
A mAb treatment may help people who:
- Are at high risk of getting more serious symptoms and
- Have a positive COVID-19 test with symptoms for 7 days or less ( bebtelovimab or sotrovimab) or
- Have been in close contact with someone who has recently tested positive
- Are high risk** for developing severe COVID-19 AND.
- Have a positive COVID-19 test and have not yet been admitted to the hospital AND.
- Are 12 years of age or older (and at least 88 pounds)
What are the dangers of monoclonal antibodies?
Jan 06, 2022 · Who is eligible for monoclonal antibody therapy? Given that COVID-19 vaccination provides strong protection against severe disease and need for hospitalization, monoclonal antibody therapy is an option for certain high-risk patients with COVID-19. THE FDA expanded EUA of two monoclonal antibody treatments to include patients as young as newborns. Criteria for …
How effective is the monoclonal treatment?
Dec 30, 2021 · For starters, a monoclonal antibody cocktail can be given for the treatment of mild-to-moderate Covid-19 in adults and children above 12 years who are at high risk of developing severe COVID-19 infection and/or hospitalisation. It is approved at a combined dose of 1200 mg (600 mg of each drug) administered by intravenous infusion or subcutaneous route.
When to start monoclonal antibodies?
Feb 01, 2022 · Treatment with anti-SARS-CoV-2 mAbs should be considered for patients with mild to moderate COVID-19 who are hospitalized for a reason other than COVID-19 if they otherwise meet the EUA criteria for outpatient treatment.
How safe is monoclonal antibodies?
Dec 21, 2021 · When do I need to get the treatment in order for it to work? The monoclonal antibody treatments are meant for mild to moderate COVID cases in adults and children over 12 to prevent the progression...
What is a monoclonal antibody for COVID-19?
Monoclonal antibodies are laboratory-produced molecules that act as substitute antibodies that can restore, enhance or mimic the immune system's attack on cells. Monoclonal antibodies for COVID-19 may block the virus that causes COVID-19 from attaching to human cells, making it more difficult for the virus to reproduce and cause harm. Monoclonal antibodies may also neutralize a virus.Mar 31, 2022
Can I get the COVID-19 vaccine if I was treated with monoclonal antibodies or convalescent plasma?
If you were treated for COVID-19 symptoms with monoclonal antibodies or convalescent plasma, you should wait 90 days before getting a COVID-19 vaccine.
Who is at greatest risk of infection from COVID-19?
Currently, those at greatest risk of infection are persons who have had prolonged, unprotected close contact (i.e., within 6 feet for 15 minutes or longer) with a patient with confirmed SARS-CoV-2 infection, regardless of whether the patient has symptoms.
Which groups of people are at increased risks of severe illness from COVID-19?
Among adults, the risk for severe illness from COVID-19 increases with age, with older adults at highest risk. Severe illness means that the person with COVID-19 may require hospitalization, intensive care, or a ventilator to help them breathe, or they may even die. People of any age with certain underlying medical conditions are also at increased risk for severe illness from SARS-CoV-2 infection.
Should you still get the COVID-19 vaccine if you were treated with monoclonal antibodies?
If you were treated for COVID-19 with monoclonal antibodies or convalescent plasma, there is no need to delay getting a COVID-19 vaccine.Feb 17, 2022
Do I need the COVID-19 vaccine if I still have antibodies?
Yes, the COVID-19 vaccines are recommended, even if you had COVID-19.Nov 23, 2021
Are people of a particular age vulnerable to coronavirus disease?
People of all ages can be infected by the COVID-19 virus.Older people and younger people can be infected by the COVID-19 virus. Older people, and people with pre-existing medical conditions such as asthma, diabetes, and heart disease appear to be more vulnerable to becoming severely ill with the virus.
Does age increase the risk for serious illness from COVID-19?
Your chances of getting seriously sick with COVID-19 go up with your age. Someone who's in their 50s is at higher risk than someone in their 40s, and so on. The highest risk is in people 85 and older.Aug 11, 2021
Are obese adults at greater risk of severe illness from COVID-19?
• Having obesity increases the risk of severe illness from COVID-19. People who are overweight may also be at increased risk.• Having obesity may triple the risk of hospitalization due to a COVID-19 infection.
Does having a weakened immune system increase your risk of severe COVID-19?
Being immunocompromised can make you more likely to get very sick from COVID-19. Many conditions and treatments can cause a person to be immunocompromised or have a weakened immune system. For example, some people inherit problems with their immune system. One example is called Primary immunodeficiency.
What groups of people may experience stigma during the COVID-19 pandemic?
See full answerSome groups of people who may experience stigma during the COVID-19 pandemic include:• Certain racial and ethnic minority groups, including Asian Americans, Pacific Islanders, and black or African Americans;• People who tested positive for COVID-19, have recovered from being sick with COVID-19, or were released from COVID-19 quarantine;• Emergency responders or healthcare providers;• Other frontline workers, such as grocery store clerks, delivery drivers, or farm and food processing plant workers;• People who have disabilities or developmental or behavioral disorders who may have difficulty following recommendations;• People who have underlying health conditions that cause a cough;• People living in congregate (group) settings, such as people experiencing homelessness.
Can I still have sex during the coronavirus pandemic?
If both of you are healthy and feeling well, are practicing social distancing and have had no known exposure to anyone with COVID-19, touching, hugging, kissing, and sex are more likely to be safe.Apr 15, 2020
What is the purpose of monoclonal antibody therapy?
The goal of this therapy is to help prevent hospitalizations, reduce viral loads and lessen symptom severity.
What are monoclonal antibodies?
However, monoclonal antibodies are mass-produced in a laboratory and are designed to recognize a specific component of this virus — the spike protein on its outer shell .
What antibodies interfere with the virus?
By targeting the spike protein, these specific antibodies interfere with the virus' ability to attach and gain entry into human cells. The two monoclonal antibody therapies currently available are the bamlanivimab and a combination of the casirivimab and imdevimab.
How long should you wait to get a second shot?
If you already received the first dose of vaccine before monoclonal antibody therapy, current CDC guidelines recommend you wait 90 days before receiving the second dose. Categories: Tips to Live By. Tags: Coronavirus, Infectious Disease.
What are the high risk people?
Those who are at high risk include people who: Are 65 years of age or older. Are at least 55 years of age and have heart disease, hypertension or a chronic respiratory disease such as COPD. Have a BMI above 35. Have chronic kidney disease.
What is the purpose of monoclonal antibodies?
Monoclonal antibodies targeting the S protein have the potential to prevent SARS-CoV-2 infection and to alleviate symptoms and limit progression to severe disease in patients with mild to moderate COVID-19, particularly in those who have not yet developed an endogenous antibody response. 3.
What antibody targets the RBD of the S protein?
Bamlanivimab (also known as LY-CoV555 and LY3819253) is a neutralizing monoclonal antibody that targets the RBD of the S protein of SARS-CoV-2. Etesevimab (also known as LY-CoV016 and LY3832479) is another neutralizing monoclonal antibody that binds to a different but overlapping epitope in the RBD of the SARS-CoV-2 S protein. Casirivimab (previously REGN10933) and imdevimab (previously REGN10987) are recombinant human monoclonal antibodies that bind to nonoverlapping epitopes of the S protein RBD of SARS-CoV-2.
What are the four major structural proteins in the SARS genome?
The SARS-CoV-2 genome encodes four major structural proteins: spike (S), envelope (E), membrane (M), and nucleocapsid (N), as well as nonstructural and accessory proteins. The S protein is further divided into two subunits, S1 and S2, that mediate host cell attachment and invasion. Through its receptor-binding domain (RBD), ...
What are the adverse events of bamlanivimab?
In the Phase 2 Blocking Viral Attachment and Cell Entry with SARS-CoV-2 Neutralizing Antibodies (BLAZE-1) trial, the most common adverse events associated with bamlanivimab were nausea, diarrhea, dizziness, headache, pruritis, and vomiting. The safety profile of bamlanivimab at all three doses was reportedly like that of the placebo.
What is Casirivimab plus imdevimab?
Casirivimab plus imdevimab: These are recombinant human monoclonal antibodies that bind to nonoverlapping epitopes of the spike protein RBD of SARS-CoV-2. Sotrovimab: This monoclonal antibody was originally identified in 2003 from a SARS-CoV survivor.
Is bamlanivimab still available in the US?
Because of an increasing number of reports of SARS-CoV-2 variants that are resistant to bamlanivimab alone, FDA has recently revoked the EUA for bamlanivimab, and the product will no longer be distributed in the United States. 4.
WHAT IS A MONOCLONAL ANTIBODY?
Your body naturally makes antibodies to fight infection. However, your body may not have antibodies designed to recognize a novel (or new) virus like SARS-CoV-2, the virus that causes COVID-19.
How Can I Get Monoclonal Antibodies?
To receive a mAb you should be referred for treatment by your healthcare professional and directed to available infusion locations. If you do not have a healthcare provider, call the Combat COVID Monoclonal Antibodies Call Center at 1-877-332-6585 to find out who to talk with about your symptoms and treatment.
WHAT IF I DO NOT QUALIFY FOR MONOCLONAL ANTIBODY TREATMENT?
Your healthcare professional may decide you do not qualify for mAb treatment. There could be several reasons for this. You may not meet all eligibility criteria or you may have an underlying health condition that disqualifies you for mAb treatment.
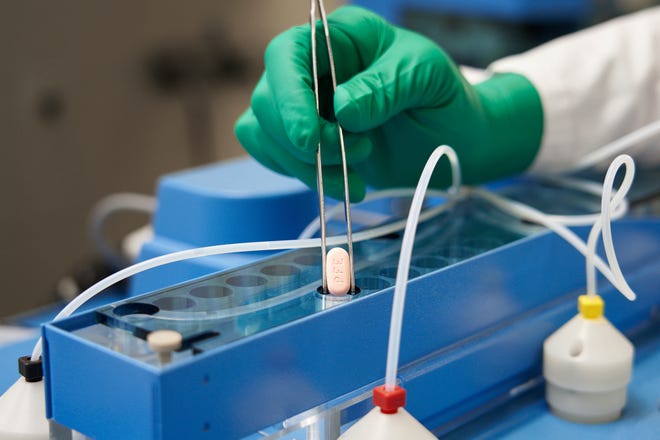
WHAT CAN I EXPECT FROM TREATMENT (INFUSION)?
The mAb treatment is usually offered at an infusion center because the treatment is given through an intravenous (IV) infusion or shots. Depending on the mAb treatment you receive, the whole process takes about 1-3 hours, depending on the treatment..
CAN MONOCLONAL ANTIBODY TREATMENT MAKE ME SICK?
Antibody treatments do not contain any live SARS-CoV-2, so there is no risk you will get COVID-19 from mAb treatment. However, the antibody treatment may have side effects:
What are monoclonal antibodies?
Antibodies are naturally produced by your body to fight off infections. When your body is introduced to a new virus such as COVID-19, it does not have the antibodies to fight it off. That is where monoclonal antibodies come in. Monoclonal antibodies are created in a laboratory. They can target a particular virus or infection such as COVID-19.
How does monoclonal antibody therapy work?
Monoclonal antibodies are given by IV or a single-dose injection to people diagnosed with COVID-19. This therapy uses COVID-19 antibodies to help a person’s body fight off the infection. The injection is a lower dosage than the infusion therapy.
What monoclonal antibody therapies for COVID-19 are available?
The Food and Drug Administration (FDA) has approved emergency use authorization for five antibody infusion therapies:
Is monoclonal antibody therapy effective against the Omicron variant?
So far, it appears only one of the monoclonal antibody treatments – sotrovimab – is effective against the Omicron variant for outpatient treatment. Most of the other monoclonal antibody treatments have limited or no effectiveness against the Omicron variant .
Who should get monoclonal antibody therapy?
Monoclonal antibody treatment is now available for three specific uses:
Who is at high risk for severe illness from COVID-19?
While anybody can get very sick or even die from COVID-19, those most at risk include:
What COVID-19 treatment is available for people diagnosed with COVID-19?
If you are diagnosed with COVID-19 but aren’t sick enough to be hospitalized, you may think there isn’t much you can do. It is important to:
