Full Answer
How is warfarin initiated for VTE treatment?
During warfarin initiation for VTE treatment we suggest the following: 1 Initiate warfarin as soon as possible following diagnosis of VTE, preferably on the same day,... 2 The initial dose of warfarin should be 5 or 10 mg for most patients. 3 Beginning on day 3 of therapy, INRs should be measured daily and warfarin doses adjusted...
What is anticoagulant therapy for venous thromboembolism (VTE)?
Anticoagulant therapy is the mainstay for the treatment of venous thromboembolism (VTE). Once treatment is started, the question arises as to how long patients should be treated, which is the focus of this perspective.
Which anticoagulants are used in the treatment of von Willebrand disease (VTE)?
Based upon its pharmacokinetics, ability to be monitored, costs and other characteristics, warfarin may be the preferred anticoagulant for some patients and should be avoided in others. Kidney disease is a risk factor for VTE [ 12 ].
When was Warfarin first used?
Warfarin, its discoverer, and its original indication (warfarin, discovered by Link, was initially launched in 1948 as the ideal rodenticide, and was considered to be too toxic for human use) 43. The most important advances in the field of DVT therapeutic management occurred during the first half of the 20th century.
When was warfarin first used?
Warfarin first came into large-scale commercial use in 1948 as a rat poison. Warfarin was formally approved for human use by the U.S. Food and Drug Administration (FDA) to treat blood clots in 1954.
Can warfarin be used for VTE?
Furthermore, the duration of warfarin treatment is important to prevent recurrent venous thromboembolism (VTE) event, a challenge condition that may cause fatal outcome.
What was the first effective anticoagulant for the prevention and treatment of VTE?
Direct oral anticoagulants. Rivaroxaban is a direct factor Xa inhibitor and the first DOAC that was approved in 2012 for the treatment of VTE.
How long has warfarin been in use?
Warfarin is a blood thinner that has been used for more than 60 years to prevent the formation of clots and strokes. It is most commonly prescribed for people with atrial fibrillation, deep vein thrombosis, pulmonary embolism and prosthetic heart valves.
What is the first line treatment for DVT?
Use of direct oral anticoagulants (DOACs) are recommended as first-line treatment of acute DVT or PE. DOAC therapy is preferred over vitamin K antagonists (VKAs) for most patients without severe renal insufficiency (creatinine clearance <30 ml/min), moderate-severe liver disease, or antiphospholipid antibody syndrome.
What is the difference between warfarin and enoxaparin?
Enoxaparin, a low-molecular-weight heparin, has been shown to reduce the prevalence of deep venous thrombosis after total hip arthroplasty. Warfarin, an orally administered anticoagulant, has been used historically to reduce the risk of deep venous thrombosis after total hip arthroplasty.
What is the most common anticoagulant for DVT prophylaxis?
Apixaban. Apixaban is a direct factor Xa inhibitor that has been approved for VTE prophylaxis following THR and TKR, for the treatment of acute DVT or PE, and for risk reduction for recurrent DVT and PE after initial diagnosis and treatment.
Which anticoagulant is best for DVT?
Rivaroxaban (Xarelto) is an oral factor Xa inhibitor approved by the FDA in November 2012 for treatment of DVT or PE and for reduction of the risk of recurrent DVT and PE after initial treatment. Approval for this indication was based on studies totaling 9478 patients with DVT or PE.
Is heparin used for VTE?
Heparin in a fixed low dose of 5000 U SC every 8 or 12 hours is an effective and safe form of prophylaxis in medical and surgical patients at risk of venous thromboembolism. Low-dose heparin reduces the risk of venous thrombosis and fatal PE by 60% to 70%.
Why is warfarin no longer used?
Why Warfarin Is No Longer Recommended for AFib Treatment. New guidelines are recommending newer drugs due to concerns over potential severe bleeding from warfarin use. After a long run at the top, warfarin may be on the way out.
Why is warfarin called rat poison?
Warfarin is a synthetic derivative of dicoumarol, and since 1948 has had a major role in slaughtering rats and mice by stimulating internal bleeding. In 1954, warfarin was also approved for therapeutic use as an anticoagulant in the prevention of thrombosis and thromboembolism.
Why is warfarin being discontinued?
The most commonly reported reasons for warfarin discontinuation were physician preference (47.7%), patient refusal/preference (21.1%), bleeding event (20.2%), frequent falls/frailty (10.8%), high bleeding risk (9.8%), and patient inability to adhere to/monitor therapy (4.7%).
What is the standard of care for acute VTE?
Anticoagulant therapy is the standard of care in patients presenting with acute VTE. Inpatient treatment with IV UFH is being replaced by outpatient therapy with LMWH as the most commonly used anticoagulant regime. Following is a review of the efficacy, safety, and appropriate dosage of both UFH and LMWH.
What is heparin induced thrombocytopenia?
Heparin-induced thrombocytopenia (HIT) is a clinicopathological syndrome; 44 its diagnosis is based on characteristic clinical events and concurrent laboratory detection of HIT antibodies in the setting of recent heparin therapy. The pathogenic antibodies are directed against multimolecular complexes of platelet factor 4 (PF4) and heparin, and stimulated by neoepitopes expressed on PF4 in response to heparin binding. 44 Interaction of the antigen/antibody complex with platelets and binding of antibody to platelet Fc receptors result in platelet activation and aggregation. 45 The end result is increased thrombin generation, which may be associated with arterial or venous thrombosis. 44
Is Fondaparinux safe for DVT?
In phase III trials, fondaparinux has been found to be at least as effective and safe as IV UFH for initial treatment of PE 62 and as the LMWH enoxaparin for initial treatment of DVT. 64. Ximelagatran (Exanta) is an oral, direct thrombin inhibitor, which is metabolized to the active metabolite melagatran once absorbed.
Is heparin an anticoagulant?
Adequate initial anticoagulant therapy of deep venous thrombosis (DVT) is required to prevent thrombus growth and pulmonary embolism (PE). Intravenous unfractionated heparin (UFH) is being replaced by low-molecular-weight heparin (LMWH) as the anticoagulant of choice for initial treatment of venous thromboembolism (VTE). Both agents are relatively safe and effective when used to treat VTE, with LMWH suitable for outpatient therapy because of improved bioavailability and more predictable anticoagulant response. Serious potential complications of heparin therapy, such as heparin-induced thrombocytopenia (HIT) and osteoporosis, seem less common with LMWH. The potential for fetal harm and changes in maternal physiology complicate the treatment of VTE during pregnancy. Although systemic thrombolysis is used in patients with massive PE and in some patients with proximal DVT, controversy persists with respect to appropriate patient selection for this intervention.
Can Coumarin cause fetal bleeding?
Selection of optimum treatment for women in whom VTE develops during pregnancy must take into account alterations in maternal physiology and the potential for fetal harm. Coumarin derivatives cross the placenta and have the potential to cause fetal bleeding and teratogenicity. In contrast, neither UFH nor LMWH cross the placental barrier, 49 and despite recent precautions from pharmaceutical manufacturers about teratogenicity associated with LMWH, available data support the safety of UFH and LMWH for the developing fetus. 60 Evidence for the efficacy of this approach is extrapolated largely from trials in nonpregnant patients. Accordingly, either UFH or LMWH may be used for both initial treatment and secondary prophylaxis of VTE during pregnancy.
Is heparin induced thrombocytopenia common with LMWH?
Serious potential complications of heparin therapy, such as heparin-induced thrombocytopenia (HIT) and osteoporosis, seem less common with LMWH. The potential for fetal harm and changes in maternal physiology complicate the treatment of VTE during pregnancy.
Is LMWH an effective treatment for VTE?
Over the past decade, LMWH has emerged as an effective alternative to UFH as initial therapy for VTE. Outpatient therapy of VTE is now common, but because the index disorders may arise unpredictably, treatment is best managed under the direction of a team of specialists available around the clock. The emergence of novel antithrombotic agents that target specific factors in the coagulation cascade may modify the initial treatment of VTE in the near future. Further trials, both in selected high-risk subgroups and use of catheter-directed drug delivery, are needed to better define the role of thrombolytic therapy for VTE.
When was DVT first discovered?
Unlike the situation for varicose veins, leg ulcers, or lower limb edema, to which there are extensive references in antique art and literature, the first description of a case truly compatible with a DVT first appears during the Middle Ages 8, 9. In the manuscript of Guillaume de Saint Pathus entitled ‘La vie et les miracles de Saint Louis’, it is reported that, in 1271, Raoul, a 20-year-old Norman cobbler suffered unilateral pain and swelling of the right calf that subsequently extended up to the thigh (Fig. 1) 9. Raoul's surgeon, Henri de Perche, advised him to wait and see. Unfortunately, the patient's symptoms worsened, and he developed a leg ulcer. He visited St Eloi's shrine, without any improvement. After additional unsuccessful unspecified treatment attempts, Raoul was advised to visit the tomb of King Saint Louis. He spent several days praying to the saint, and then he decided to collect the dust that he found below the stone that covered the tomb, and he applied it directly to the ulcer. The story reports that he was miraculously healed after this direct application, and was still alive 11 years later. Thus, this first reported case of effective treatment of DVT might not be the most reproducible. In antiquity, neither famous Greek physicians such as Hippocrates and Oribasius, nor Roman physicians such as Galen or Caelius Aurelianus, reported a case suggesting a diagnosis of DVT; this is also true of the art of ancient Egypt, Persia, and South America. Nevertheless, it is likely that this disease is as old as humankind, and it may have affected famous historical figures: on the basis of writings from the New Testament, Brenner surmised that Jesus Christ himself may have suffered from a PE, but this hypothesis is debated 10 - 12. The oriental scientist Avicenna (980–1037) warned against the risk of ‘particle migration’ in cases of vein surgery, consistent with embolization of a DVT, but provided no formal description 13, 14. Thus, although venous thrombosis is a frequent disease, it appears that no cases clearly compatible with the diagnosis of DVT were reported before the description of the case of Raoul.
What was the first anticoagulant?
The first isolated anticoagulant was hirudin, obtained in 1884 by Haycraft 32. It was extracted from the saliva of leeches. However, it could not be used as a potent anticoagulant agent until its production by genetic engineering in 1986. Thus, the first anticoagulant that could be effectively used for the treatment of DVT was heparin. It was discovered in 1916 by McLean, at that time a medical student, while he was studying the procoagulant properties of crude ether and alcohol extracts of the brain, liver and heart under the supervision of Howell 37. Indeed, during World War I, scientists were more interested in the development of procoagulant than of anticoagulant substances 4. McLean noticed that these extracts, and more particularly heparphosphatide, became anticoagulant agents after long-term exposure to air 37. In 1918, Howell renamed heparphosphatide, which was a mixture of phospholipids, ‘heparin’ 3. Four years later, he discovered true heparin, a water-soluble mucopolysaccharide from dog liver. A dispute over the paternity of the discovery started between the two scientists. However, this dispute might well have been vain, as it emerged later that the anticoagulant isolated years earlier in 1911 by Doyon after peptone shock was, in fact, heparin 3 .
How long has DVT been around?
The history of DVT treatment started more than 700 years ago, and has involved medical and surgical treatments (Fig. 5 ). All major breakthroughs have been made during the last 100 years. During the first half of the last century, anticoagulants were discovered, shifting the issue from the fear of death to less severe and less frequent complications: VTE recurrence and major bleeding. The second half of the century was characterized by the simplification of anticoagulant treatment, which allowed ambulatory treatment of the disease and the end of the bed-rest dogma. Complementary treatments were developed, but have not provided sufficiently good results to justify their use in routine practice. The next steps in the improvement of DVT treatment will probably focus on decreasing DVT morbidity, such as PTS, for which therapeutic options are currently limited 87. New oral anticoagulants might have the potential to decrease this morbidity through safer and longer duration of treatment 88, 89. Another option under development is the use of microbubbles for safe early thrombus removal 90. Finally, the main treatments for atherothrombosis, antiplatelet agents and statins, could be used to reinforce the DVT therapeutic arsenal in the coming years. Indeed, both drugs have recently been demonstrated to prevent VTE effectively 91, 92. This is a therapeutic confirmation of the suspected pathophysiologic link between VTE and atherothombotic diseases 93. The numerous ongoing therapeutic trials assessing various promising potential treatments for DVT are clear evidence of the dynamism of venous thrombosis research.
What is the humoral theory of DVT?
From the 17th century, the humoral theory, which was previously used to explain DVT pathophysiology, was gradually abandoned. In 1676, Wiseman suggested that DVT was the consequence of an alteration of blood, and then, in 1793, Hunter hypothesized that it was an occlusion of the vein by blood clots 15.
What is DVT in medical terms?
Deep vein thrombosis (DVT) is a common disease. However, unlike that of varicose veins, which have been depicted since antiquity in art and literature, its description was more recent in the history of medicine. The first well-documented case of DVT was reported during the Middle Ages: in 1271, Raoul developed a unilateral edema in the ankle, which then extended to the leg. The number of reported DVT cases steadily increased thereafter, particularly in pregnant and postpartum women. During the first half of the 20th century, well before the discovery of anticoagulants, many therapeutic approaches were used, and arose from the pathologic hypotheses that prevailed at their time. Despite the development of anticoagulants, and the fact that they were thought to dramatically decrease DVT mortality, numerous complementary treatments have also been developed during the last 50 years: they include vena cava clips and surgical thrombectomy, and are intended to decrease mortality or to prevent late complications. Most of these treatments have now been abandoned, or even forgotten. In this review, we recall also the discovery and the use of vitamin K antagonists and heparin, which have constituted the mainstay of treatment for decades. We also bring some perspective to historical aspects of this disease and its treatment, notably regarding elastic compression and early mobilization, but also abandoned and complementary treatments. In these times of change regarding DVT treatment, mainly marked by the arrival of new oral anticoagulants, efforts of physicians through the ages to treat this common disease provide a beautiful example of the history of knowledge.
How long did heparin last?
The duration of heparin treatment varied between centers, but was usually 7–10 days 34, 42 . The introduction of oral vitamin K antagonists (VKAs) for this indication in 1941 allowed treatments to be prolonged 5 .
When were compression bandages used?
The use of compression therapy was reported during antiquity: Hippocrates, in his Corpus Hippocraticum (450–350 BC), prescribed compression bandages to treat leg ulcers 56. In his treatise entitled Chirurgica Magna, which remained a standard reference in Europe for almost four centuries, Guy de Chauliac, a French surgeon, recommended treating varicose veins with bandages 57. It is only from the late 19th century, after observing that superficial vein thromboses disappeared rapidly after application of compression bandages, that Fischer and Lasker, two German phlebologists, started prescribing compression bandages to their patients with DVT 57. However, the prolonged bed rest imposed on patients with DVT at that time prevented the diffusion of this approach to DVT treatment. Compression bandages started to be more widely used when anticoagulants became available. They were usually prescribed at the end of heparin treatment, once ambulation was authorized 42. A demonstration of their usefulness in preventing post-thrombotic syndrome (PTS) was provided by Brandjes in 1997 58 .
Sunday, October 5, 2014
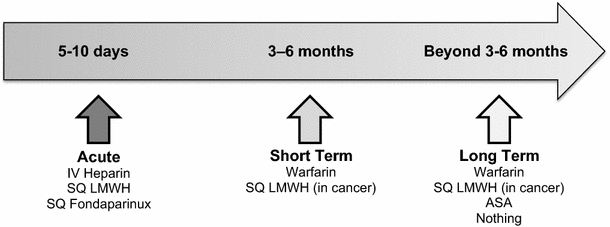
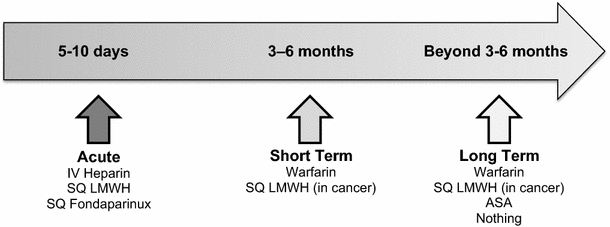
Given the rising number of options for treating venous thromboemboli (VTE), questions occasionally arise on what is the standard for initiating and continuing anticoagulation. Questions such as, "How long do we need to overlap parenteral anticoagulation for?" and "Can we begin monotherapy with a new oral anticoagulant?" will be discussed below.
Get the Vancomycin Dosing Calculator - A HughesMedicine App
Get the app to quickly determine an ideal vancomycin regimen, estimate a steady-state trough concentration, and adjust an existing regimen.
About Gregory Hughes
I write brief pharmacotherapy pearls for physicians, pharmacists, students, and anyone else who may find them useful.
How long are VTE patients followed?
No trial has randomized patients with VTE, with or without cancer, to stop or continue anticoagulants and then followed patients indefinitely (eg, for 10 or more years). Available studies anticoagulated all patients for 3 or 6 months, randomized half to stop and half to continue anticoagulants from that time point, and followed the 2 groups while the extended therapy group was being treated (ie, 1-4 years). If patients in the extended therapy group then stopped anticoagulants, which was often the case, they were not subsequently followed. The studies were heterogeneous with respect to: when randomization and follow-up started (at diagnosis or after the initial common period of treatment); study populations; type and intensity of anticoagulant; use of placebo; assessment of bleeding in the nonanticoagulated group, including if they had a recurrent VTE and restarted anticoagulants; and whether patients were followed for the same or for a variable length of time.
How long does it take for a VTE to stop?
The decision to stop anticoagulants at 3 months or to treat indefinitely is more finely balanced after a first unprovoked proximal DVT or pulmonary embolism (PE).
What are the factors that affect bleeding during anticoagulation?
Many factors are associated with bleeding during anticoagulant therapy including: older age (>65 years and particularly >75 years), previous bleeding (particularly if the cause was not correctable), cancer (particularly if metastatic or highly vascular), renal insufficiency, liver failure, diabetes, previous stroke, thrombocytopenia, anemia, concomitant antiplatelet therapy, recent surgery, frequent falls, alcohol abuse, reduced functional capacity, and poor control of VKA therapy. 1 With an increase in the severity of individual factors, and with the number of factors present, the risk of bleeding is expected to increase (both at baseline and while on anticoagulants). However, there are no validated prediction rules for bleeding during extended anticoagulation for VTE, and the rules that are available have demonstrated limited discriminatory capacity in VTE patients. 35, 36, 59 That, however, does not mean that it is impossible to stratify patients’ risk of bleeding; young (eg, <65 years) healthy patients with good VKA control will have a low risk of major bleeding (≤1% per patient-year), those with less severe factors have an intermediate risk, and elderly patients with severe or multiple factors are at high risk for major bleeding (>4% per patient-year). 1, 33, 59
What happens if you stop anticoagulant treatment?
If anticoagulants are stopped before active treatment is completed, the risk of recurrent VTE is higher than if treatment was stopped after its completion. 2, 3 The excess episodes are due to reactivation of the initial thrombus.
How long does it take to treat venous thromboembolism?
It takes about 3 months to complete “active treatment” of venous thromboembolism (VTE), with further treatment serving to prevent new episodes of thrombosis (“pure secondary prevention”). Consequently, VTE should generally be treated for either 3 months or indefinitely (exceptions will be described in the text).
What is anticoagulant therapy?
Anticoagulant therapy is the mainstay for the treatment of venous thromboembolism (VTE). Once treatment is started, the question arises as to how long patients should be treated, which is the focus of this perspective.
What is the most important consequence of a recurrent VTE or a major bleed?
The most important consequence of a recurrent VTE or a major bleed is that it may be fatal. In prospective studies, case fatality has been estimated as 3.6% for a recurrent VTE and 11.3% for a major bleed on a VKA. 26 There is uncertainty about these estimates.