
For patients seeking diagnosis and rheumatoid arthritis treatment from a leading research center and treatment provider, Brigham and Women's Hospital (BWH) in Boston offers a world-class Center for Arthritis and Joint Diseases. Learn more about rheumatoid arthritis treatment services at BWH.
- Mayo Clinic.
- Brigham and Women's Hospital.
- Massachusetts General Hospital.
- UCSF Medical Center.
- UCLA Medical Center.
- NYU Langone Orthopedic Hospital.
- University of Alabama at Birmingham Hospital.
What is the best hospital for rheumatoid arthritis treatment?
Jan 19, 2016. Diagnosing rheumatoid arthritis (RA) early in the disease process is ideal, because treatments are more likely to be effective and less damage will occur. When determining the best treatment protocol, Vivian Bykerk, MD, rheumatologist and director of the Inflammatory Arthritis Center of Excellence at HSS.
How is rheumatoid arthritis (RA) treated?
Rheumatoid arthritis is a chronic disorder for which there is no known cure. Fortunately in the last few years, a shift in strategy toward the earlier institution of disease modifying drugs and the availability of new classes of medications have greatly improved the outcomes that can be expected by most patients.
What is the safest treatment for rheumatoid arthritis?
The BWH Center for Arthritis and Joint Diseases provides world-class care and treatment for more than 100 causes of arthritis, including lupus, gout and pseudogout, spine disorders, and the immune system, as happens in rheumatoid arthritis. The Center has a long history of innovation and focus on arthritis – it originated as the Robert Breck Brigham Hospital, the first teaching …
What type of Doctor treats rheumatoid arthritis?
As RA specialists, rheumatologists may be best qualified to diagnose RA and develop an effective treatment plan for your goals. RA can be a serious chronic disease—but a prompt, accurate diagnosis and appropriate management can better your chances of effective RA symptom improvement and may help prevent permanent joint damage.
What is the best hospital for autoimmune diseases?
Johns Hopkins Hospital. 844-741-0147. ... Cleveland Clinic. Cleveland, OH 44195-5108. ... Mayo Clinic. 507-516-3231. ... Hospital for Special Surgery, New York-Presbyterian University Hospital of Columbia and Cornell. ... Brigham and Women's Hospital. ... Massachusetts General Hospital. ... UCSF Health-UCSF Medical Center. ... NYU Langone Hospitals.More items...
Who is the top rheumatologist in the US?
Top 10 U.S. Specialists in Rheumatoid ArthritisRoy Fleischmann, M.D., University of Texas Southwestern.Mark Genovese, M.D., Stanford University.Arthur Kavanaugh, M.D., University of California San Diego.Joel Kremer, M.D., Center for Rheumatology Albany.Michael Weinblatt, M.D., Brigham and Women's Hospital.More items...•Nov 19, 2020
Which doctor is best for rheumatoid arthritis?
Rheumatologists – Rheumatologists specialize in musculoskeletal diseases and autoimmune conditions. They treat all types of arthritis, including osteoarthritis, rheumatoid arthritis and psoriatic arthritis.Nov 18, 2019
Which Mayo Clinic is best for rheumatology?
Mayo Clinic's combination of clinical, research and education efforts means you receive the best possible rheumatologic care. Mayo Clinic in Rochester, Minn., is ranked among the Best Hospitals for rheumatology by U.S. News & World Report.Apr 1, 2020
Which Mayo Clinic is best for autoimmune disease?
Mayo Clinic rheumatologists are experts in the treatment of people with inflammatory conditions and autoimmune diseases of the body's musculoskeletal system.Apr 1, 2020
Which hospital is best for rheumatology?
The top-ranked hospitals for rheumatology in the 2018-2019 report are:Mayo Clinic.Brigham and Women's Hospital.Massachusetts General Hospital.UCSF Medical Center.UCLA Medical Center.NYU Langone Orthopedic Hospital.University of Alabama at Birmingham Hospital.More items...•Aug 17, 2018
What is the new medicine for rheumatoid arthritis?
People with Rheumatoid Arthritis (RA) could soon benefit from a new drug treatment that not only suppresses inflammation but also significantly reduces patient-reported pain scores. Otilimab is a monoclonal antibody, biologic drug, which targets and suppresses the inflammatory cytokine GM-CSF.
What can I take instead of methotrexate for RA?
In elderly patients with RA who are unable to tolerate methotrexate, the alternatives are hydroxychloroquine or sulfasalazine for mild-to-moderate disease and cyclosporin or leflunomide for severe disease, given in combination with low-dose oral corticosteroids.
Can RA go into remission forever?
Rheumatoid arthritis is generally considered a chronic, lifelong condition. However, new treatments sometimes lead to dramatic improvements in the signs and symptoms of the condition. They can even prevent joint damage and lead to remission. Doctors and people living with RA may both have remission as a goal.Feb 11, 2019
Is rheumatoid arthritis hereditary?
While RA isn't hereditary, your genetics can increase your chances of developing this autoimmune disorder. Researchers have established a number of the genetic markers that increase this risk. These genes are associated with the immune system, chronic inflammation, and with RA in particular.
How do you permanently treat rheumatoid arthritis?
There is no cure for rheumatoid arthritis. But clinical studies indicate that remission of symptoms is more likely when treatment begins early with medications known as disease-modifying antirheumatic drugs (DMARDs).May 18, 2021
What is the test for rheumatoid arthritis?
An anti-CCP antibody test — also called an ACCP test or CCP-test — looks for the presence of these antibodies to help confirm rheumatoid arthritis. An anti-CCP test can also help doctors determine the severity of a rheumatoid arthritis case.Oct 25, 2021
What is the goal of rheumatoid arthritis treatment?
The goal of rheumatoid arthritis treatment now aims toward achieving the lowest possible level of arthritis disease activity and remission if possible, minimizing joint damage, and enhancing physical function and quality of life.
Why is rest important for musculoskeletal health?
Because obesity stresses the musculoskeletal system , ideal body weight should be achieved and maintained. Rest, in general, is an important feature of management. When the joints are actively inflamed, vigorous activity should be avoided because of the danger of intensifying joint inflammation or causing traumatic injury to structures weakened by inflammation. On the other hand, patients should be urged to maintain a modest level of activity to prevent joint laxity and muscular atrophy. Splinting of acutely inflamed joints, particularly at night and the use of walking aids (canes, walkers) are all effective means of reducing stress on specific joints. A consultation with a physical and an occupational therapist is recommended early in the course.
What are the different types of rheumatoid arthritis drugs?
There are three general classes of drugs commonly used in the treatment of rheumatoid arthritis: non-steroidal anti-inflammatory agents (NSAIDs), corticosteroids, and disease modifying anti-rheumatic drugs (DMARDs). NSAIDs and corticosteroids have a short onset of action while DMARDs can take several weeks or months to demonstrate a clinical effect. DMARDs include methotrexate, sulfasalazine, leflunomide (Arava®), etanercept (Enbrel®), infliximab (Remicade®), adalimumab (Humira®), certolizumab pegol (Cimzia®), golimumab (Simponi®), abatacept (Orencia®), rituximab (Rituxan®), tocilizumab (Actemra®), anakinra (Kineret®), antimalarials (e.g. Plaquenil®). Other immunomodulators are occasionally used including azathioprine (Imuran) and cyclosporine. Because cartilage damage and bony erosions frequently occur within the first two years of disease, rheumatologists now move aggressively to a DMARD agent early in the course of disease, usually as soon as a diagnosis is confirmed. Analgesic drugs are also sometimes helpful in decreasing pain until DMARDs take effect. A summary table of how to monitor drug treatment in rheumatoid arthritis is included.
What are the benefits of DMARD?
Although both NSAIDs and DMARD agents improve symptoms of active rheumatoid arthritis, only DMARD agents have been shown to alter the disease course and improve radiographic outcomes. DMARDs have an effect upon rheumatoid arthritis that is different and may be slower. In most cases, when the diagnosis of rheumatoid arthritis is confirmed, DMARD agents should be started. The presence of erosions or joint space narrowing on x-rays of the involved joints is a clear indication for DMARD therapy, however one should not wait for x-ray changes to occur. The currently available drugs include: 1 Methotrexate (Rheumatrex®, Trexall®) 2 Hydroxychloroquine (Plaquenil ®) 3 Sulfasalazine (Azulfidine®) 4 Leflunomide (Arava®) 5 Tumor Necrosis Factor Inhibitors — etanercept (Enbrel®, adalimumab (Humira ®), and infliximab (Remicade®), certolizumab pegol (Cimzia®), golimumab (Simponi®) 6 T-cell Costimulatory Blocking Agents —abatacept (Orencia®) 7 B cell Depleting Agents —rituximab (Rituxan®) 8 Interleukin-6 (IL-6) Inhibitors– tocilizumab (Actemra®) 9 Interleukin-1 (IL-1) Receptor Antagonist Therapy —anakinra (Kineret®) 10 Intramuscular Gold 11 Other Immunomodulatory and Cytotoxic agents — azathioprine (Imuran®) and cyclosporine A (Neoral®, Sandimmune®)
What is a DMARD?
Disease Modifying Anti-rheumatic Drugs (DMARDS) Although both NSAIDs and DMARD agents improve symptoms of active rheumatoid arthritis, only DMARD agents have been shown to alter the disease course and improve radiographic outcomes. DMARDs have an effect upon rheumatoid arthritis that is different and may be slower.
How long does it take for folic acid to work after methotrexate?
These side effects can often be overcome by increasing folic acid or using an activated form of folic acid known as folinic acid (leukovorin®) given as a 5mg dose 12 hours and sometimes 24 hours after methotrexate is given. Some patients complain of GI upset (nausea or diarrhea) with oral methotrexate.
How long does it take for NSAIDS to work?
Usual Time to Effect: The onset of action is seen in as early as 4 to 6 weeks.
What is the best treatment for RA?
Blocking TNF inhibitors or the activation of T cells is one method of preventing the joint damage that frequently occurs in patients who suffer from RA. This greatly reduces the risk of further damage or infection. Biologic agents are typically prescribed in combination with other medications to fight RA symptoms.
How does a physical therapist help with RA?
Physical therapists can help patients learn appropriate exercises and new ways of approaching tasks that minimize the strain on affected joints while improving overall body strength.
What is DMARDs for arthritis?
DMARDs, or disease-modifying antirheumatic drugs, are long-term medications meant to slow or alter the progression of rheumatoid arthritis by stopping the immune system from attacking healthy tissue. These drugs protect joints and tissues from permanent damage and gradually reduce daily pain.
How do NSAIDs work?
NSAIDs can be taken orally or applied directly to the joint as a patch or cream. Corticosteroid medications or another form of drug used in the treatment of RA. They work in your body similar to hormones as they try to slow the progression of the disease and stop the immune system from attacking healthy tissue.
How does surgery help with RA?
However, surgery potentially enables patients to regain function by repairing the joint damage that frequently occurs with this condition . The overall goal of surgery, when deemed appropriate, is to improve the quality of life of those affected. There are three surgical procedures that RA patients typically receive.
What is tight control for RA?
Depending on the severity of your symptoms, the goals of treatment will be to gain “tight control” of RA, meaning the disease’s activity is kept steadily at a low level. Keeping RA in “tight control” can prevent long-term joint damage. These goals primarily focus on:
Can RA go into remission?
Following a strict treatment regimen could bring RA into remission. Remission means that the level of disease activity has decreased in the body. It is never an indication that symptoms will not return, but following remission, many patients can go for long periods of time without experiencing symptoms. There are many ways to treat rheumatoid ...
What is the BWH Center for Arthritis and Joint Diseases?
The BWH Center for Arthritis and Joint Diseases provides world-class care and treatment for more than 100 causes of arthritis, including lupus, gout and pseudogout, spine disorders, and the immune system, as happens in rheumatoid arthritis.
What is the most common type of arthritis that is caused by the immune system?
Rheumatoid arthritis is an autoimmune disease where certain cells in the immune system malfunction and attack healthy joints. Affecting 1.3 million Americans, it is the most common kind of chronic arthritis that is caused by the immune system.
What is BWH research?
As a leading rheumatology, inflammation, and immunity research facility, BWH has contributed to advances that have significantly changed the practice of rheumatology and rheumatoid arthritis treatment. BWH researchers, for example, have helped to develop the TNF blockade – a highly effective treatment for rheumatoid arthritis and one of the most exciting medical discoveries in the past decade.
Who is the best doctor for RA?
As RA specialists, rheumatologists may be best qualified to diagnose RA and develop an effective treatment plan for your goals. RA can be a serious chronic disease—but a prompt, accurate diagnosis and appropriate management can better your chances of effective RA symptom improvement and may help prevent permanent joint damage.
Why do you see a rheumatologist?
That’s why it’s important to see a rheumatologist as soon as you or your primary care physician suspects you have RA. While your primary care physician should remain an important part of your overall health care, your rheumatologist should take the lead role when it comes to managing your rheumatoid arthritis.
How to fix rheumatoid arthritis?
Surgery may help restore your ability to use your joint. It can also reduce pain and improve function. Rheumatoid arthritis surgery may involve one or more of the following procedures: Synovectomy. Surgery to remove the inflamed lining of the joint (synovium) can help reduce pain and improve the joint's flexibility. Tendon repair.
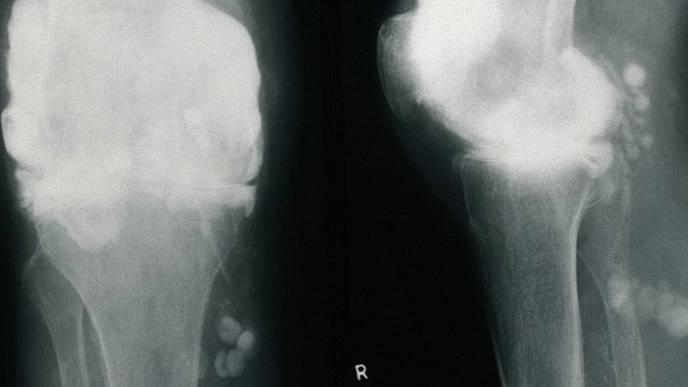
What tests can be done to diagnose rheumatoid arthritis?
Imaging tests. Your doctor may recommend X-rays to help track the progression of rheumatoid arthritis in your joints over time. MRI and ultrasound tests can help your doctor judge the severity of the disease in your body.
What are the drugs that slow the progression of rheumatoid arthritis?
Conventional DMARDs. These drugs can slow the progression of rheumatoid arthritis and save the joints and other tissues from permanent damage. Common DMARDs include methotrexate (Trexall, Otrexup, others), leflunomide (Arava), hydroxychloroquine (Plaquenil) and sulfasalazine (Azulfidine). Side effects vary but may include liver damage ...
How does rheumatoid arthritis affect your life?
The pain and disability associated with rheumatoid arthritis can affect a person's work and family life. Depression and anxiety are common, as are feelings of helplessness and low self-esteem. The degree to which rheumatoid arthritis affects your daily activities depends in part on how well you cope with the disease.
Why is rheumatoid arthritis so difficult to diagnose?
Rheumatoid arthritis can be difficult to diagnose in its early stages because the early signs and symptoms mimic those of many other diseases. There is no one blood test or physical finding to confirm the diagnosis. During the physical exam, your doctor will check your joints for swelling, redness and warmth.
What does elevated erythrocyte sedimentation rate mean?
People with rheumatoid arthritis often have an elevated erythrocyte sedimentation rate (ESR, also known as sed rate) or C-reactive protein (CRP) level, which may indicate the presence of an inflammatory process in the body.
How to get rid of a swollen joint?
If you're just getting started, begin by taking a walk. Avoid exercising tender, injured or severely inflamed joints. Apply heat or cold.
Can you take pain medicine for RA?
But continued use of pain medicine may be a sign your RA symptoms are not being managed effectively.
Is rheumatoid arthritis a treatment plan?
An effective rheumatoid arthritis (RA) treatment plan is unique to everyone. People can react differently to different medications, so it can be normal to try a number of treatment options to see what works for you. Effective treatment plans, including the appropriate medication for you, can help limit the impact RA has on your life.
What is the best way to diagnose RA?
A doctor or a team of doctors who specialize in care of RA patients should diagnose and treat RA. This is especially important because the signs and symptoms of RA are not specific and can look like signs and symptoms of other inflammatory joint diseases.
How to diagnose RA?
RA is diagnosed by reviewing symptoms, conducting a physical examination, and doing X-rays and lab tests. It’s best to diagnose RA early—within 6 months of the onset of symptoms—so that people with the disease can begin treatment to slow or stop disease progression (for example, damage to joints).
What are the consequences of rheumatoid arthritis?
It can cause pain, disability, and premature death. Premature heart disease. People with RA are also at a higher risk for developing other chronic diseases such as heart disease and diabetes.
What is RA in medical terms?
What is rheumatoid arthritis (RA)? Rheumatoid arthritis, or RA, is an autoimmune and inflammatory disease, which means that your immune system attacks healthy cells in your body by mistake, causing inflammation (painful swelling) in the affected parts of the body. RA mainly attacks the joints, usually many joints at once.
Why is RA risk the highest?
The risk of RA may be highest when people with these genes are exposed to environmental factors like smoking or when a person is obese. Smoking. Multiple studies show that cigarette smoking increases a person’s risk of developing RA and can make the disease worse. History of live births.
How to help arthritis?
Learn more about physical activity for arthritis. Go to effective physical activity programs. If you are worried about making arthritis worse or unsure how to safely exercise, participation in physical activity programs can help reduce pain and disability related to RA and improve mood and the ability to move.
How do you know if you have RA?
Signs and symptoms of RA include: Pain or aching in more than one joint. Stiffness in more than one joint. Tenderness and swelling in more than one joint. The same symptoms on both sides of the body (such as in both hands or both knees) Weight loss. Fever.
