Why do dentists prescribe antibiotics?
Why Your Dentist Might Recommend Amoxicillin For Abscessed Tooth
- Types of Dental Infections. According to the American Association of Endodontists, you may have an abscessed tooth if you experience pain when chewing, an aching jaw or swollen gums.
- Treatment of Dental Abscesses. ...
- Antibiotics for Dental Infections. ...
Why take amoxicillin before dental work?
The reason why a dental patient may need to take an antibiotic before their treatment is primarily due to the risk of oral biofilm entering the blood supply through the mouth, as it’s being disrupted by the dentist or hygienist. For medically compromised individuals, there is a risk of the biofilm transferring itself into the blood vessels, heart, or elsewhere in the body.
How much Clindamycin should I take before dental work?
- Rheumatoid arthritis, lupus, and other autoimmune disorders for which infection can trigger sometimes severe inflammation of the joints
- People with hemophilia or insulin-dependent diabetes who are at increased risk of blood-borne infections
- Immune compromised individuals. ...
- Persons who have had a past infection of a joint implant
Do I need antibiotics before a dental procedure?
The reason why a dental patient may need to take an antibiotic before their treatment is primarily due to the risk of oral biofilm entering the blood supply through the mouth, as it’s being disrupted by the dentist or hygienist. For medically compromised individuals, there is a risk of the biofilm transferring itself into the blood vessels ...

Do you need antibiotics for dental procedure?
Antibiotics treat certain oral infections caused by bacteria, like an abscessed tooth. In some cases, antibiotics are prescribed before dental procedures as a precaution to prevent infection. This is called prophylaxis and should be used only when necessary based on clinical guidelines.
Why do dentist put you on antibiotics?
The Usual Occasions for Antibiotics Antibiotics may be used in cases of an abscess or periodontal disease (gum infection). It's usually a necessary part of such procedures as tooth extraction, root canal therapy or deep cleaning of the gums. In other cases, antibiotics may be prescribed to prevent an infection.
Do dentists use antibiotics?
Antibiotics are generally used in dental procedures to treat odontogenic infections, nonodontogenic infections, local infection, focal infection, and prophylaxis.
Who prescribes antibiotics for teeth?
To treat a tooth infection, a dentist will typically do one of the following: Open up and drain the abscess, perform a root canal, or pull the affected tooth. A doctor can also prescribe antibiotics to kill the infection before the tooth is dealt with by the dentist, to prevent the bacteria from spreading.
Who needs antibiotics prior to dental work?
Today, the AHA only recommends antibiotics before dental procedures for patients with the highest risk of infection, those who have: A prosthetic heart valve or who have had a heart valve repaired with prosthetic material. A history of endocarditis. A heart transplant with abnormal heart valve function.
When do dentists prescribe antibiotics?
If a patient's condition progresses to systemic involvement, showing signs of fever or malaise, then dentists should prescribe antibiotics.
Do you need antibiotics for root canal?
Antibiotics are not absolutely necessary after a root canal. After a root canal, you need very little time to recover, and post-operative care is the best way for fast healing. However, a dentist may recommend antibiotics before root canal to improve the chances of a successful outcome.
What is the strongest antibiotic for dental infection?
Amoxicillin is usually the first choice for tooth infection treatment. If your tooth infection is more serious, your dentist may prescribe a combination of amoxicillin and another drug called Clavulanate. This combination is stronger and more effective against tooth infections.
Do I need antibiotics before a root canal?
Giving a patient antibiotics before a dental treatment is known as antibiotic prophylaxis. For patients with certain conditions, this is recommended before undergoing dental treatment that poses a risk of bacteria entering the bloodstream.
Can a doctor give antibiotics for tooth infection?
Antibiotics are not routinely prescribed for dental abscesses, but may be used if the infection spreads or is particularly severe.
When do you need antibiotics for toothache?
When Does a Toothache Require Antibiotics? When the dental infection is severe or impacts the gum around an erupting tooth, your dentist may recommend antibiotics. For instance, pericoronitis is an infection in the gum tissue that can develop around impacted wisdom teeth, as Merck Manuals explains.
Can dentist prescribe antibiotics for gum infection?
Your dentist will likely prescribe an antibiotic to help kill the bacteria causing your tooth infection. Read on to learn more about the types of antibiotics used to treat tooth infections and over-the-counter options for pain relief.
What antibiotics treat tooth infections?
The most common antibiotics for infected tooth treatment are those in the penicillin class, including penicillin and amoxicillin. Some people are a...
How long does it take for doxycycline to work for tooth infection?
You may begin to notice relief from doxycycline for dental infection within a day or two. However, you must continue to take the amount your dentis...
What antibiotics are used for a tooth infection?
Common antibiotics used for tooth infection treatment include penicillin, amoxicillin, metronidazole, Clindamycin, and azithromycin. Now let's take...
What is the best antibiotic for tooth infection treatment?
In many cases, antibiotics from the penicillin class, including penicillin and amoxicillin, are the best antibiotics for tooth infection. But that...
How long does it take for antibiotics to work for a tooth infection?
You can start feeling the effects of antibiotics on a tooth infection in as little as a day. But just because your pain has gone away doesn't mean...
What is the best antibiotic for gum infection?
An untreated gum infection (periodontitis) can lead to problems such as adult tooth loss, soft tissue damage, and a weakening of your jaw bone. It...
Who needs antibiotics before dental work?
Most patients don't require antibiotics before dental work. Immune systems are more than capable of handling these bacteria, but there are some peo...
How much Clindamycin should I take for a tooth infection?
You should take the dosage prescribed by your dentist. If you are prescribed a typical dose for Clindamycin—300 mg for tooth infection—this is norm...
How long does it take for amoxicillin to work for a tooth infection?
If you take the amoxicillin antibiotic for tooth infection, you may begin to feel better in just one to two days. However, that doesn't mean that y...
What is the best antibiotic for abscess tooth treatment?
The best antibiotic for dental abscess is the one your dentist prescribes for you. It's also likely one from the penicillin class, including penici...
What is the best antibiotic for a tooth infection?
There is no one antibiotic that is best for treating a tooth infection. The type of antibiotic a dentist recommends will vary depending on the bact...
How long does it take for a tooth infection to go away with antibiotics?
After a person begins to take antibiotics, it should take 2-3 days for the infection to begin to clear. A person should finish the entire course of...
Will antibiotics stop tooth pain?
Research shows that when a person begins to take antibiotics for a tooth infection, they begin to feel some pain relief within 24 hours. After 24 h...
What is the best antibiotic for tooth infection?
Penicillin-type drugs are common forms of antibiotics for tooth infections. This includes penicillin and amoxicillin. Some dentists may also recommend amoxicillin with clavulanic acid, as the combination may help eliminate more stubborn bacteria.
How to treat an infection in a tooth?
Antibiotics may help clear the active infection, but the tooth will need work to keep the infection at bay. This typically means undergo ing one or more procedure s in the area, such as : draining the abscess . filling in any cavities.
Why is it important to treat tooth decay early?
Treating tooth decay early is important to prevent complications such as tooth infections. Anyone who experiences a tooth infection should see a dentist right away to prevent the infection from spreading. One of the first things a dentist will likely recommend is an antibiotic to kill the infection. Some antibiotics work better than others ...
What is the first thing a dentist will recommend?
One of the first things a dentist will likely recommend is an antibiotic to kill the infection. Some antibiotics work better than others for tooth infections, and there may also be some over-the-counter (OTC) pain medications to help with the symptoms.
How common is tooth decay?
Without treatment, the infection may spread to other areas of the jaw or even the brain. Dental decay and cavities are very common. As one article notes, up to 91% of adults. Trusted Source. ages 20–64 have cavities. Also, around 27% of people in the same age group have untreated tooth decay.
How long does it take for a tooth infection to go away?
As the International Dental Journal. Trusted Source. study notes, the majority of acute infections resolve in 3–7 days.
Why does my tooth get infected?
Summary. A tooth infection, or an abscessed tooth, generally occurs as a result of tooth decay and poor oral hygiene. However, it can also develop due to previous dental work or traumatic injury. When an infection occurs, it causes a pocket of pus to form in the mouth as a result of an overgrowth of bacteria.
Key Points
The guideline recommends against using antibiotics for most pulpal and periapical conditions and instead recommends only the use of dental treatment and, if needed, over-the-counter pain relievers such as acetaminophen and ibuprofen.
Get Your Personalized Clinical Recommendation
To find the guideline recommendation that's best for your patient, select the appropriate parameters below and press the "Next" button.
Disclaimer
Content on this page is for informational purposes only. It is based on the “ Evidence-Based Clinical Practice Guideline on Antibiotic Use for the Urgent Management of Pulpal- and Periapical-Related Dental Pain and Intraoral Swelling ,” published in the November 2019 issue of the Journal of the American Dental Association.
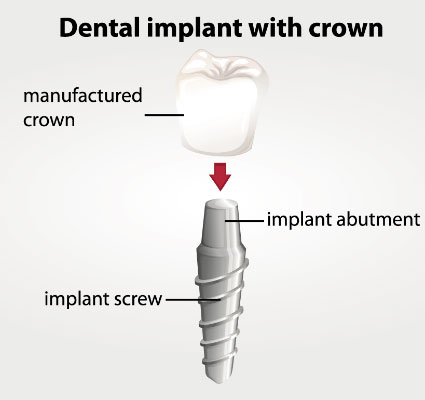
How Implant Infection Occurs
The most common route of a bacterial infection into the body is through broken skin. While normal tissue can typically defend itself against the invading bacteria, the inorganic materials of a prosthesis (artificial body part) cannot. It is there that an infection can seed and cause damage to surrounding bone and tissue.
Current Dental Recommendations
There is often confusion (and not only among patients but healthcare providers, as well) as to who should receive antibiotics before dental work. In the past, antibiotics were commonly administered for all dental procedures for the first two years following implant surgery.
Special Circumstances
This is not to suggest that antibiotics should be avoided or that there aren’t circumstances for which antibiotics may be appropriate. This includes major extractions (the pulling of teeth).
Recommended Antibiotics
When antibiotics are recommended, healthcare providers will typically prescribe oral amoxicillin (a form of penicillin) to be taken one hour before the dental work.
