How much does it cost to treat hepatitis C virus (HCV)?
Jun 01, 2018 · The table below highlights the average cost of treatment for the combination DAAs currently available. Most of these drugs take at least 12 weeks to cure HCV, while the most recently approved drug ...
Who pays for HCV treatment?
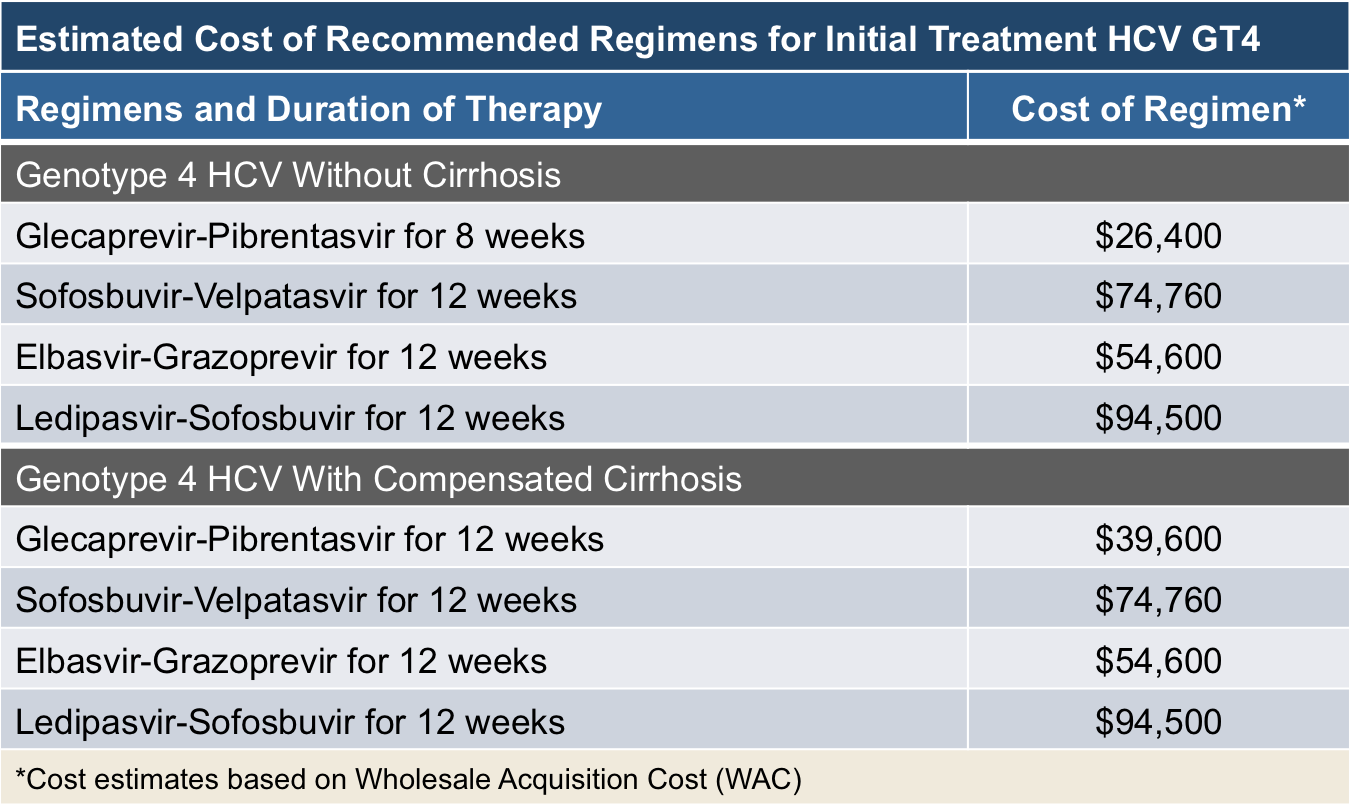
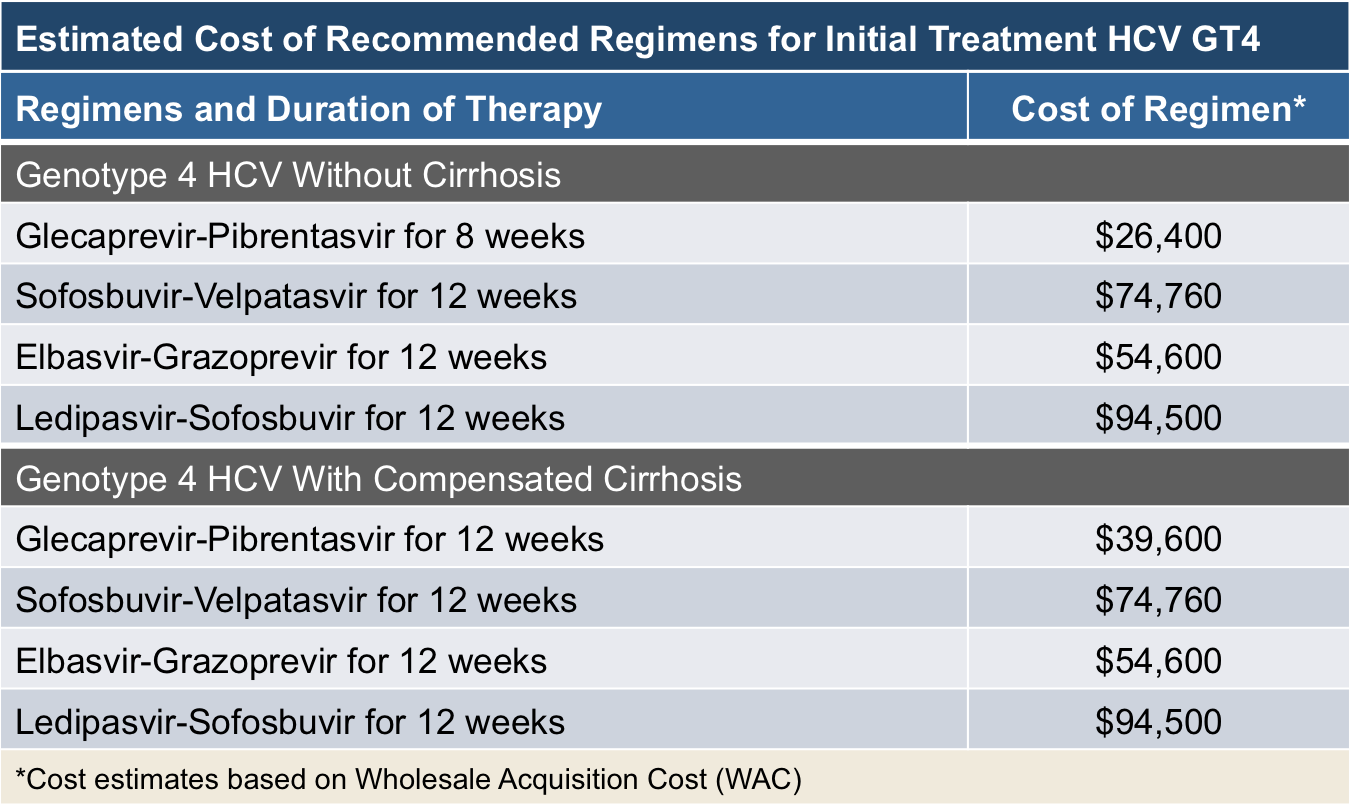
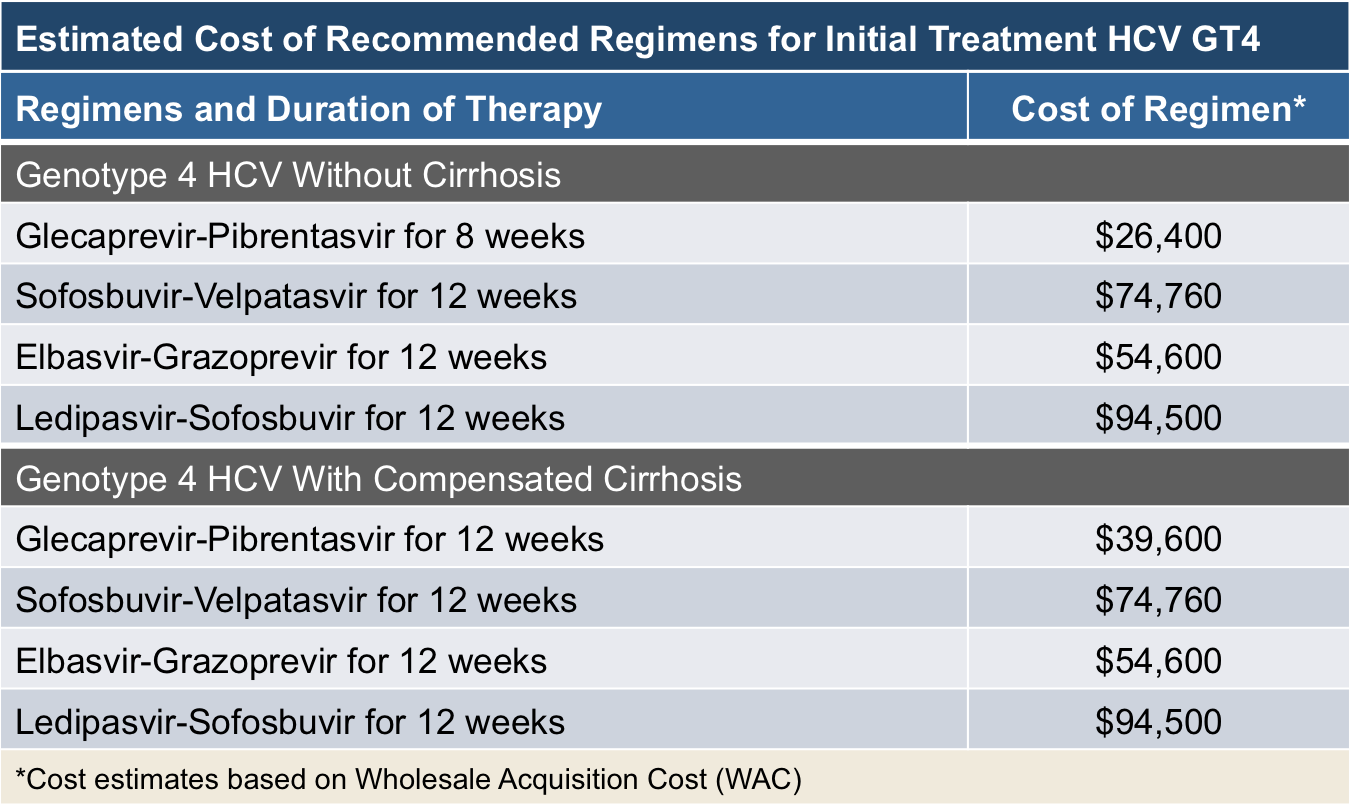
May 20, 2021 · Costs of DAA treatment were based on the wholesale acquisition price of glecaprevir/pibrentasvir (Mavyret; AbbVie): $26,400 to $39,600 for an 8- to 12-week treatment course (Table 1 [part A and ...
What are the new drugs available to treat hepatitis C?
2010 wholesale acquisition costs: 41,803: The total treatment cost input was a function of the regimen used for each genotype in the given year weighted by the prevalence of each genotype. Regimen list prices were identified in RED BOOK. 21 2012 wholesale acquisition costs: 97,196 2014 wholesale acquisition costs: 106,360 2016 wholesale acquisition costs: 68,753
Can I get help paying for hepatitis C drugs?
Dec 13, 2019 · Rates of hepatitis C virus (HCV) treatment in a commercially insured population doubled after availability of new direct-acting antivirals. ... DAAs. 18,19 The published wholesale acquisition cost ...
What is the cost of treating hep C?
The cost of hep C treatment varies depending on the type of drug. However, an 8- to 12-week course can range from $54,000 to $95,000 (or higher). For example, the price of a 12-week course of Zepatier can be as much as $54,600, and a 12-week course of Harvoni can cost as much as $94,500.Sep 2, 2021
How much does Sovaldi cost in America?
Official Answer. The wholesale cost of Sovaldi is $1000 per 400mg tablet. A 12-week treatment course of Sovaldi costs around $84,000 and a 24-week course, $168,00.Apr 23, 2020
How much does Mavyret cost without insurance?
How much does Mavyret cost without insurance? Without insurance, the customers pay an average of $3,168.19 for a refill of Mavyret. However, when you claim your SingleCare savings, you pay a discounted retail price of $2,634.56 for this prescription drug at your neighborhood pharmacy.
What company makes Mavyret?
AbbVie Receives U.S. FDA Approval of MAVYRET™ (glecaprevir/pibrentasvir) for the Treatment of Chronic Hepatitis C in All Major Genotypes (GT 1-6) in as Short as 8 Weeks.Aug 3, 2017
Why is Sovaldi so cheap in India?
The newspaper says that current treatments for the disease in India run about $6,000 and require a 24- to 48-week course of injectables that come with serious side effects. So Sovaldi will be cheaper and easier to administer, with fewer side effects and the ability to cure many of the cases.
What are the side effects of Sovaldi?
Common side effects of Sovaldi include:fatigue,headache,nausea,insomnia,itching,anemia,weakness,rash,More items...
What is the generic for MAVYRET?
Generic Name: glecaprevir-pibrentasvir Chronic hepatitis C infection can cause serious liver problems such as scarring (cirrhosis) or liver cancer. It is not known if this treatment can prevent you from passing the virus to others.
How much does maverick for hep C cost?
Abbvie has priced Mavyret at $13,200 per month, or $26,400 per treatment course, before discounts. Although this is still expensive, Macyret is priced significantly lower than other hepatitis C treatments.Aug 23, 2017
Does Medicare pay for MAVYRET?
Yes. 78% of Medicare prescription drug plans cover this drug.
Is MAVYRET better than Harvoni?
Mavyret is reported to have some advantages over Harvoni including the number of HCV genotypes it covers, the length of treatment required, and the cost of a course of treatment.Aug 25, 2021
What is Maverick for hep C?
MAVYRET is a prescription medicine used to treat adults and children 12 years of age and older or weighing at least 99 pounds (45 kilograms) with chronic (lasting a long time) hepatitis C virus (hep C): Genotypes (GT) 1, 2, 3, 4, 5 or 6 infection without cirrhosis or with compensated cirrhosis.
What is the new medicine for hep C?
The new hepatitis C treatments are sofosbuvir with ledipasvir (Harvoni); sofosbuvir (Sovaldi); daclatasvir (Daklinza); and ribavirin (Ibavyr). These new treatments are now available on the Pharmaceuticals Benefits Scheme.Mar 1, 2016
How much does it cost to cure hepatitis C?
According to the Pharmacy Times, the cost of treatment can be as low as $54,600 for the 12-week course and the entry to the market of new, cheaper drugs is likely to continue to bring the cost of hepatitis C treatments down.
How much does Sovaldi cost?
Sofosbuvir (Sovaldi): This medication costs $1,000 per 400 mg pill. The total cost for a 12-week course is around $84,000, and doctors will typically prescribe it with other medicines, such as simeprevir. Ombitasvir-paritaprevir-ritonavir and dasabuvir (Viekira Pak): The cost for this medication is $83,319 for a 12-week treatment course.
Is hepatitis C treatment successful?
Recent innovations in hepatitis C treatment mean that treatment is usually successful. However, for some people, the costs of these medications can be prohibitive. While prices may decrease in the future, there are currently no guarantees.
Is hepatitis C a direct-acting drug?
In 2014, the United States Food and Drug Administration (FDA) approved drug treatment s called direct-acting antiviral medications that were available in oral form only to treat hepatitis C, according to the journal Open Forum Infectious Diseases . Several medications to treat hepatitis C have met FDA approval since then.
What is the cure rate for hepatitis C?
Direct-acting antivirals (DAAs) are associated with cure rates above 95% for hepatitis C virus (HCV). 1 However, the exorbitant costs of DAAs historically have made access prohibitive for many patients.
Why is Maryland not a direct acting agent for Medicare?
Objectives: Most Medicaid beneficiaries with hepatitis C virus (HCV) are not treated with direct-acting agents because of budget constraints, but they experience costly complications after becoming Medicare eligible. Maryland’s “total coverage” proposal could receive a credit from Medicare to offset Medicaid investments in treatments ...
What is the semi infectious disease model?
The semi-infectious disease model assessed the cost-effectiveness of HCV outcomes based on increased treatment probabilities under the total coverage scenario, compared with 2 scenarios reflecting the current payer model with standard coverage for all beneficiaries or prioritized coverage for all high-risk beneficiaries ( Figure 1 ). In the latter alternative, the 60% of patients with chronic HCV who had a liver fibrosis score of 2 or higher, as opposed to a fibrosis score of 0 or 1, received DAAs first, before lower-risk patients, in order to better manage budget impact. 15
Is DAA coverage for HCV?
Providing total coverage for DAA medications for all patients with HCV is systematically complex and may not be economically viable for state Medicaid programs that face some of the highest rates of HCV among payers. Joint Medicaid-Medicare coverage provides an efficient solution to treat all patients now to reduce harm caused by chronic infection in the United States. Recent price reductions for HCV treatments improve the outlook on affordability at the system level, as the $26,400-plus price tag still makes it inaccessible to individual Medicaid enrollees. Furthermore, the long-term costs of untreated HCV typically borne by Medicare are offset under this concept. The Maryland TCOC model gives Medicare the option of crediting Medicaid for spending money today that it will save on health care costs in the future. This is an approach to resolve the mismatch between investing today and getting future returns.
Is expanded coverage for hepatitis C cost effective?
Expanded coverage under a joint partnership by Medicare and Medicaid to treat all prevalent cases of hepatitis C virus (HCV) appears to be cost-effective by saving money and improving patient outcomes.
What is the primary analysis for this methodology study focused on?
The primary analysis for this methodology study focused on the changing costs and effectiveness estimates at each time point to estimate incremental cost-effectiveness ratios. A scenario analysis was conducted using only the WAC for each drug referenced in RED BOOK to describe the effect of using list versus net price in the CEA. 21
Is HCV treatment effective?
Treatment effectiveness for HCV has increased steadily, while treatment costs increased substantially from 2010-2014 before decreasing to its lowest point in 2018. The dynamic nature of CEAs in a disease state with rapid pharmaceutical innovation may cause some concern for decision makers who rely on a single analysis over time. Model transparency along with resources to update or revise model assumptions would enable organizations to provide more up-to-date results to inform formulary decisions.