An antacid may make the pain from a peptic ulcer go away temporarily, yet it will not kill H. pylori. If you receive treatment for an H. pylori-induced peptic ulcer, check with your doctor before taking antacids. Some of the antibiotics may not work as well if you take them with an antacid.
Do antacids kill Helicobacter pylori?
Antacids An antacid may make the pain from a peptic ulcer go away temporarily, yet it will not kill H. pylori. If you receive treatment for an H. pylori-induced peptic ulcer, check with your doctor before taking antacids. Some of the antibiotics may not work as well if you take them with an antacid.
What are H pylori eradication agents?
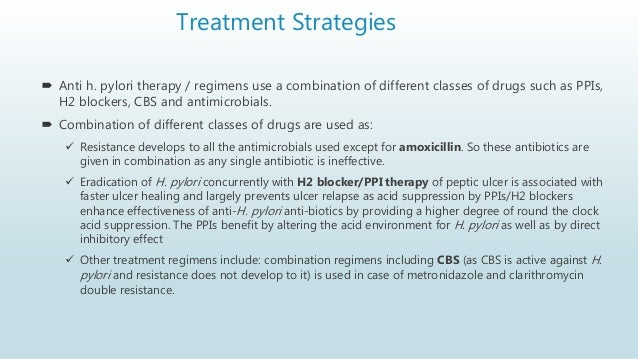
H. pylori eradication agents. What are H. pylori eradication agents? Agents used in treatment of Helicobacter Pylori are medicines used for stomach acid inhibition, combined with antibacterial agents. Treatment is for one week with a proton pump inhibitor or an antacid (or antisecretory agents), and two appropriate antibacterial agents.
How do medications treat Helicobacter pylori ulcers?
If you have an H. pylori infection, a doctor will treat your NSAID-induced peptic ulcer with PPIs or histamine receptor blockers and other medicines, such as antibiotics, bismuth subsalicylates, or antacids.
How do PPIs treat H pylori infection?
PPIs reduce stomach acid and protect the lining of your stomach and duodenum. While PPIs can’t kill H. pylori, they do help fight the H. pylori infection. Histamine receptor blockers work by blocking histamine, a chemical in your body that signals your stomach to produce acid. Histamine receptor blockers include
Do antacids help with H. pylori?
The recommended primary therapy for H pylori infection is proton pump inhibitor (PPI)–based triple therapy. Antacids or a GI cocktail (typically an antacid with an anesthetic such as viscous lidocaine and/or an antispasmodic) may be used as symptomatic therapy in the ED.
Why PPI are given in H. pylori treatment?
The rationale of PPI-based triple therapy has been established by many clinical trials and a large body of experimental evidence. PPIs have a piv- otal effect in the eradication of Helicobacter pylori infection, both indirect effects and direct effects. PPIs have a weak antibacterial effect against H.
What is the best antacid for H. pylori?
pylori infection. In patients with acute GORD with oesophagitis, omeprazole is at least as effective as lansoprazole or pantoprazole in promoting healing, and superior to ranitidine, cimetidine or cisapride in oesophagitis healing and symptom relief.
Why combined drugs are used in H. pylori infection?
How It Works. The right antibiotics combinations usually kill Helicobacter pylori (H. pylori) bacteria that are the cause of many peptic ulcers. At least two antibiotics are used, because combination treatment works better and is less likely to fail because of resistance to the antibiotics.
How do proton pump inhibitors affect H. pylori?
Background: Proton pump inhibitors are known to decrease the activity of Helicobacter pylori organisms within the stomach and to shift their distribution proximally. This effect may reduce the sensitivity of histological examination and rapid urease testing for H. pylori on biopsies taken from recommended sites.
What do PPI inhibitors do?
Proton pump inhibitors are used to: Relieve symptoms of acid reflux, or gastroesophageal reflux disease (GERD). This is a condition in which food or liquid moves up from the stomach to the esophagus (the tube from the mouth to the stomach).
What medication is used to treat H. pylori?
The most important antibiotics in H. pylori treatment are clarithromycin, metronidazole, and amoxicillin. Figure 1 illustrates recently reported clarithromycin and metronidazole resistance rates worldwide. Resistance to these antibiotics is thought to be the main cause of eradication failure[27-29].
What's the latest treatment for H. pylori?
Bismuth-containing quadruple therapy has been confirmed as an effective regimen for eradicating H. pylori, especially in strains with antibiotic resistance. High-dose proton-pump inhibitor-amoxicillin dual therapy could decrease the use of unnecessary antibiotics, which is a promising alternative approach.
Does H. pylori increase stomach acid?
Helicobacter pylori infection increases gastric acid secretion in patients with duodenal ulcers but diminishes acid output in patients with gastric cancer and their relatives.
What is the best antacid for stomach ulcer?
Omeprazole, pantoprazole and lansoprazole are the PPIs most commonly used to treat stomach ulcers.
Can omeprazole and azithromycin be taken together?
Interactions between your drugs No interactions were found between azithromycin and omeprazole. However, this does not necessarily mean no interactions exist. Always consult your healthcare provider.
Can omeprazole and metronidazole be taken at the same time?
Bismuth subcitrate, metronidazole, and tetracycline combination is used together with omeprazole to treat a stomach infection caused by the H. pylori bacteria and duodenal ulcer. This bacteria can cause stomach ulcers if it is not treated. This medicine should not be used for any other infection.
What are H. pylori eradication agents?
Agents used in treatment of Helicobacter Pylori are medicines used for stomach acid inhibition, combined with antibacterial agents. Treatment is for one week with a proton pump inhibitor or an antacid (or antisecretory agents), and two appropriate antibacterial agents. This one week triple therapy does give a good eradication rate.
Further information
Always consult your healthcare provider to ensure the information displayed on this page applies to your personal circumstances.
What is the best medicine for acid reflux?
Millions of people take over the counter antacids, or more potent prescription acid blocking medications such as proton pump inhibitors to deal with acid reflux and gastro-esophageal reflux disease.
How long can you take acid blockers?
As you can see, the risks of long-term acid blocker use are pretty big and in my opinion, it’s insane for the medical system to recommend these meds are used for more than 60-90 days without good reason, or without monitoring nutrient levels and gastrointestinal health.
What are the symptoms of inadequate stomach acid?
Common symptoms of inadequate stomach acid include heartburn, bloating and other digestive discomfort, which is often result from SIBO, Candida, parasites and even serious infections like C. difficile.
Does Candida cause nutrient depletion?
Not only does this lead to nutrient depletion over time, but it also makes it much easier for microbes such as H. pylori, Candida and SIBO to overgrow and cause problems.
Can antacids cause bloating?
The net result can be bloating, gas, loose stools, diarrhea, fatigue, depression, allergies and other unpleasant symptoms. If you are taking antacids, H2 blockers or PPIs on an ongoing basis, perhaps it’s worth considering the info below because your long term health may be at stake.
Can acid blockers cause dementia?
Long-term acid blocker use may also contribute in some people to the development of osteoporosis, heart disease, kidney disease and dementia.
Can acid blocking medications cause nutrient depletion?
There are clear problems with acid blocking medications potentially causing nutrient depletion, not so much with short term use, but certainly in the long term. My advice is to discuss with your doctor the possibility of gradually reducing the dose and coming off your long term acid blocking medications.
What antibiotics are used to treat H. pylori?
The most important antibiotics in H. pyloritreatment are clarithromycin, metronidazole, and amoxicillin. Figure Figure11illustrates recently reported clarithromycin and metronidazole resistance rates worldwide. Resistance to these antibiotics is thought to be the main cause of eradication failure[27-29]. Antibiotic resistance is discovered by bacterial culture-based techniques (E-test, modified disk diffusion, agar dilution method, and breakpoint susceptibility test) and molecular methods [polymerase chain reaction (PCR), real-time PCR, allele-specific PCR, sequencing, and fluorescent in situhybridization][30]. Although these methods are useful for examining antibiotic resistance, their implementation at the early stages of H. pyloriremains impractical due to the time required to obtain results and the high cost of the tests.
What is the sole class of antibiotics for treatment of H. pylorithat?
Fluoroquinolones are the sole class of antibiotics for treatment of H. pylorithat directly inhibit bacterial DNA synthesis. Resistance to fluoroquinolones occurs primarily by mutation in the genes for topoisomerase IV and gyrase[59].
What is the first line of treatment for H pylori infection?
The first-line regimen for the eradication of H. pyloriinfection consists of STT using a PPI, amoxicillin and clarithromycin and was first introduced by Dr. Bazzoli. In studies conducted during the 1990s, STT yielded > 80% treatment success with reports of > 90% possible[66,67]. However, the increased prevalence of clarithromycin resistance has accounted for the diminished efficacy of STT. Table Table11shows eradication rates from recent studies using STT. Generally, STT is not recommended as a first-line regimen when the clarithromycin resistance rate is > 15%-20%, and other therapies such as quadruple therapy or sequential therapy are suggested[25]. Thus, a steady increase in H. pyloriresistance to amoxicillin and metronidazole has also resulted in reduced treatment success of STT[27,68,69]. The ideal outcome of H. pylorieradication is > 80% by intention to treat (ITT) analysis and > 90% by per protocol (PP) analysis. According to a recent study, the eradication rate was unacceptably low for treatment success, with only 18% exceeding 85% and approximately 60% failing to attain 80% eradication by ITT analysis[20]. Over the past 20 years, the efficacy of STT has decreased, with eradication rates < 80% by ITT analysis[41]. According to the present formula by Dr. Graham[70], if clarithromycin resistance rate of 20%, the outcome of clarithromycin containing triple therapy is reduced to 77.2% by PP analysis. Already in some countries the eradication rates have been reported to be < 50% and if this trend continues for another 20 years, the efficacy of STT will be negligible.
What is the best treatment for Helicobacter pylori?
pylorieradication is underscored by its designation as a group I carcinogen. The standard triple therapy consists of a proton pump inhibitor, amoxicillin and clarithromycin, although many other regimens are used, including quadruple, sequential and concomitant therapy regimens supplemented with metronidazole, clarithromycin and levofloxacin. Despite these efforts, current therapeutic regimens lack efficacy in eradication due to antibiotic resistance, drug compliance and antibiotic degradation by the acidic stomach environment. Antibiotic resistance to clarithromycin and metronidazole is particularly problematic and several approaches have been proposed to overcome this issue, such as complementary probiotic therapy with Lactobacillus. Other studies have identified novel molecules with an anti-H. pylorieffect, as well as tailored therapy and nanotechnology as viable alternative eradication strategies. This review discusses current antibiotic therapy for H. pyloriinfections, limitations of this type of therapy and predicts the availability of newly developed therapies for H. pylorieradication.
What is the resistance to clarithromycin?
Clarithromycin is a macrolide antibiotic that inhibits protein synthesis by binding to and slowing the actions of the bacterial ribosome[30] . Clarithromycin resistance is due to three point mutations at A2142C, A2142G, and A2143G in the 23s rRNAgene[31]. In particular, the A2143G mutation has been related to a very low eradication rate[32]. In contrast, the A2143G mutation occurs in only 23% of resistant strains in Eastern countries[31]. This suggests that clarithromycin point mutations may be geographically distinct between Eastern and Western countries and new point mutations have appeared in South America[33]. Clarithromycin resistance is also different depending on the area. In Brazil, stomach biopsy specimens positive for H. pyloriwere analyzed by PCR to detect the point mutation associated with clarithromycin resistance[34]. The results uncovered primary clarithromycin resistance in 16.5% patients. Recently, the clarithromycin resistance rate in South Korea was reported to range from 17.2% to 23.7%[35]. In a study published in Japan, the clarithromycin resistance rate in 2002 was 18.9%; however, the clarithromycin resistance rate in 2006 increased to 27.2%[36]. Even with third-line eradication therapy, clarithromycin resistance rates in Japan were reported as 86.4%[37]. Several studies in China have reported increased resistance rates Shanghai[38], 21.5% resistance in the southeast coastal region[39], and a relatively high rate of 33% in Vietnam, which is near Southeast China[40]. In Western Asia, resistance to clarithromycin has been reported to be > 10% in Iran and > 20% in Turkey[13]. In one study, clarithromycin resistance was reported in 47.5% of patients with dyspepsia in Turkey[41]. In sharp contrast to other Asian countries, no resistance to clarithromycin has been reported in Malaysia[42] and the prevalence of resistance to clarithromycin in Gambia and Senegal also remains very low[43,44]. Resistance to clarithromycin has also risen by > 20% in Southern Europe, although in Northern Europe the resistance rate is less than 10%[45] compared to 1.5% in a random adult Swedish population[46] and 7.5% in central Germany[47]. During the last 15 years, a twofold increase in clarithromycin resistance was reported in Italy[48] and in Spain, where the mean clarithromycin resistance rate was 18.3% in 1709 patients[49], and 34.7% in Portuguese children[50]. In contrast to the general trend, the rate of H. pyloristrains resistant to clarithromycin decreased from 34% to 22% during 6 years in Southern Poland[51]. Despite these variations, the overall frequency of clarithromycin resistance has risen from 10.2% to 21.3% worldwide, and A2143G is the most frequently reported point mutation. Present European guidelines recommend 7 d of STT in regions in which the rate of clarithromycin resistance is < 20%, and 14 d in regions with clarithromycin resistance rates of > 20%[25,45].
Is amoxicillin a beta-lactam?
Amoxicillin is a beta-lactam antibiotic that was first used for H. pyloritherapy[25]. Unlike clarithromycin and metronidazole, amoxicillin resistance rates are low worldwide[30]: 0% or < 1% in Europe[30]. However, other studies revealed high amoxicillin resistance rates in Iran, Japan, and Cameroon[37,45,54].
Is H pylori a carcinogen?
The World Health Organization has classified H. pylorias a group I carcinogen with a risk of stomach cancer[7,8]. H. pylori-related stomach cancer represents 5.5% of all cancers worldwide and 25% of all infection-associated malignancies.
