Why is informed consent important?
Generally speaking, obtaining informed consent means that a patient who agrees to undergo a treatment or procedure does so only after being made aware of the associated benefits, risks, and alternative treatments.
What does it mean to obtain informed consent?
Generally speaking, obtaining informed consent means that a patient who agrees to undergo a treatment or procedure does so only after being made aware of the associated benefits, risks, and alternative treatments.
What does consent to treatment mean?
Children and young people. Consent to treatment means a person must give permission before they receive any type of medical treatment, test or examination. This must be done on the basis of an explanation by a clinician. Consent from a patient is needed regardless of the procedure, whether it's a physical examination, ...
Why is consent important?
The principle of consent is an important part of medical ethics and international human rights law.
What is voluntary consent?
voluntary – the decision to either consent or not to consent to treatment must be made by the person, and must not be influenced by pressure from medical staff, friends or family. informed – the person must be given all of the information about what the treatment involves, including the benefits and risks, whether there are reasonable alternative ...
What does it mean to have the capacity to consent?
capacity – the person must be capable of giving consent, which means they understand the information given to them and can use it to make an informed decision. If an adult has the capacity to make a voluntary and informed decision to consent to or refuse a particular treatment, their decision must be respected.
Can consent be given verbally?
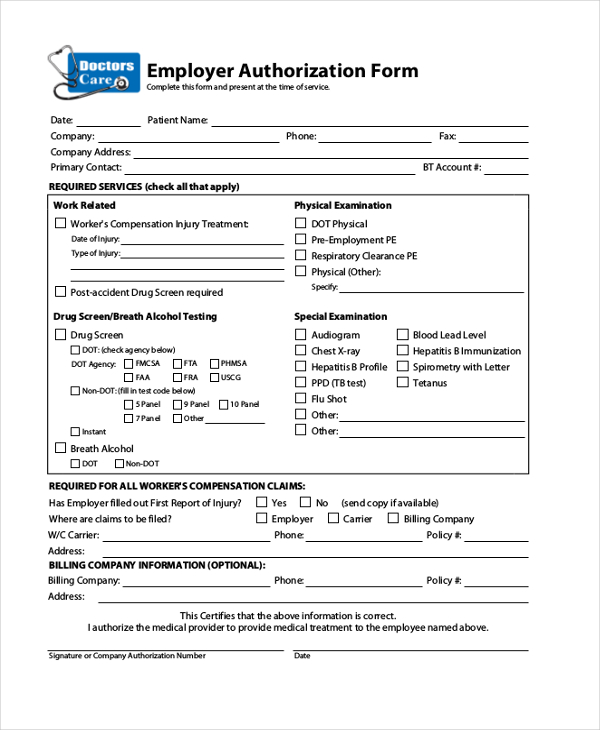
Consent can be given: verbally – for example, a person saying they're happy to have an X-ray. in writing – for example, signing a consent form for surgery. Someone could also give non-verbal consent, as long as they understand the treatment or examination about to take place – for example, holding out an arm for a blood test.
How old do you have to be to give consent to a child?
But someone with parental responsibility may need to give consent for a child up to the age of 16 to have treatment. Find out more about how the rules of consent apply to children and young people.
What happens if you refuse treatment?
This is still the case even if refusing treatment would result in their death, or the death of their unborn child. If a person does not have the capacity to make a decision about their treatment ...
Why is informed consent required in research?
It informs the participants about the trial and lets them make educated decisions about taking part in the study. The process is similar to informed consent in healthcare. In a research setting, it involves discussing the following:
Do you need informed consent for blood work?
Informed consent isn’t always required in emergencies. In an emergency, your provider may look for your closest blood relatives for consent. But if your relatives aren’t available, or if you’re in a life-threatening situation, a healthcare provider can perform the necessary life-saving procedures without consent.
What is consent form?
This form is a legal document that shows your participation in the decision and your agreement to have the procedure done.
Do you have to give consent to a teen?
In most states, if you’re younger than 18, a parent or guardian will need to give consent on your behalf. But some states allow teens who are emancipated, married, parents, or in the military to provide their own consent. You want someone else to make the decisions.
Can you give consent to someone else?
This allows someone else to give consent on your behalf if you’re unable to. You can’t give consent. Another person can make your medical decisions if you can’t provide consent. This may happen if you’re in a coma, or have a condition like advanced Alzheimer’s disease.
What does informed consent mean?
If you decide to move forward, you’ll need to give informed consent first. Informed consent means that you made a voluntary and educated decision. It also means that your healthcare provider has fully explained the medical procedure, including its risks and benefits.
What is implied consent?
Implied consent is a type of informed consent. This consent is suggested, or implied, by the patient’s actions. It isn’t explicitly stated or written down. For example, if you have a fever and see a healthcare provider, your visit implies that you want treatment.
Statistics from Altmetric.com
Decision-making is a prominent theme in this edition of the Journal of Medical Ethics. Our feature article examines the relationship between trust and informed consent. Informed consent is, of course, central to the decision-making process in medicine. In addition, several articles consider decision-making in medicine from a variety of angles.
Informed consent and trust: Eyal's argument
In our feature article, Nir Eyal attacks attempts by bioethicists including Onora O'Neill, Torbjörn Tännsjö, and Jennifer Jackson to ground the importance of informed consent in its role in safeguarding trust in medical practice ( see page 437, Editor's choice).
Responses from Tännsjö and Bok
Eyal's article is followed by commentaries from Torbjörn Tännsjö ( see page 445) and Sissela Bok ( see page 446 ). Tännsjö, who advances a version of the trust-promotion argument based on hedonistic utilitarianism, denies that the argument runs counter to commonsense views about informed consent.
Is informed consent only instrumentally valuable?
This is an enlightening and important debate, especially since lack of trust in medical research and practice can have worrying consequences, as Eyal and Bok both note.
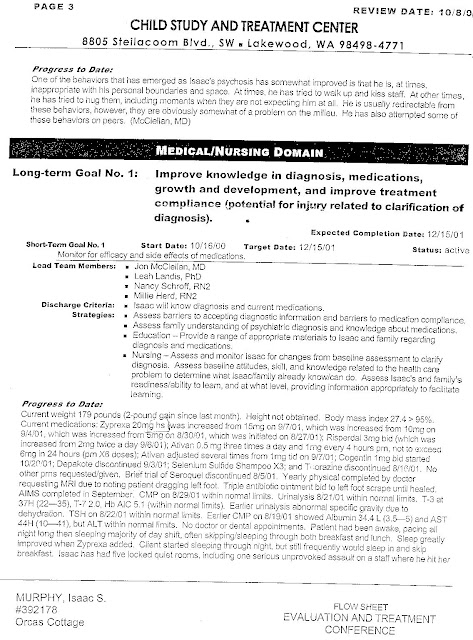
Decision-making in medicine
A further six articles in the current issue address various other aspects of decision-making. Two of these articles relate to groups of patients generally taken to lack decision-making capacity: children and psychiatric patients.
Request Permissions
If you wish to reuse any or all of this article please use the link below which will take you to the Copyright Clearance Center’s RightsLink service. You will be able to get a quick price and instant permission to reuse the content in many different ways.
Copyright information
Published by the BMJ Publishing Group Limited. For permission to use (where not already granted under a licence) please go to http://group.bmj.com/group/rights-licensing/permissions
Optimal Communication
At the beginning of the session,” complained one client, “my massage therapist started chanting. I didn’t understand what he was doing. It really freaked me out, but I didn’t say anything.”
No Surprises
It’s important to have a written explanation of the services you offer, along with a listing of their benefits and risks, if any. Give this to every new client and ensure they have time to read it and ask questions before you start working with them. As therapists, we take some aspects of bodywork for granted, but our clients may not.
The Right of Refusal
The inherent power difference in our relationships with our clients makes it easy for them to slip into a compliant, passive role. As already mentioned, clients may be reluctant to refuse, interrupt, or stop a treatment for fear of offending.
Do nurses have to give consent to patients?
They have their patients’ consent before starting treatment. Consent will only be valid if that information has been given. Nurses will be acting unlawfully, and contrary to the principles of person-centred care if they administer care without a patient’s consent.
What is person-centred care?
For the purpose of this article, person-centred care is defined as the “ approach to care that places the person at the centre of their own care.
What is the duty of a nurse?
Nurses have a legal duty to ensure they obtain informed consent from their patients before carrying out any intervention or treatment. This is one of the requirements of the Nursing and Midwifery Council’s Code, which sets out a mandatory framework of standards for practice. Nurses and midwives will all be aware of that requirement ...
What is the nursing code?
This means nurses must “get properly informed consent and document it before carrying out any action”.
Is ignorance a defence?
There is a legal principle that ignorance is not a defence: if a law is not known or not understood, this does not remove any liability that comes with it. To recognise and uphold their patients’ rights, nurses must not only be aware of the standards set out in the Code, but also understand their legal basis.
What is the role of nurses in healthcare?
Nurses must provide patients with the information they need to make an informed decision about their care. If the necessary information to make an informed decision is not given, consent may not be valid and nurses may be acting unlawfully if they proceed with treatment.
What is the NMC code?
The NMC Code: key legal principles. The Nursing and Midwifery Council’s Code says that nurses must not only “act in the best interests of people at all times”, but also balance this with “the requirement to respect a person’s right to accept or refuse treatment”. This means nurses must “get properly informed consent and document it ...
Types of Consent
Informed Consent
- To be valid, consent must be freely and voluntarily given by a patient with capacity who has been given all the information he or she needs to reach a decision. Patients should not be subjected to undue pressure or influenceby medical staff or their family or friends.
What Is Capacity?
- Capacity is defined in the Mental Capacity Act 2005, section 3 (1). A person has capacity to make a decision for themselves if they can: 1. understand the information relevant to the decision, 2. retain that information, 3. use or weigh that information as part of the process of making the decision, and 4. communicate their decision (whether by talking, using sign language or any oth…
Let's Get Technical...
- Consent represents the ethical and legal expression of a person's right to have their autonomy and self-determination respected.
- It may well be unlawful for doctors to treat patients in the absence of consent or other authority, and those doing so could commit both the crime of battery and the tort of trespass to the person1.
- Consent represents the ethical and legal expression of a person's right to have their autonomy and self-determination respected.
- It may well be unlawful for doctors to treat patients in the absence of consent or other authority, and those doing so could commit both the crime of battery and the tort of trespass to the person1.
- A doctor may treat without consent in a patient’s best interests as a matter of necessity in an emergency, where the patient lacks capacity. However, if the patient has capacity it is no defence to...