Should I start taking insulin if I have type 2 diabetes?
1. Guava...
2. Apples...
3. Cherries...
4. Grapefruit...
5. Gokhru...
6. Avocado...
7. Strawberries...
8. Oranges...
Learn More...When should you take insulin?
If you have type 2 diabetes, it is likely that your treatment regimen will change over time as your needs change, and at some point, your healthcare professional may suggest that you start taking insulin. While this might feel scary, there are millions of others living with type 2 diabetes and taking insulin, so it’s definitely manageable.
How many insulin injections should a diabetic have a day?
The decision to take insulin is never an easy one. For many patients, it comes after years of having type 2 diabetes and trying multiple weight-loss regimens, diets, and oral medications. For other patients, the decision to take insulin is made when blood glucose levels are simply too high to control with other drugs.
Does early insulin treatment reduce macrovascular risk in type 2 diabetes?
In patients with type 2 diabetes already using at least one daily insulin injection, the introduction of intensive insulin therapy with continuous subcutaneous insulin infusion resulted in comparable glycemic control, weight gain, and hypoglycemia risk as multiple daily injection therapy (52,53).
When should type 2 diabetes start insulin?
Insulin should be initiated when A1C is ≥7.0% after 2–3 months of dual oral therapy. The preferred regimen for insulin initiation in type 2 diabetes is once-daily basal insulin. In addition to timely initiation, rapid titration of the dose is indispensable for successful insulin therapy.
At what sugar level should you start taking insulin?
Insulin therapy will often need to be started if the initial fasting plasma glucose is greater than 250 or the HbA1c is greater than 10%.
When should I start insulin therapy?
The American College of Endocrinology and the American Association of Clinical Endocrinologists recommend initiation of insulin therapy in patients with type 2 diabetes and an initial A1C level greater than 9 percent, or if the diabetes is uncontrolled despite optimal oral glycemic therapy.
What are the indications for insulin therapy in type 2 diabetes?
Insulin therapy is indicated in patients with newly diagnosed diabetes and severe hyperglycemia (plasma glucose level greater than 250 mg per dL), recent significant weight loss, and ketonuria.
Should I take insulin if my blood sugar is 110?
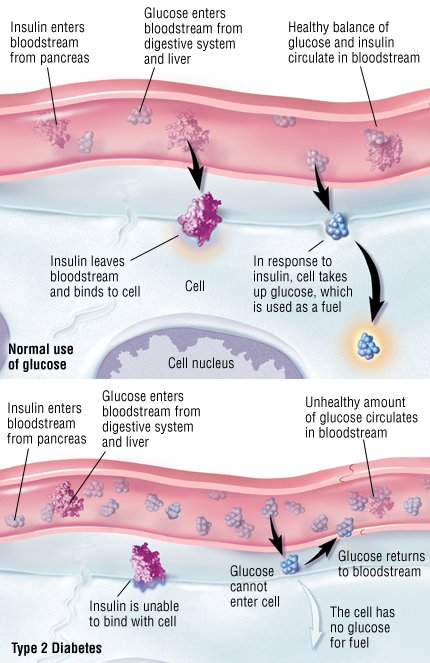
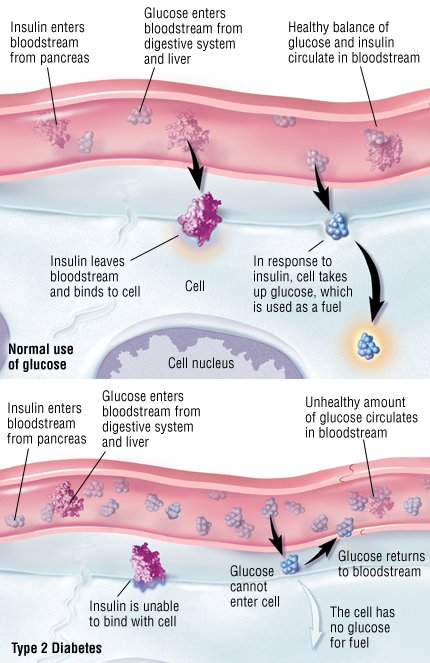
A fasting blood sugar between 110 and 125 would be considered in the “prediabetes” range. Less than 110 is normal and greater than 126 is diabetes. These abnormal blood sugar levels usually happen when a person's tissues don't respond well to a hormone [insulin] signal to take up sugar from the blood.
How do I know if I need insulin?
If your body doesn't make enough or any insulin, or if your cells resist the insulin your body makes, the glucose can't get into them and you have no energy. This can make you hungrier and more tired than usual. Peeing more often and being thirstier.
Is blood sugar of 7.8 high?
Less than 140 mg/dL (7.8 mmol/L) is normal. 140 to 199 mg/dL (7.8 mmol/L and 11.0 mmol/L) is diagnosed as prediabetes. 200 mg/dL (11.1 mmol/L) or higher after two hours suggests diabetes.
Do all type 2 diabetes need insulin?
“Someone with Type 1 diabetes will always require insulin injections, because their body produces little or no insulin, but someone with Type 2 diabetes may require insulin injections as part of their treatment plan as well,” said Eileen Labadie, Henry Ford Health diabetes education specialist.
Should I take my insulin if my blood sugar is normal?
Ultimately, there is no single, right answer to the question of whether to take your insulin if your sugars are low. So much depends on the follow-up questions posed above. Experience is the best predictor of the correct response.
What percentage of type 2 diabetes use insulin?
Historically, 30% or more of people with type 2 diabetes required insulin therapy. However there are many new drugs available that may delay or prevent the need for insulin therapy. It is expected that fewer and fewer individuals will need insulin replacement to control their blood sugars.
When do people with type 2 diabetes start insulin?
After 10 to 20 years, many people with type 2 diabetes will begin insulin therapy, although every person’s journey with type 2 diabetes is different. This happens when lifestyle changes and medications aren’t keeping your glucose levels in your target range. It is important that you start treatment as early as possible to avoid persistent hyperglycemia (high blood sugar), which can lead to long-term health complications affecting your heart, kidneys, eyes, and other organs.
How do I take and adjust my insulin doses?
There are several ways to take insulin – syringe, pen, pump, or inhalation – though injection with a syringe is currently the most common for people with type 2 diabetes. There are many apps that can help you calculate your insulin doses.
What are the different types of insulin?
The key to transitioning to insulin is knowing your options. Some people taking insulin need to use both a basal (long-acting) and a prandial (rapid-acting or “mealtime”) insulin each day, while others may only need to use basal insulin. Learn about your options here.
How often should I test my blood sugar?
Initially, you may be advised to check your blood glucose three to four times a day. As a starting point, check in with your healthcare team about how often to check your blood sugar. Many people test before meals, exercise, bedtime, and one to two hours after meals to ensure that they bolused their insulin correctly. Over time, your fasting, pre-meal, and post-meal blood glucose levels will help you figure out how to adjust your insulin doses.
What else do I need to know about taking insulin?
It’s common to experience minimal discomfort from needle injections or skin changes at the insulin injection site. You may also experience side effects of insulin therapy, which can include some weight gain and hypoglycemia. In some people, insulin increases appetite and stops the loss of glucose (and calories) in the urine, which can lead to weight gain. Hypoglycemia can occur if you are not taking the right amount of insulin to cover your carb intake, over-correcting high glucose levels, exercising, or consuming alcohol. Treating hypoglycemia also adds more calories to your daily intake and can further contribute to weight gain. Contact your healthcare professional to adjust your insulin dose if you are experiencing hypoglycemia, or call 911 if you experience more serious side effects, such as severe low blood sugar levels, serious allergic reactions, swelling, or shortness of breath.
What is the difference between prandial and ultra-rapid insulin?
Prandial (rapid-acting or “mealtime”) insulins are taken before mealtime and act quickly to cover carbohydrates eaten and bring down high sugar levels following meals. Ultra-rapid-acting prandial insulins can act even more rapidly in the body to bring down glucose levels. Rapid and ultra-rapid insulins are also taken to correct high glucose levels when they occur or are still persistent a few hours after a meal.
What is inhaled insulin?
Inhaled insulin is ultra-rapid acting insulin and can replace insulin used for mealtime and corrections of high glucose. It is taken through an inhaler and works similarly to injected prandial insulin. People with diabetes who do not want to inject prandial insulin might use this, but it’s not for people who only use basal insulin. The only approved inhaled insulin on the market is the ultra-rapid-acting mealtime insulin Afrezza.
What are the benefits of insulin injections?
Insulin is a stronger medication for lowering blood glucose levels and can help with the following aspects: Decrease the effects of symptoms of high blood sugar , such as fatigue and frequent need to urinate. Reduce the risk of developing diabetic complications. Decrease pressure on the pancreas to produce insulin.
Why do people need to test their blood sugar?
People starting insulin therapy may need to regularly test their blood sugar levels to monitor the effect that insulin is having and to help prevent low glucose levels (hypoglycemia) from happening.
What are the disadvantages of insulin?
Disadvantages of being on insulin injections 1 Raises the risk of hypoglycemia 2 Can promote weight gain 3 Some people may be uncomfortable about injecting 4 Could affect employment if you drive for a living
How many injections a day?
A number of different injection regimes are available, ranging from one injection a day to multiple injections a day. Your health team will be able to help you to choose an injection regime that best fits in with your lifestyle.
Does insulin injection cause weight gain?
Raises the risk of hypoglycemia. Can promote weight gain. Some people may be uncomfortable about injecting. Could affect employment if you drive for a living. The needles used for insulin injections are very slim and many people who start injections are surprised by how painless the needles are.
Can insulin cause hypoglycemia?
Insulin therapy and hypoglycemia. Insulin is a powerful medication for lowering blood glucose levels and can cause blood glucose levels to go too low if too much insulin is taken. Your health team should advise you on how to spot and treat hypos and how to avoid hypos from occuring.
Treatment Delays and Barriers
Patient and clinician factors contribute to delays in adding insulin to treatment regimens or in transitioning from oral antidiabetic agents (OADs) to insulin.
Advanced Basal Insulin Analogs and Fixed-Ratio Combinations
Advanced insulin analogs and pre-filled pen delivery devices are helping to overcome some of the barriers to insulin initiation and titration experienced by some patients and PCPs.
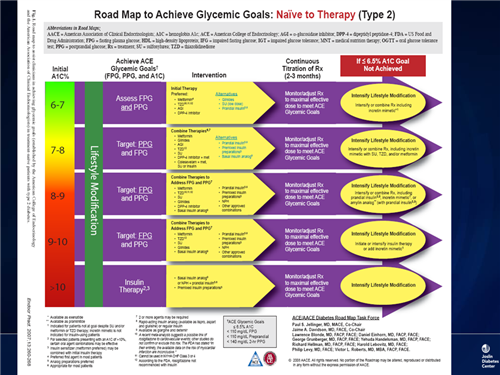
Current Guidelines for Insulin Initiation and Titration
The American Diabetes Association (ADA) recommends initiation of basal insulin at 10 units/day or 0.1–0.2 units/kg/day, adjusted by 10–15% or 2–4 units once or twice weekly to reach a target fasting plasma glucose (FPG) in patients whose A1C remains uncontrolled after >3 months of triple combination therapy, whose A1C is >10%, whose blood glucose is >300 mg/dL, or who are symptomatic of hyperglycemia ( 37 ).
Insulin Titration Algorithms
A number of titration algorithms have been evaluated that aim to simplify insulin titration and enable patient empowerment through self-titration to effectively participate in the management of their disease ( 4, 39 – 42 ), the details of which are summarized in Table 1.
When Too Much Insulin Has Little Effect on Glycemic Target
Current use of basal insulin has been shaped by treat-to-target trials that have emphasized systematically titrating the insulin dose without limit until an FPG of 100–130 mg/dL is reached ( 50 ). “Overbasalization” is said to occur when FPG is uncontrolled despite uptitration of basal insulin and the A1C target remains unmet ( 51 ).
Managing Insulin Regimens in the Primary Care Setting
It is important to gain an understanding of a patient’s background and lifestyle before initiating insulin to ensure that the treatment regimen takes into account the patient’s needs and preferences as well as clinical characteristics ( 37, 56, 57 ).
Conclusion
Multiple insulin algorithms have been developed to help PCPs with insulin initiation and titration and to enable patient self-management.
You don't understand what you've done wrong
Diabetes usually progresses over time. There comes a time when more and stronger treatment is needed. When the pills that have controlled your blood glucose no longer work, insulin is needed. This doesn't mean you have failed. It is expected in the course of the disease.
You feel isolated
You are not alone! Most healthy patients with diabetes can expect to live long lives after their disease is diagnosed. A large number will require insulin at some point. Many are not happy about taking injections, but most adjust to them well.
You feel like your life is going to change
In some cases, insulin treatment may be temporary. In others, it is not. Whatever is needed to control your blood glucose should be used. That's what keeps you healthy.
You've heard that insulin causes blindness and kidney failure
Nothing could be further from the truth. High blood glucose cause blindness, kidney failure, and other problems, such as nerve damage that can lead to amputations. But eye, kidney, and nerve damage can be delayed or prevented by good control. Insulin will NOT make your diabetes worse, and it is one of the most natural diabetes treatments available.
You're afraid to take injections or worried about a complicated insulin routine
Insulin needles today are so small and thin that patients barely feel them. And most starting insulin routines are fairly simple. Your provider may even be able to prescribe an insulin pen device, which makes injections even easier.
You're afraid injections will hurt or that you'll have low blood glucose reactions (hypoglycemia)
Most patients find that insulin shots don't hurt. Severe hypoglycemia is far more common in people with type 1 diabetes. Mild hypoglycemia may sometimes occur in patients with type 2 diabetes, but your provider will teach you how to detect, prevent, and treat it.
When to add prandial insulin?
Insulin could be added before breakfast if the pre-lunch glucose level is elevated, or before lunch if the dinner-time blood glucose level is elevated, or before dinner if the bedtime blood glucose level is el-evated—or a combination of these. Prandial insulin can be started at a low dose (4–6 units) and increased gradually.
What is the best insulin to treat postprandial hypoglycemia?
Rapid-acting insulin analogues (lispro, aspart, and glulisine) control postprandial glucose levels better than regular insulin and cause less hypoglycemia. Their pharmacokinetics enable them to be taken within a few minutes of the start of a meal, or even after the meal if the patient forgets to take an injection before the meal.
Can you take glargine twice a day?
Most often, glargine or detemir (Levemir) in-sulin is used. Detemir can also be given twice daily if needed. If cost is a concern, neutral protamine Hagedorn (NPH, Humulin N, Novolin N) insulin once daily at bedtime or twice daily is a reasonable alternative.
Should insulin be re-evaluated?
The insulin regimen should be re-evaluated routinely. It might need to be changed in re-sponse to the dynamic multifactorial process of progression of diabetes, change in stress level,presence or resolution of intercurrent illnesses, risk of hypoglycemia, concerns about weight gain, and cost.
Is insulin analogue safer?
Newer insulin analogues makeinsulin treat-ment safer and more accepted by patients. The availability of several options for insulin regimens allows individualization of the treat-ment according to the patient’s acceptance, the safety profile, and the cost.
Why do people take insulin?
For other patients, the decision to take insulin is made when blood glucose levels are simply too high to control with other drugs.
Who can teach you how to measure insulin?
If your health care provider prescribes insulin, a trained diabetes educator or pharmacist can teach you how to measure out the proper dose and administer your daily injections.
Does insulin work?
The good news is that insulin almost always works . Daily injections, however inconvenient or painful at first, can be very effective at controlling blood glucose. Anxious about giving injections? Help is available. If your health care provider prescribes insulin, a trained diabetes educator or pharmacist can teach you how to measure out the proper dose and administer your daily injections.
Can you have high blood glucose if you take other medications?
You often experience thirstiness, frequent urination, or other symptoms of high blood glucose despite taking other medications.
Can insulin be used for type 2 diabetes?
Injectable insulin is identical to the insulin made by the body , but can be categorized into two main types: basal insulin (long-acting and intermediate-acting insulin) keeps your blood glucose stable all day long, even when not eating, while bolus insulin (rapid-acting and short-acting insulin) helps your body respond to the quick rise in blood glucose after meals.