
Maintenance programs for patients with dental implants are often not considered until restorative care is complete or until the patient has a maintenance issue. This is a mistake.
Full Answer
What to consider when planning an implant in the esthetic zone?
There are multiple variables that should be considered while planning an implant in the esthetic zone. These include, Emergence profile: The emergence profile refers to the portion of the prosthesis that allows the implant to turn into a natural-looking tooth.
How to make decisions about implant therapy?
Decisions have to be made regarding the treatment plan according to the patient’s clinical presentation, to deliver a prosthesis which is expected to last long and fulfills patient’s desires. The patient may be partially or fully edentulous. In both the cases, the basic principles of implant therapy have to be followed.
What are the general rules followed during implant placement?
The general rules followed during implant placement Following are the general principles followed during implant placement, The minimum distance between the implant margin to adjacent tooth should be 1.5 mm to 2 mm. The minimum distance between two implants should be 3 mm to 4 mm.
When should you consider dental implants?
If a hopeless or nonrestorable tooth is still present, but the site will receive an implant in the future, this should also be considered at this time. Alveolar Bone: It is important to ensure there is enough tridimensional bone to house the desired implant diameter and length.
What is required when you process an implant?
Because dental implants require one or more surgical procedures, you must have a thorough evaluation to prepare for the process, including a: Comprehensive dental exam. You may have dental X-rays and 3D images taken, and have models made of your teeth and jaw. Review of your medical history.
What is a contraindication for considering a patient for dental implants?
There are few absolute contraindications to dental implant placement. Relative contraindications include cognitive decline, American Society of Anesthesiology Patient Status IV or higher categories, or medical conditions that may jeopardize the life or lifespan of the patient.
What are the 3 components of a dental implant?
Implant Post, Abutments, Prosthesis Usually, conventional dental implants have a three-piece design. The three components are the implant post or screw, the abutment that attaches to the implant post, and the prosthesis or tooth restoration, which could be a crown, bridge, or denture.
When implants are not an option?
The medical case for dentures Implants need healthy jaws and gums to stay in place. The implant screw needs enough bone to hold onto, and the implant needs your gums to grow around the implant and offer additional support. If your jaw or gums are unhealthy or weak, implants may not be an option.
Are there any contraindications that should be reviewed with a patient before an implant is placed?
There are few absolute contraindications to dental implant placement. Relative contraindications include cognitive decline, American Society of Anesthesiology patient status IV or higher categories, or medical conditions that may jeopardize the life or lifespan of the patient.
What is contraindication in dentistry?
Spectrum of risk when considering placement of a dental implant. Contraindications are recognized as being either absolute or relative. An absolute contraindication indicates that the procedure could cause a life-threatening event or the risk of the procedure clearly outweighs any possible therapeutic benefit.
What dental implants include?
Dental implant systems consist of a dental implant body and dental implant abutment and may also include an abutment fixation screw. The dental implant body is surgically inserted in the jawbone in place of the tooth's root.
What are the different parts of an implant?
The Different Parts Of A Dental ImplantImplant Fixture. The foundation or base of a dental implant is the fixture. ... The Abutment. The abutment sits along the gum line and is the part of a dental implant that holds the replacement tooth in place. ... The Crown. The final component of a dental implant is the crown.
What are implant posts made of?
Titanium is one of the most widely used materials for dental implant posts. The titanium alloy material is very durable and can be trusted to last for years without becoming broken or damaged. Titanium posts are surgically placed inside the jaw and serve as the base for an artificial tooth.
Who should not get an implant?
Patients suffering from systemic diseases such as diabetes, Parkinson's disease, and certain autoimmune diseases are at greater risk of infection or implant complications. Osteoporosis, medications used for osteoporosis and other bone deterioration diseases, contribute greatly to implant complications as well.
What they don't tell you about dental implants?
Dental implants are secured permanently to your jawbone; hence, they can't fall off. The Procedure Is Quite Painless- Having titanium on your jawbone sounds painful; however, the procedure causes little pain. There is minimal post-operative pain, and you can go back to work in a relatively short time.
Why you should not get dental implants?
The risks and complications you are taking for dental implants include infection, damage to other teeth, delayed bone healing, nerve damage, prolonged bleeding, jaw fractures and more. If you are willing to take these risks, dental implants might be right for you.
What are the complications of implant surgery?
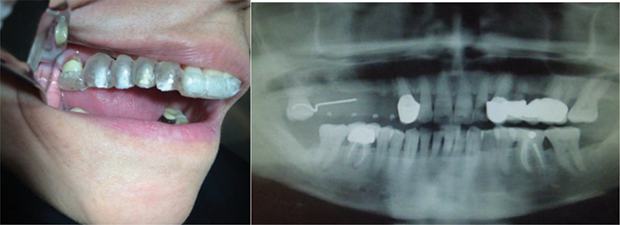
Biologic Complications can include soft tissue dehiscence, peri-implant bone loss (≥ 2 mm) following initial healing, peri-implant mucositis, inflammation under the fixed prosthesis, and hypertrophy/hyperplasia of soft tissue. 8 They are divided according to chronological criteria in early and late complications/failures. 9 Early implant complications/failures occur soon after placement of implants, leading to a failure in achieving osseointegration, which might indicate an interference with the initial bone healing process. Factors thought to contribute to early implant failures include (but are not limited to) poor bone quantity and quality, the patient’s general health condition, smoking, early infection, post-insertion pain, lack of primary stability, or inadequate surgical and prosthetic techniques. 9 On the other hand, late complications occur following a longer period after placement. These complications arise from pathologic processes after osseointegration is achieved. Most late complications fall within the categories of peri-im plant mucositis (Figures 1A and 1B) and peri-implantitis (Figures 2A and 2B). As an example, the most frequently reported biologic implant-related complications are both considered late complications. These include peri-implant mucositis (inflammation of the peri-implant tissues with no bone loss), followed by excessive peri-implant crestal bone loss/peri-implantitis. 10
What is the goal of dental implant risk assessment?
The main goals are to identify variables that increase the risk of complications leading to implant loss. It is a dynamic process in which risk will be assessed not only prior to dental implant treatment, but also during treatment, as well as after the implant is restored and functioning.
What is the ultimate determinant of dental implant success rates?
In the context of the individual treatment plan, the ultimate determinant of dental implant treatment success rates is the patient’s personal subjective criteria; therefore, realistic expectations should be determined and clarified at the beginning of treatment.
What are biological complications?
Biologic complications are disturbances in the implant function characterized by biological processes affecting the supporting peri-implant tissues, namely, early and late implant failures, and adverse reactions in the peri-implant hard and soft tissues.
Is there a risk of dental implant failure?
The risk of failures and complications is not evenly distributed among individuals seeking dental implant treatment. Many patients will have one or more risk factors, making them more susceptible to complications than those with no significant risk factors.
Why do dental implants have a larger diameter?
Most often, larger implants (and artificial abutments) are selected for the back part of the mouth due to the increased chewing forces (although this is not a general rule). The length and diameter of dental implants ultimately depends on the bone structure and the type of prosthesis that is planned. e.
Can bone be used for implants?
It is not uncommon that the size and/or structure of the bone is not adequate to support the designed implants. In this case, adjunctive surgical procedures are planned to increase the amount of bone (e.g bone graft, sinus lift ).
1. Introduction
One of the goals of a successful traditional dental practice has been the preservation and rehabilitation of a patient’s natural dentition. Endodontic treatment has played a key role in the retention and restoration of teeth affected by pulp and/or periapical pathosis. In earlier times, diseased teeth would invariably be extracted.
2. Factors influencing treatment planning
One of the most-often debated components of this implant or endodontics dilemma is whether endodontic treatment and restoration can compete with a dental implant-borne prosthesis in terms of survival rates and success.
3. Conclusion
When choosing the appropriate treatment for patients, it should be kept in mind that every patient and situation is unique. Specific patient and/or clinician factors weigh heavily in choosing whether to perform tooth preservation procedures or extraction procedures with the option of implant-supported restoration.

Biologic and Technical Complications
Risk Assessment
Pretreatment Comprehensive Examination
Chief Complaint
Extraoral and Intraoral Examination
Clinical Examination
Radiographic Examination
- The implant surgeon has to consider certain anatomic landmarks or conditions that may influence or determine implant placement, such as the inferior alveolar nerve, mental nerve, nasopalatine nerve, floor of the sinus, lingual concavities on the mandible, or simply inadequate bone dimensions for adequate implant placement (Figures 5A through 5D).31...
Diagnosis and Implant Planning
Conclusion
References