What will the nurse teach the patient to avoid from prednisone?
The nurse will teach her to gradually decrease her dose of prednisone to avoid a) gastrointestinal problems. b) menstrual irregularities. c) hypokalemia. d) adrenal insufficiency.
What is Prednisone used to treat?
Prednisone is also used alone or with other drugs to treat many other diseases and conditions. The drug continues to be studied in the treatment of many types of cancer and other conditions. More About Prednisone. Definition from the NCI Drug Dictionary - Detailed scientific definition and other names for this drug.
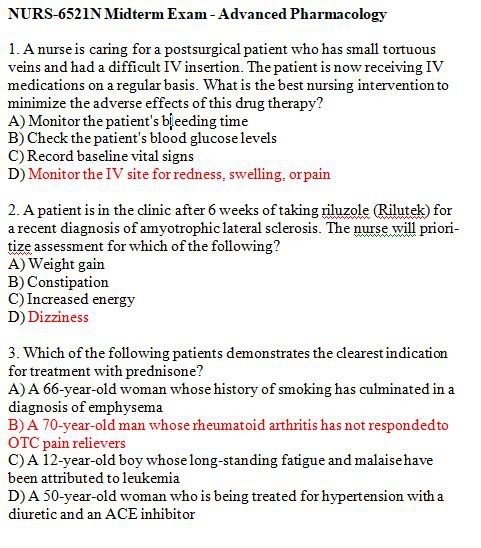
What are the indications for glucocorticoids such as prednisone?
(There are numerous clinical indications for treatment with glucocorticoids such as prednisone. Among these are inflammatory diseases such as rheumatoid arthritis. Emphysema, hypertension, and leukemia are not health problems that are typically treated with corticosteroids.)
How should I care for a client who is on prednisone?
Carefully assess the client for infections. (It is important to monitor clients who are taking prednisone carefully for signs of infection, because prednisone's immunologic activity may mask the symptoms of infection. Antacids may normally be used alongside prednisone.

Which conditions are indications for glucocorticoid drugs?
Glucocorticoids treat many conditions that are caused by inflammation, such as:Asthma.Chronic obstructive pulmonary disease (COPD)Allergies.Rheumatoid arthritis.Osteoarthritis.Crohn's disease and other types of inflammatory bowel disease.Eczema and other skin conditions.Multiple sclerosis.More items...
What adverse effects should the nurse discuss with a client prescribed long term systemic corticosteroid therapy?
Osteoporosis, adrenal suppression, hyperglycemia, dyslipidemia, cardiovascular disease, Cushing's syndrome, psychiatric disturbances and immunosuppression are among the more serious side effects noted with systemic corticosteroid therapy, particularly when used at high doses for prolonged periods.
What are the contraindications of using steroids?
Contraindications to corticosteroids include hypersensitivity to any component of the formulation, concurrent administration of live or live-attenuated vaccines (when using immunosuppressive dosages), systemic fungal infection, osteoporosis, uncontrolled hyperglycemia, diabetes mellitus, glaucoma, joint infection, ...
Which should a client be monitored for when prescribed a glucocorticoid?
They also include more specific recommendations on which parameters should be monitored during follow-up, including body weight, blood pressure, serum lipids, blood and/or urine glucose, infections, osteoporotic fractures, or eye adverse effects.
What is prednisone used to treat?
Prednisone is used to treat conditions such as arthritis, blood disorders, breathing problems, severe allergies, skin diseases, cancer, eye problems, and immune system disorders. Prednisone belongs to a class of drugs known as corticosteroids.
What are the nursing implications of prednisone?
Nursing considerationsAdminister once-a-day doses before 9AM to mimic normal peak corticosteroid blood levels.Increase dosage when patient is subject to stress.WARNING: Taper doses when discontinuing high-dose or long-term therapy to avoid adrenal insufficiency.More items...
What is the indication of prednisone?
Prednisone is an FDA-approved, delayed-release corticosteroid indicated as an anti-inflammatory or immunosuppressive agent to treat a broad range of diseases, including immunosuppressive/endocrine, rheumatic, collagen, dermatologic, allergic states, ophthalmic, respiratory, hematologic, neoplastic, edematous, ...
Who should avoid using corticosteroids?
You should also check with your doctor if you have a history of:nose injuries.surgeries on your nose.nose sores.infections.heart attack.liver disease.type 2 diabetes.underactive thyroid, or hypothyroidism.More items...•
In which of the following disease are corticosteroids indicated?
Long-term oral corticosteroid therapy may be necessary for chronic illnesses such as polymyalgia rheumatica, SLE, RA, vasculitis, myositis, IgG4-related disease, chronic myelogenous leukemia (CML), lymphoma, leukemia, multiple sclerosis, organ transplantation, etc.
What should I monitor with prednisone?
Prednisone may increase the risk that you will develop osteoporosis....If you experience any of the following symptoms, call your doctor immediately:Confusion.Depression.Difficulty breathing or swallowing.Dry, hacking cough.Eye pain, redness or tearing.Hives.Irregular heartbeat.Itching.More items...
What are the side effects of prednisone?
Prednisone may cause side effects. Tell your doctor if any of these symptoms are severe or do not go away:headache.dizziness.difficulty falling asleep or staying asleep.inappropriate happiness.extreme changes in mood.changes in personality.bulging eyes.acne.More items...•
Which laboratory value would the nurse monitor in a patient receiving methylprednisolone?
Blood pressure, blood glucose, electrolytes, weight, bone mineral density, HPA hypothalamic-pituitary-adrenal (HPA) axis suppression, and intraocular pressure all require monitoring in patients taking methylprednisolone.
What is prednisone used for?
Prednisone is approved to be used to reduce inflammation and suppress (lower) the body's immune response. It is used with other drugs to treat the following types of cancer: Acute lymphoblastic leukemia (ALL) and acute myeloid leukemia (AML). It is used as palliative therapy in adults and children.
Why are drugs studied?
Drugs are often studied to find out if they can help treat or prevent conditions other than the ones they are approved for. This patient information sheet applies only to approved uses of the drug. However, much of the information may also apply to unapproved uses that are being studied.
Is prednisone used for hypersensitivity?
Thrombocytopenia (low platelet levels) in adults. Prednisone is also used alone or with other drugs to treat many other diseases and conditions.
Is a syringe a substitute for medical advice?
It is not a substitute for medical advice. The information may not cover all possible uses, actions, interactions, or side effects of this drug, or precautions to be taken while using it. Please see your health care professional for more information about your specific medical condition and the use of this drug.
Is prednisone used for T cell lymphoma?
Mycosis fungoides (a type of cutaneous T-cell lymphoma ). Non-Hodgkin lymphoma. It is used as palliative therapy in adults. Prednisone is also used alone or with other drugs to prevent or treat the following conditions related to cancer: Anemia.
How long does methylprednisolone last?
Other corticoids, including methylprednisolone, hydrocortisone, Prednisone, and prednisolone, are considered to be short acting (producing adrenocortical suppression for 1¼ to 1½ days following a single dose) and thus are recommended for alternate day therapy.
Why should corticosteroids be used for herpes simplex?
Corticosteroids should be used cautiously in patients with ocular herpes simplex because of possible corneal perforation. The lowest possible dose of corticosteroid should be used to control the condition under treatment, and when reduction in dosage is possible, the reduction should be gradual.
What is ADT in medicine?
ADT is a corticosteroid dosing regimen in which twice the usual daily dose of corticoid is administered every other morning. The purpose of this mode of therapy is to provide the patient requiring long-term pharmacologic dose treatment with the beneficial effects of corticoids while minimizing certain undesirable effects, including pituitary-adrenal suppression, the Cushingoid state, corticoid withdrawal symptoms, and growth suppression in children.
How long does adrenocortical insufficiency last?
This type of relative insufficiency may persist for months after discontinuation of therapy; therefore, in any situation of stress occurring during that period, hormone therapy should be reinstituted.
What is the purpose of glucocorticoids?
Naturally occurring glucocorticoids (hydrocortisone and cortisone), which also have salt-retaining properties, are used as replacement therapy in adrenocortical deficiency states. Their synthetic analogs are primarily used for their potent anti-inflammatory effects in disorders of many organ systems.
Can corticosteroids mask infection?
In patients on corticosteroid therapy subjected to unusual stress, increased dosage of rapidly acting corticosteroids before, during, and after the stressful situation is indicated. Corticosteroids may mask some signs of infection, and new infections may appear during their use.
Is cortisone a primary or secondary adrenocortical insufficiency
Primary or secondary adrenocortical insufficiency (hydrocortisone or cortisone is the first choice; synthetic analogs may be used in conjunction with mineralocorticoids where applicable; in infancy mineralocorticoid supplementation is of particular importance) Congenital adrenal hyperplasia.
What should a nurse monitor for in a patient with fludrocortisone?
Rationale: The nurse should monitor for edema, hypertension, congestive heart failure, enlargement of the heart, increased sweating, and allergic skin rash in the patient as adverse reactions to the drug. Sore throat, malaise, and nasal congestion are not adverse reactions to the fludrocortisone drug.
When should I take cortisol?
Rationale: Corticosteroids should be taken immediately on awaking in the morning in order to mimic the normal diurnal pattern. The peak levels of cortisol usually come between 6:00 AM and 8:00 AM. The levels then fall off slowly and reach a low in the late evening with the lowest levels around midnight.
What are the symptoms of desmopressin?
Rationale: Excessive dosage of desmopressin is manifested as water intoxication (fluid overload). Signs and symptoms include confusion, drowsiness, and headache. The nurse should assess the vital signs of this client and notify the health care provider.
What are the characteristics of a cushingoid?
Long-term administration can cause Cushingoid characteristics, including muscle weakness and atrophy, obesity, and "moon face" (the presence of abnormal fat deposits in the cheeks). A client is diagnosed with septic shock. What would the nurse expect a long course of low-dose corticosteroids to do?
Why is IV insertion so difficult?
Rationale: The client's thinning skin may make IV insertion more difficult because the skin is so much more fragile and it bruises so easily due to capillary fragility. You are caring for an 84-year-old diabetic client who is receiving hydrocortisone 40 mg daily PO for treatment of an arthritic flare-up.
What are the conditions that are aggravated by the use of drugs?
Older adults are especially likely to have conditions that are aggravated by the drugs (e.g., congestive heart failure, hypertension, diabetes mellitus, arthritis, osteoporosis, increased susceptibility to infection, concomitant drug therapy that increases risks of gastrointestinal ulceration and bleeding).
Which is better for cerebral edema: IV or PO?
Dexamethasone is the only medication that is used for cerebral edema. The IV is best compared to the IV route, because it is more rapid. After a craniotomy, the drug of choice is either IV or PO dexamethasone. Click again to see term 👆. Tap again to see term 👆.
When should I take hydrocortisone?
The patient takes hydrocortisone every evening at bedtime. (Hydrocortisone therapy should be given prior to 9 a.m. to minimize suppression of the hypothalamic-pituitary axis (HPA). The nurse should question the patient taking hydrocortisone in the evening. The other answers are acceptable administration techniques.)
What are the signs of a client taking long term corticosteroid therapy?
The nurse would report these if the client reported they were getting worse or interfering with the client's activities of daily living. Slight pedal edema may or may not be significant.) A client is taking long-term corticosteroid therapy.
What is the hormone used to regulate blood glucose levels?
Insulin is the hormone used for regulating the blood glucose level. Penicillins and cephalosporins are examples of bactericidal agents used to fight infections.) A nurse is administering hydrocortisone cypionate (Cortef) to a child.
What are the symptoms of desmopressin?
(Excessive dosage of desmopressin is manifested as water intoxication (fluid overload). Signs and symptoms include confusion, drowsiness, and headache. The nurse should assess the vital signs of this client and notify the health care provider.
What are the health problems that are not treated with corticosteroids?
Among these are inflammatory diseases such as rheumatoid arthritis. Emphysema, hypertension, and leukemia are not health problems that are typically treated with corticosteroids.) A patient being treated for Cushing's disease is upset about body changes.
Is hydrocortisone dose limiting?
Headaches, weakness, and hyperglycemia would not be dose limiting, because patients can be taught to cope with weakness, treated for headaches, given insulin, or taught diet modifications for hyperglycemia.) A patient receiving hydrocortisone has started estrogen hormonal replacement therapy.
Can hydrocortisone cause fluid retention?
(Corticosteroids create a risk for infection due to immune suppression; infection control measures are a priority. When taking hydrocortisone daily, the client should not increase dietary sodium because of a risk for fluid retention.
Prednisone Description
Actions
Warnings
Precautions
Adverse Reactions
Dosage and Administration
- The initial dosage of Prednisone may vary from 5 mg to 60 mg of Prednisone per day depending on the specific disease entity being treated. In situations of less severity lower doses will generally suffice while in selected patients higher initial doses may be required. The initial dosage should be maintained or adjusted until a satisfactory respons...
How Supplied
Frequently Asked Questions