIDs to relieve any pain and underlying inflammation.
How do you remove calcium from arteries naturally?
Eat a balanced diet composed of all essential nutrients. Exercise can decrease the buildup calcium and cholesterol inside the artery. Exercise burns body fat and it also does not allow the fat to stay for a long time in the blood. Reduce your sodium intake.
How do you reduce calcium deposits in your arteries?
So, you can prevent calcium buildup in your arteries by choosing a diet rich in vitamin K2 and exercising regularly. Both these things will help circulation and prevent plaque that leads to calcification. The key is to avoid saturated fat (to be kept under 7 percent) and dietary cholesterol.
Can statins reduce calcification?
Two included studies reported an inverse association, which is in tune with recent theory that statins stabilize plaques by promoting calcification while lowering LDL cholesterol (1); another two reported no association, which is consistent to previous findings from clinical data (5, 35, 36). Healy et al.
What causes blood vessels to calcify?
The calcium deposits in your arteries are not related to your diet or any supplements you may be taking. They occur because the cells in your blood vessels are not working as they should. They can be a sign of heart disease, or simply of getting older.
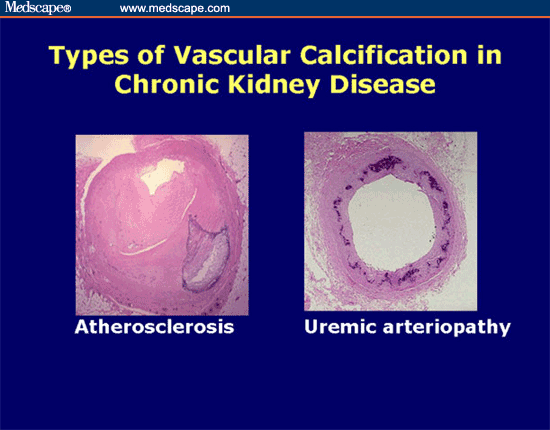
What is vascular calcification?
Vascular calcification is the pathological deposition of mineral in the vascular system. It has a variety of forms, including intimal calcification and medial calcification, but can also be found in the valves of the heart. Vascular calcification is associated with atherosclerosis, diabetes, certain heredity conditions, and kidney disease, ...
What is the result of medial calcification?
The result of medial calcification is a stiffening of the artery wall, with the associated rise in blood pressure, and a higher risk of cardiovascular mortality [1]. Valves: native and bioprosthetic valves. Vascular calcification can also lead to the dysfunction of heart valves, both native valves and bioprosthetic valves.
How long does it take for a bioprosthetic valve to calcify?
However, bioprosthetic valves are prone to calcification and may require replacement after 5–10 years. In fact, calcification and its contribution to tissue deterioration is the major mode of failure of bioprosthetic valves.
What is calcification of leaflets?
In the valves, calcification of the leaflets can change the mechanical properties of the tissue and result in stenosis. Calcification of the valves is commonly associated with aging, and is the most common pathology seen in excised native valves [3].
What is a calcimimetic?
Calcimimetics are allosteric modulators of CaR which make the CaR more sensitive to existing levels of circulating calcium, which in turn, suppress secretion of PTH. Calcimimetics have been shown to reduce vascular calcification in a variety of uremic rat models [40]. There is also evidence of efficacy in humans.
Is vascular calcification a risk factor?
Patients with vascular calcification are at higher risk for adverse cardiovascular events. Vascular calcification affects a wide variety of patients. Idiopathic infantile arterial calcification is a rare form of vascular calcification where the arteries of neonates calcify.
Does vitamin K2 cause vascular calcification?
Vitamin K was found to inhibit vascular calcification in warfarin-treated rats [43]. In humans, increased expression of under carboxylated MGP is associated with vascular calcification and increased risk of cardiovascular mortality, and supplementation with vitamin K2 was found to increase levels of carboxylated MGP in dialysis patients [44].
What is medial calcification?
Medial calcification is an extracellular event initiated by deposition of hydroxyapatite on elastin fibers. (1) The first step in this process is the formation of CaHPO4, which can be reduced by lowering phosphate concentrations. (2) Thiosulfate may inhibit this reaction by forming ion pairs with calcium ions.
Does calcitriol increase calcification?
Second, calcitriol and calcitriol analogues may increase medial calcification, either through direct actions on vascular smooth muscle or by raising circulating calcium levels. Lastly, smooth muscle-specific factors that promote and inhibit calcification are not addressed by this strategy.
Does hypercalciuria cause vascular calcification?
The hypercalciuria could be preventing vascular calcification through negative calcium balance , but this is unlikely without a long-term reduction in serum calcium or increase in parathyroid hormone. Not surprisingly, the serum anion gap increased with a drop in bicarbonate concentration and pH.
Does magnesium inhibit hydroxyapatite formation?
6 Magnesium also inhibits hydroxyapati te formation and could be an effective substitute for calcium in phosphate binders.
Is pyrophosphate safe for calcification?
A seemingly safe way to do this would be to use calcification inhibitors normally present in vascular smooth muscle, of which pyrophosphate is the most feasible. Although pyrophosphate prevents medial calcification in vitamin D-toxic rats,3 very high doses are required because of rapid hydrolysis to orthophosphate.
Does thiosulfate prevent calcification?
Thiosulfate completely prevented calcification in this model at a dose and interval comparable to those used in humans with CUA, thus providing a scientific basis for its clinical use. However, this is a model of large-artery calcification, not CUA, and the pathogenesis may not be the same.
Does PPI inhibit calcification?
Large doses of PPi have been shown to inhibit vascular calcification in vitamin D-toxic rats. (4) PP i is hydrolyzed by tissue-nonspecific alkaline phosphatase (TNAP) on the smooth muscle membrane, and this could be targeted by newly developed TNAP inhibitors.
What is vascular calcification?
Vascular calcifications are mineral deposits on the walls of your arteries and veins. These mineral deposits sometimes stick to fatty deposits, or plaques, that are already built up on the walls of a blood vessel.
What is calcification in blood vessels?
Vascular calcifications are mineral deposits on the walls of your arteries and veins. These mineral deposits sometimes stick to fatty deposits, or plaques, that are already built up on the walls of a blood vessel.
How to treat a clogged blood vessel?
Vascular Calcification Treatment and Prevention. Doctors treat plaque-clogged blood vessels in a variety of ways, including vascular surgery and medicine. Lifestyle changes — quitting smoking, eating healthier foods, and starting to exercise — can decrease the chances of plaque and calcifications forming. If you take calcium supplements, your ...
What is UPMC heart and vascular?
The UPMC Heart and Vascular Institute has long been a leader in cardiovascular care, with a rich history in clinical research and innovation. As one of the first heart transplant centers in the country and as the developer of one of the first heart-assist devices, UPMC has contributed to advancing the field of cardiovascular medicine.
What is calcification in breast?
In the body, calcification is actually part of the aging process. Calcifications accumulate in the vessels, heart, or valves as calcium travels through the bloodstream.
Where does calcification occur?
Calcifications can occur in the intimal (inside) or medial (middle layer) part of the blood vessel. Each location has different associated risks. Medial calcifications, for example, are most often associated with kidney disease, diabetes, hypertension, and advanced age.
Can vascular calcification cause stroke?
You may not always notice symptoms of vascular calcification. If vascular calcification causes arteries to harden, the heart will have to work harder to pump blood. Eventually, you might develop symptoms of peripheral artery disease (PAD) or stroke.
What supplements can help with calcification of the arteries?
Supplementation for Calcification of the Arteries. 1. Vitamin K2 Liquid. One study published in the Journal of the American Society of Hematology induced calcification of the arteries in rats by giving them warfarin (blood thinning drug) , then separated into four groups.
What causes calcification of the arteries?
Calcification of the Arteries – There are many different ways that calcification can occur: High vegetable oil intake, blood thinning medications, high fluoride intake, vitamin C deficiency, a high calcium intake without adequate magnesium, K and D, and excessive vitamin D to low vitamin K intake. With diligent diet and supplementation, you may be ...
What causes calcium to not be deposited in bones?
Lack of vitamin K2 causes calcium to fail to be deposited in bones and instead ends up in the arteries, aorta and other parts of the body. A clinical study from Rotterdam, Holland found that long term adequate vitamin K2 intake was correlated with a lower incidence of calcification of the wall of the aorta.
What is the best vitamin for calcification?
Vitamin C keeps the blood vessels strong, reducing circulating cholesterol, while also clearing the inner walls of fat deposits. Long-term vitamin C deficiency can lead to weak arteries prone to calcification. 3. Magnesium Citramate.
Does vitamin K block calcium buildup?
The group given the highest level of vitamin k not only blocked new arterial calcium buildup but also reduced existing levels of calcification by 37 percent. The researchers noted, “Our study shows that in an animal model, vitamin K can actually regress preformed calcifications. The health implications for humans are significant.”.
Does Coumadin cause arterial calcification?
Blood thinning drugs: Drugs like Coumadin are known to induce arterial calcification by inactivating a protein called matrix GLA, or MGP, a potent inhibitor of calcification. MGP requires vitamin K for activation. High Calcium Intake: Taking isolated calcium while being deficient in vitamin K, D and magnesium can cause calcium to have deleterious ...
Can calcium supplements cause heart attacks?
High Calcium Intake: Taking isolated calcium while being deficient in vitamin K, D and magnesium can cause calcium to have deleterious effects on the body. One meta-analysis linked calcium supplements to heart attacks due to taking isolated forms. 1. Fluoride: A 2012 study in the Journal of Nuclear Medicine Communications found ...
What causes calcium to be calcified?
existing heart or kidney conditions. taking certain medications that affect the way your body processes calcium, such as high blood pressure and cholesterol medications. injury.
What organs are affected by aortic calcification?
The arteries ( atherosclerosis ) heart valves (calcification of the aortic valve) other organs, such as the kidneys, bladder, and even (though rare) the liver. other soft tissues (muscles, breasts, fatty tissue) joints and tendons. the brain (cranial calcification)
What is the term for the accumulation of calcium in parts of the body?
The term “calcification” refers to the accumulation of calcium in parts of the body where it should not accumulate, causing hardening of the tissues in question. This type of calcium build-up can affect many parts of the body, including: The arteries ( atherosclerosis ) heart valves (calcification of the aortic valve) ...
Can kidney stones be removed surgically?
Calcium deposits in the joints and tendons can be removed surgically. While people with kidney stones will likely be prescribed diuretics that stimulate calcium build-up in the bones. Those prone to kidney stones may also be advised to reduce their calcium intake.
Is calcification normal in women?
Almost all adult humans have some calcification of the pineal gland in the brain, and about half of women over 50 have some calcification within their breast tissues.
Can calcification be self diagnosed?
While calcification of any kind is unlikely to produce symptoms that easily lead to self-diagnosis, anyone concerned about their health should see a orthopaedic in Delhi. The detailed description of your symptoms will allow your doctor to decide what kinds of tests should be done, leading to a diagnosis.
How to diagnose calcification?
Diagnosing calcification. Calcifications are usually found via X-rays. X-ray tests use electromagnetic radiation to take pictures of your internal organs and usually cause no discomfort. Your doctor will likely detect any calcification issues right away with X-rays. Your doctor may also order blood tests.
What causes calcification in the body?
Causes of calcification. Many factors play a role in calcification. These include: infections. calcium metabolism disorders that cause hypercalcemia (too much calcium in the blood) genetic or autoimmune disorders affecting the skeletal system and connective tissues. persistent inflammation.
What are the soft tissues that are affected by calcium buildup?
soft tissues like breasts, muscles, and fat. kidney, bladder, and gallbladder. Some calcium buildup is harmless. These deposits are believed to be the body’s response to inflammation, injury, or certain biological processes. However, some calcifications can disrupt organ function and affect blood vessels.
What happens when calcium builds up in the body?
Calcification happens when calcium builds up in body tissue, blood vessels, or organs. This buildup can harden and disrupt your body’s normal processes. Calcium is transported through the bloodstream. It’s also found in every cell. As a result, calcification can occur in almost any part of the body. According to the National Academy of Medicine. ...
What is the most common type of breast calcification?
According to the National Cancer Institute, macrocalcifications in the breasts are most common in women over 50 years old.
What medications affect calcium levels?
Some medications can affect your body’s calcium levels. Cholesterol medication, blood pressure medication, and hormone replacement therapy are common medications that affect how calcium is used in your body.
Can you get calcifications at 65?
If you’re under 65 years old and were born with a heart defect or kidney-related issues, calcifications can be more common for you than for others of your age. If you are aware of any of these conditions, ask your doctor about getting tested for calcifications. Some medications can affect your body’s calcium levels.
Overview
- Breast calcifications are small calcium deposits that develop in a woman's breast tissue. They are very common and are usually benign (noncancerous). In some instances, certain types of breast calcifications may suggest early breast cancer. Microcalcifications are small calcium deposits that look like white specks on a mammogram. Microcalcifications are usually not a result of can…
Treatment
- If you have macrocalcifications, no further testing or treatment is needed, because they are not harmful. If microcalcifications are seen on your mammogram, another mammogram may be performed to get a more detailed look at the area in question. The calcifications will be determined to be either \"benign,\" \"probably benign,\" or \"suspicious.\" ''Benign'' calcifications a…
- In diagnosing calcium crystal pathology, other pathologies such as gout and infection must be first ruled out. Tests done include joint fluid sampling, X-rays, and blood and biochemical panels. Non-steroidal anti-inflammatory drugs (NSAIDs) like ibuprofen ease the pain associated with acute attacks.Anti-gout drug colchicine may also be used to reduce the interaction between the …
Definition
- Distribution modifiers (grouped or clustered, linear, segmental, regional, diffuse) are used to describe the arrangement of the calcifications. Historically, the terms grouped or clustered were used to describe suspicious calcification. Now, these terms are neutral and may be used to describe benign or malignant processes. Grouped or clustered should be used to describe calcif…
Symptoms
- Breast calcifications do not cause symptoms, as they are too small to be felt during a routine breast exam. Usually, breast calcifications are first noticed on a mammogram.
Diagnosis
- Radiologists who interpret mammograms encounter calcifications on a daily basis (see the images below). Most of the breast calcifications encountered by radiologists are benign. Radiologists must be able to identify typically benign breast calcifications that do not require biopsy to prevent unnecessary procedures and to reduce patient anxiety. [1, 2, 3, 4, 5, 6] High-qu…
Types
- Macrocalcifications look like large white dots on a mammogram (breast X-ray) and are often dispersed randomly within the breast. Macrocalcifications are common -- they are found in approximately half of women over age 50, and one in 10 women under age 50 -- and are considered noncancerous.
- Typically, benign calcifications that do not require biopsy are skin or dermal calcifications, vascular calcifications, lucent-centered calcifications, eggshell or rim calcifications, coarse or popcornlike calcifications, large rodlike calcifications, round and punctuate calcifications, milk of calcium calcifications, suture calcifications, and dystrophic calcifications. [7, 8]
Causes
- A number of factors can cause calcification in a woman's breast, including normal aging, inflammation, and past trauma to the area. Calcium from your diet does not cause breast calcifications.
Prognosis
- ''Probably benign'' calcifications have a less than 2% risk of being cancer. In other words, more than 98% of the time \"probably benign\" calcifications are not cancer. Typically, they will be monitored every six months for at least one year. After a year of follow-up, and assuming no new changes are found, your doctor will recommend you have a routine mammogram once a year.
Cause
- Regionally distributed calcifications are most likely due to benign processes. These calcifications are scattered in a large volume of the breast and do not necessarily conform to a ductal distribution.
Categories
- There are 7 ACR BI-RADS standardized categories [10, 11] : Typically, benign calcifications will be placed in ACR BI-RADS categories 1 and 2. Sometimes, these calcifications are initially placed in ACR BI-RADS category 0 and, after additional imaging evaluation, are found to have benign features. Early in their development, calcifications (eg, vascular, dystrophic, or lucent centered c…