Explore
Oct 26, 2021 · Supplemental oxygen, also known as oxygen therapy [7], could also alleviate symptoms of central sleep apnea, and you can choose from different devices to use in the comfort of your home. If you are new to oxygen therapy, your physician can help select the best device for you. The air is usually provided through nasal prongs or a face mask.
What are the best treatments for sleep apnea?
Dec 13, 2019 · Using nasal sprays or allergy medicines The breathing devices that are most commonly used to treat obstructive sleep apnea – such as continuous positive airway pressure (CPAP), automatic positive airway pressure (APAP) or variable positive airway pressure (VPAP) – may be prescribed as central sleep apnea treatment options, as well.
What is the best device for central sleep apnea?
Sep 01, 2020 · For many patients with central sleep apnea, the use of CPAP or BiPAP machines can decrease cessations in respiration. Supplemental oxygen may be used in a similar way. In 2017, the Food and Drug Administration (FDA) approved an implantable device 8 that stimulates breathing-related muscles as a treatment for CSA.
What is treatment-emergent Central apnea?
Bilevel positive airway pressure (BPAP). This is another treatment used for OSA sufferers that can be effective for central sleep apnea patients. Similar to a CPAP mask, a BPAP device adjusts the amount of air delivered to the lungs depending on whether the patient is inhaling or exhaling. Adaptive servo-ventilation (ASV).
Can CPAP help with central sleep apnea?
Central sleep apnea (CSA) is characterized by a lack of drive to breathe during sleep, resulting in repetitive periods of insufficient ventilation and compromised gas exchange. These nighttime breathing disturbances can lead to important comorbidity and increased risk of adverse cardiovascular outcomes.
What is the most effective treatment for sleep apnea?
This air pressure prevents obstructive sleep apnea and snoring. Although CPAP is the most consistently successful and most commonly used method of treating obstructive sleep apnea, some people find the mask cumbersome, uncomfortable or loud.Jul 27, 2021
What is centralized sleep apnea?
Central sleep apnea is a disorder in which your breathing repeatedly stops and starts during sleep. Central sleep apnea occurs because your brain doesn't send proper signals to the muscles that control your breathing.Aug 7, 2021
Is BiPAP used for central sleep apnea?
BiPAP is primarily used to treat central sleep apnea (CSA), as well as heart, lung, and neurological disorders that require structured airway support during sleep. Both CPAP and BiPAP machines are available with a range of accessories, both integrated and after-market.Apr 8, 2022
What causes treatment-emergent central sleep apnea?
Complex sleep apnea is also referred to as treatment-emergent central sleep apnea. Complex sleep apnea occurs when someone who previously had obstructive sleep apnea develops central sleep apnea due to treatment with continuous positive airway pressure (CPAP).Nov 2, 2021
What is the most common cause of central sleep apnea?
In most cases, central sleep apnea is associated with obstructive sleep apnea syndromes or is caused by an underlying medical condition, recent ascent to high altitude, or narcotic use. Primary central sleep apnea is a rare condition, the etiology of which is not entirely understood.Aug 25, 2020
What is a BiPAP used for?
BiPAP stands for bi-level positive airway pressure. It is one type of PAP, or positive airway pressure machine, that is used to maintain a consistent breathing pattern at night or during symptom flare-ups in people with COPD.
How does ASV treat central apnea?
ASV is similar to continuous positive air pressure (CPAP) devices, but it's a newer technology. These devices track how you breathe while you sleep. They react to your breathing pattern and adjust air pressure to help you breathe more normally during the night.Apr 25, 2020
How does BiPAP help sleep apnea?
BiPAP refers to Bilevel or two-level Positive Airway Pressure. Like CPAP, this sleep apnea treatment works by sending air through a tube into a mask that fits over the nose. While CPAP generally delivers a single pressure, BiPAP delivers two: an inhale pressure and an exhale pressure.
What Is Central Sleep Apnea?
Sleep apnea is when a person’s breathing repeatedly starts and stops while they are asleep. Central [1] sleep apnea is caused by the brain not sending signals to the muscles that regulate breathing. Central sleep apnea can result from various health and situational circumstances, and we will cover these in detail further below.
Central Sleep Apnea Symptoms
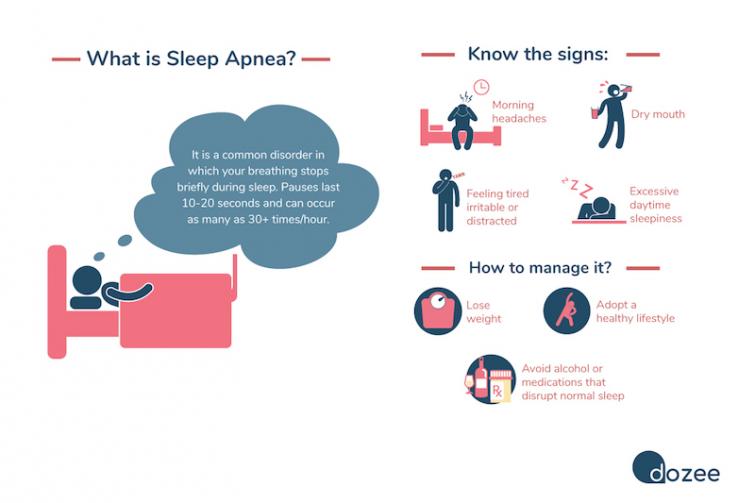
If you notice any of the following symptoms, you may have central sleep apnea and should schedule a visit with your doctor.
What Causes It?
According to experts, less than ten percent [4] of patients referred to sleep laboratories have central sleep apnea. Though the numbers are significantly lower than obstructive, central sleep apnea can be just as dangerous to individuals’ health.
Diagnosing CSA
To get a formal central sleep apnea diagnosis, you will need to first consult your doctor, who will likely do an initial evaluation. Following this, your physician may refer you to a sleep specialist for further testing.
How to Treat Central Sleep Apnea
By addressing the root cause of your CSA, a healthcare professional can help you find the best central sleep apnea treatment plan. The Mayo Clinic reports that the following remedies can aid with central sleep apnea.
Frequently Asked Questions
Certain factors can put some at a greater risk of developing central sleep apnea, as reported by the Mayo Clinic.
What is the treatment for obstructive sleep apnea?
The first step is usually to make behavioral or lifestyle changes, which often include: The breathing devices that are most commonly used to treat obstructive sleep apnea – such as continuous positive airway pressure (CPAP) , automatic positive airway pressure ...
What breathing devices are used to treat sleep apnea?
The breathing devices that are most commonly used to treat obstructive sleep apnea – such as continuous positive airway pressure (CPAP) , automatic positive airway pressure (APAP) or variable positive airway pressure (VPAP) ...
Why is central sleep apnea so complicated?
Because central sleep apnea is caused by non-physical causes, the options for successful treatment can begin to get more complicated in the event that the above methods don’t yield results.
What diseases can cause central sleep apnea?
Hypothyroid disease. Kidney failure. Alzheimer’s disease. Amyotrophic lateral sclerosis (ALS, also known as Lou Gehrig’s disease) Encephalitis. Brain damage. In these cases, your physician will likely prescribe central sleep apnea treatment that focuses on treating those conditions first and foremost – which, in theory, ...
Is CSA a neurological condition?
CSA, on the other hand, has neurological causes – think of it as your brain failing to tell your body to breathe consistently throughout the night. So, given the different nature of these two types of sleep apnea, it makes sense that central sleep apnea treatment options may be considerably different than obstructive sleep apnea treatment options.
Can narcotics cause sleep apnea?
If narcotic medicine is causing the apnea, the dosage may need to be lowered or the medicine changed.” 1. Finally, because it’s caused by your nervous system and mental processes, central sleep apnea has also been known to resolve itself without treatment – in fact, Medscape states that 20 percent of all central sleep apnea cases resolve themselves ...
Can sleep apnea be mild?
If your sleep apnea is thought to be mild – that is, if your central sleep apnea symptoms aren’t severe, or don’t have much of an effect on your personal life – your physician will most likely start you off with basic treatment options. These are the treatments consistent with both CSA and OSA. The first step is usually to make behavioral ...
What is the second category of sleep apnea?
The second category of central sleep apnea involves hyperventilation (breathing deep breaths and quickly), followed by pauses in breathing. This type of central sleep apnea occurs because of aberrant pacing and control of respiration. Hyperventilation-type of central sleep apnea includes the following subtypes:
How many people have central sleep apnea?
While the exact number of people with central sleep apnea is unknown, it is estimated that about .9% of people over 40 4 in the United States have the condition. Though it affects both men and women, it occurs more often in men of greater than 65 years old. People who have a heart condition, use narcotics, suffer from a stroke, ...
What is Cheyne Stokes breathing?
Cheyne-Stokes Breathing: Cheynes-Stokes breathing is a unique type of central sleep apnea commonly found in people with heart conditions. The most common heart conditions associated with Cheynes-Stokes breathing 6 include heart failure and atrial fibrillation.
What happens when you breathe at high altitude?
As a response, a person’s breathing becomes faster and larger. During sleep, this may cause pauses in breath.
What is hypoventilation type sleep apnea?
Hypoventilation-type of central sleep apnea includes the following subtypes: Narcotic-Induced Central Sleep Apnea: In this type of central sleep apnea, the use of narcotics, such as opioids, diminishes the brain’s ability to properly initiate and regulate breathing.
What is CSA in medical terms?
Further information can be found in our privacy policy. Central sleep apnea (CSA) is a disorder that affects breathing during sleep. It is distinct from obstructive sleep apnea (OSA), which is much more common and well-known. CSA is often tied to an underlying health condition, and if it is left unaddressed, it may affect overall health by causing ...
How does CSA affect sleep?
CSA is often tied to an underlying health condition, and if it is left unaddressed, it may affect overall health by causing fragmented sleep, daytime drowsiness, thinking problems, moodiness, and fatigue. While there can be overlap with the causes, symptoms, and treatments of obstructive sleep apnea, central sleep apnea is a distinct disorder, ...
What is central sleep apnea?
Central sleep apnea is a neurological condition —in other words, the brain is not sending the correct signals to the respiratory system to keep breathing while the patient sleeps. Sometimes another medical condition causes CSA; sometimes, pain medication can lead to it; and sometimes, the apnea occurs for no known reason.
What is a phrenic nerve?
Phrenic nerve stimulation is delivered by a pacemaker-like implantable device that stimulates a nerve in the chest (phrenic nerve) to send signals to the diaphragm to control breathing. It monitors respiratory signals while you sleep and helps restore normal breathing patterns.
What is the purpose of ASV?
If the user is breathing fine, the device reduces the air it provides. It the patient’s breathing begins to pause, ASV increases the oxygen. Phrenic Nerve Stimulation. Phrenic Nerve Stimulation is a new FDA-approved therapy for moderate to severe central sleep apnea in adult patients.
Can CSA cause snoring?
CSA patients might not snore, may be at their ideal weight, and may have not had a history of sleep disorders yet still find themselves with the condition characterized by pauses in breathing many times during the night. Central sleep apnea is a neurological condition—in other words, the brain is not sending the correct signals to ...
Do you need a mask for a phrenic nerve?
Because the device is implantable and turns on automatically during sleep, it does not require wearing a mask. Phrenic nerve stimulation allows normal breathing to resume by stabilizing carbon dioxide, preventing apneic events and the subsequent period of rapid breathing.
Does codeine cause sleep apnea?
Studies have proved that more powerful pain medications such as morphine, codeine and oxycodone can cause central sleep apnea. Reducing the dosage or not taking them altogether can help, but discussing this option with your doctor and with a sleep specialist is important.
Can a stroke cause central sleep apnea?
Treating the medical condition that is also causing central sleep apnea. Congestive heart failure or the aftermath of a stroke can interfere with night-time breathing and lead to CSA. The solution here is simple: Treat the heart failure or the stroke and the apnea will likely subside.
What is the drug that causes bicarbaturia?
Acetazolamide (Diamox) Acetazolamide is a carbonic anhydrase inhibitor that causes bicarbaturia and metabolic acidosis, which presumably shifts the apneic threshold of PaCO 2 to a lower level. It has been shown to be effective therapy in primary central sleep apnea and CSB in patients with heart failure and in the treatment ...
What is loop gain?
The role of loop gain in determining respiratory instability. A) When loop gain is less than 1, the tendency for an overshoot of the corrective response to an apnea or hypopnea is lessened, and ventilation returns to a steady pattern.
Is acetazolamide a drug of choice?
Due to the heterogeneity of the central sleep apnea syndromes, different medications have been used under different circumstances. No single medication can be considered a drug of choice. [ 1] . Several different medications aimed at improving central sleep apnea include acetazolamide, theophylline, and sedative-hypnotic agents.
How does central sleep apnea affect the body?
The immediate effects of central sleep apnea on the body depend on how long the failure to breathe endures, how short is the interval between failures to breathe, and the presence or absence of independent conditions whose effects amplify those of an apneic episode. Brain cells need constant oxygen to live, and if the level ...
How do you know if you have central sleep apnea?
Signs and symptoms of central sleep apnea. Signs: Lack of abdominal and thoracic movement for 10 seconds or longer during sleep and coincident with breathing pauses. Symptoms: Inability, either complete or without excessive effort, to voluntarily operate diaphragm and other thoracic muscles upon awakening.
What is CSA in medical terms?
Specialty. Neurology. Central sleep apnea ( CSA) or central sleep apnea syndrome ( CSAS) is a sleep -related disorder in which the effort to breathe is diminished or absent, typically for 10 to 30 seconds either intermittently or in cycles, and is usually associated with a reduction in blood oxygen saturation.
What happens after a patient receives a diagnosis?
After a patient receives a diagnosis, the diagnosing physician can provide different options for treatment. If central sleep apnea is medication-induced (e.g., opioids), reducing the dose or eventual withdrawal of the offending medication often improves CSA.
What is the curse of Ondine?
Congenital central hypoventilation syndrome (CCHS), often referred to by its older name " Ondine's curse ," is a rare and very severe inborn form of abnormal interruption and reduction in breathing during sleep. This condition involves a specific homeobox gene, PHOX2B, which guides maturation of the autonomic nervous system; certain loss-of-function mutations interfere with the brain's development of the ability to effectively control breathing. There may be a recognizable pattern of facial features among individuals affected with this syndrome.
What is the function of a phrenic nerve?
After a commonly performed procedure, the device stimulates a nerve in the chest (phrenic nerve) to send signals to the large muscle that controls breathing (the diaphragm). It monitors respiratory signals during sleep and helps restore normal breathing patterns.
What is the brain's respiratory control center?
In pure central sleep apnea, the brain's respiratory control centers, located in the region of the human brain known as the pre-Botzinger complex, are imbalanced during sleep and fail to give the signal to inhale, causing the individual to miss one or more cycles of breathing.
