Nutrition
It may also be possible to change TB medications if your side effects are serious. If you are taking TB medicine on your own, it's important to get into a routine. Here are some ways to help you remember to take your TB medicine: Take your medicine at the same time every day.
Can I Change my TB medicine if I want to?
With the recent advances in TB treatment and diagnostics, and many ongoing trials, the next five years will likely see major changes to TB treatment approaches. However, the future trend is clear and is already arriving for drug resistant TB—shorter, all oral regimens incorporating newer drugs.
What will TB treatment look like in the next 5 years?
If you are having TB treatment (sometimes known as antitubercular treatment or ATT), then this should always be supervised by an experienced doctor or other health person. A patient must take their drugs properly.
Who can supervise me when I am having TB treatment?
To decide what treatment patients need, the World Health Organisation (WHO) used to put patients into TB treatment categories. But with the increasing availability of drug susceptibility testing (DST), treatment categories were abolished, and DST is now used instead to decide on the treatment that patients need.
How does the World Health Organisation decide what TB treatment patients need?
When should you restart TB treatment?
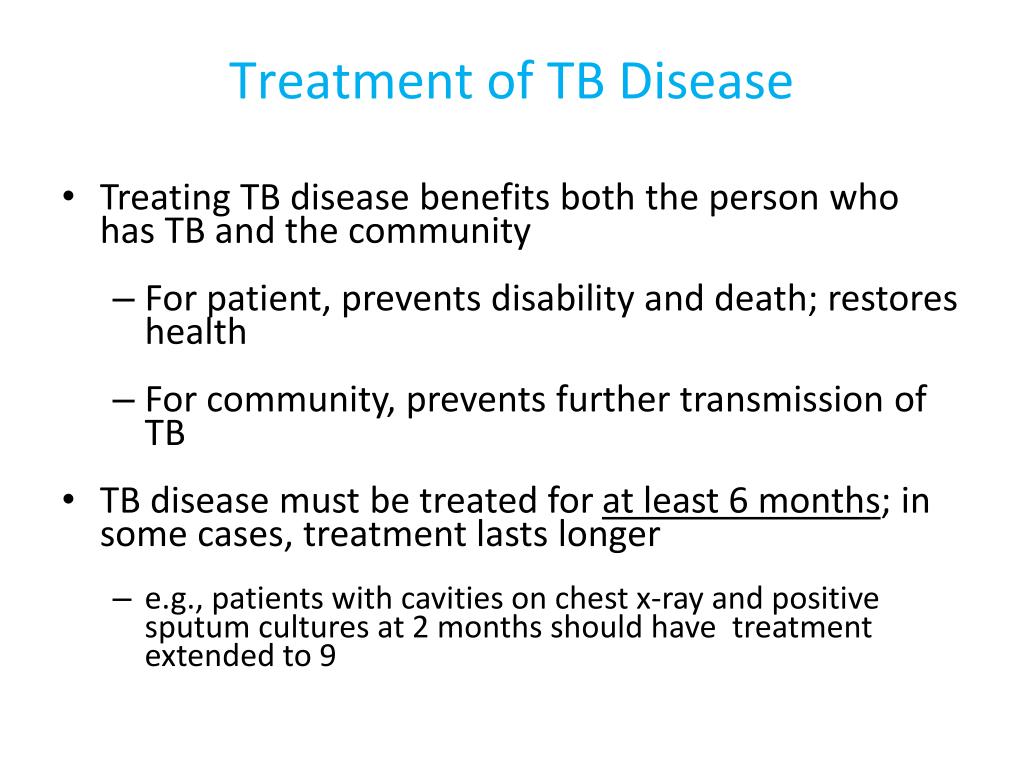
RIPE regimens for treating TB disease have an intensive phase of 2 months, followed by a continuation phase of either 4 or 7 months (total of 6 to 9 months for treatment). This is the preferred regimen for patients with newly diagnosed pulmonary TB.
When should TB treatment be stopped?
After taking antibiotics for 2 weeks, most people are no longer infectious and feel better. However, it's important to continue taking your medicine exactly as prescribed and to complete the whole course of antibiotics. Taking medication for 6 months is the best way to ensure the TB bacteria are killed.
How do you know if TB treatment is successful?
Physical signs of tuberculosis treatment success include:A reduction in symptoms, such as less coughing.Overall improvement in the way one feels.Weight gain.Increased appetite.Improvement in strength and stamina.
How long does active TB treatment last?
For active tuberculosis, you must take antibiotics for at least six to nine months. The exact drugs and length of treatment depend on your age, overall health, possible drug resistance and where the infection is in your body.
Why do TB patients stop their medication early?
The main reason treatments fail is that people do not take their medications properly. Medicines given to people with TB disease usually stop them from spreading TB bacteria within a few weeks. Most TB patients live at home and can continue normal activities if they take their medicine.
Who new TB treatment guidelines?
The new WHO 2022 guidelines evaluated the following new regimens: 1) the 6-month regimen based on bedaquiline, pretomanid and linezolid (BPaL) in combination with moxifloxacin (BPaLM), evaluated in the TB-PRACTECAL randomised clinical trial; 2) the 6-month regimens based on the BPaL combination with decreased exposure ...
How do you know if TB treatment is not working?
After taking TB medicine for several weeks, a doctor will be able to tell TB patients when they are no longer able to spread TB germs to others. Most people with TB disease will need to take TB medicine for at least 6 months to be cured.
What happens after finishing TB treatment?
Once your course of treatment is finished, you may have tests to make sure you are clear of TB. You might need more treatment if tests show there is still TB bacteria in your body, but most people will get the all-clear. Your treatment will not be stopped until you are cured.
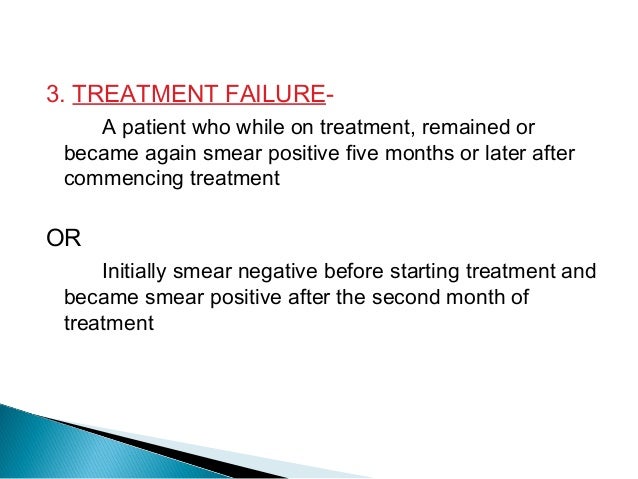
What makes TB treatment failure?
Some of the factors associated with treatment failure include poor drug compliance, primary drug-resistant TB, lack of efficacious anti-TB drugs, and presence of comorbidities such as HIV infection and diabetes mellitus.
Can tuberculosis come back after treatment?
A recurrence of TB can be due to relapse or re-infection [1]. To prevent relapse, TB treatment guidelines in the United States (U.S.) recommend extended treatment for TB cases with cavities on chest radiograph and delayed bacterial clearance from sputum [2]. Re-infection is prevented when TB transmission is averted.
Will I always test positive for TB after treatment?
Yes, this is true. Even after you finish taking all of your TB medicine, your TB skin test or TB blood test will still be positive.
When does TB cough stop?
Symptoms of tuberculosis Usually TB affects the lungs. The symptoms of active TB in the lungs include: Bad cough that lasts 3 weeks or longer. Coughing up blood or sputum (mucus from deep inside the lungs)
Where is TB common?
From countries where TB is common, including Mexico, the Philippines, Vietnam, India, China, Haiti, and Guatemala, or other countries with high rates of TB. (Of note, people born in Canada, Australia, New Zealand, or Western and Northern European countries are not considered at high risk for TB infection, unless they spent time in a country ...
Why is latent TB important?
Treatment of latent TB infection is essential to controlling TB in the United States because it substantially reduces the risk that latent TB infection will progress to TB disease.
How many people have latent TB?
In the United States, up to 13 million people may have latent TB infection. Without treatment, on average 1 in 10 people with latent TB infection will get sick with TB disease in the future. The risk is higher for people with HIV, diabetes, or other conditions that affect the immune system.
What is a TST reaction?
People with a tuberculin skin test (TST) reaction of 5 or more millimeters who are: HIV-infected persons. Recent contacts to a patient with active TB disease. Persons with fibrotic changes on chest radiograph consistent with old TB. Organ transplant recipients.
Can TB be treated with LTBI?
Persons with no known risk factors for TB may be considered for treatment of LTBI if they have either a positive IGRA result or if their reaction to the TST is 15 mm or larger. However, targeted TB testing programs should only be conducted among high-risk groups.
Can TB spread to others?
People with latent TB infection do not have symptoms, and they cannot spread TB bacteria to others. However, if latent TB bacteria become active in the body and multiply, the person will go from having latent TB infection to being sick with TB disease.
Is TB a serious disease?
TB is a serious disease, and can be fatal if not treated properly. It is important to remember that all medications have risks and benefits. Learn more from CDC’s Dear Colleague letter. Not everyone infected with TB bacteria becomes sick. As a result, two TB-related conditions exist: latent TB infection and TB disease.
Can rifampin be used for TB?
Treatment. impurities in rifampin and rifapentine, two important anti-tuberculosis (TB) medications. People with TB disease or latent TB infection taking rifampin or rifapentine should continue taking their current medication, and should talk with their healthcare provider about any concerns.
How long does it take to treat TB?
The treatment for this type of TB takes much longer, 20 to 30 months to complete, and you may experience more side effects.
What is the best treatment for TB?
The most common treatment for active TB is isoniazid INH in combination with three other drugs—rifampin, pyrazinamide and ethambutol. You may begin to feel better only a few weeks after starting to take the drugs but treating TB takes much longer than other bacterial infections.
What are the side effects of TB?
While you are in treatment for active TB disease, you will need regular checkups to make sure your treatment is working. Everyone is different, but there are side effects associated with taking the medications, including: 1 Upset stomach, nausea and vomiting or loss of appetite 2 Tingling or numbness in the hands or feet 3 Itchy skin, rashes or bruising 4 Changes in your eyesight or blurred visions 5 Yellowish skin or eyes 6 Dark-colored urine 7 Weakness, fatigue or fever that for three or more days
What are the symptoms of TB?
Yellowish skin or eyes. Dark-colored urine. Weakness, fatigue or fever that for three or more days. It is important to tell your doctor or TB nurse immediately if you begin having any unusual symptoms while taking medicine for either preventive therapy or for active TB disease.
Can TB cause liver damage?
TB drugs can be toxic to your liver, and your side effects may be a warning sign of liver damage . If you are having trouble with tingling and numbness, your doctor may prescribe a vitamin B6 supplement while you are in treatment. It may also be possible to change TB medications if your side effects are serious.
Can you get TB from taking too much medicine?
You must finish your medicine and take the drugs exactly as prescribed. If you stop taking the drugs too soon you can become sick again and potentially spread the disease to others. Additionally, by taking the drugs incorrectly, TB germs that are still alive may become drug-resistant, making it harder for you to get better next time.
How long does TB treatment last?
For new patients with presumed drug susceptible pulmonary TB, the World Health Organisation (WHO) recommends that they should have six months of treatment. This consists of a two month intensive phase followed by a four month continuation phase.
When should a TB smear be performed?
The recommendation from WHO is that for smear positive TB patients treated with first line drugs, the patients should have smear microscopy performed at the end of the two month intensive phase of treatment .
What are the best drugs for TB?
The drugs that a patient should take depends on whether the patient has ever had TB treatment before. If the patient has never had treatment before then it can be assumed that the bacteria in the patient's body will respond, and be sensitive to all the TB drugs. So the patient can then be given the following drugs: 1 Isoniazid 2 Rifampicin 3 Pyyrazinamide 4 & Ethambutol.
Why does TB treatment fail?
It is often suggested that TB treatment fails because a patient doesn’t take their TB drugs correctly. However there can be a number of different reasons for TB treatment failure. It is certainly true that if a patient doesn’t take their TB drugs properly that this can lead to the development of drug resistant TB.
What is the responsibility of a doctor for TB?
A patient must take their drugs properly. But it is also the responsibility of the doctor to make sure that the patient has the correct drugs. The doctor must also explain to the patient how to take the drugs correctly. In many countries there are "alternative" medicines available.
How many drugs are there for TB?
There are more than twenty drugs available for TB treatment. Which ones have to be taken depends on the circumstances of the patient. If you are having TB treatment (sometimes known as antitubercular treatment or ATT), then this should always be supervised by an experienced doctor or other health person.
What happens if you take only one or two TB drugs?
If only one or two TB drugs are taken then only some of the bacteria may be killed. They may then become resistant to the TB drugs which then don't work. If the person becomes sick again then different TB drugs called second line drugs may be needed.
Treatment
What You Need to Know About Your Medicine for Latent Tuberculosis (TB) Infection-Fact Sheet Series
Treatment for Latent TB Infection
What You Need to Know About Your Medicine for Latent Tuberculosis (TB) Infection-Fact Sheet Series
How long does it take to treat TB?
The current poor global control of TB is due in part to the lack of research innovation over the past few decades; current DS-TB treatment guidelines have been essentially unchanged for 35 years and treatment still takes a minimum six months.
How many people have TB in the world?
According to WHO estimates, in 2018 10 million people developed TB globally, for an incidence of 132/100 000 people. This global average, however, hides the vast disparities between developed and developing countries. Almost all cases are concentrated in South East Asia (44%), Africa (24%), and the western Pacific (18%) regions.
Is TB latent or active?
While TB treatment and control efforts are currently dichotomized around “latent” and “active” TB infection, neither of the two available methods to identify latent TB infection (tuberculin skin test and interferon gamma release assays) distinguish the few asymptomatic individuals who will develop active TB (estimated to be 5-10% lifetime risk) from the majority of individuals who will never develop active TB. Treating all M tuberculosis latently infected individuals for months is not feasible in most areas of the world. Rather, evidence is emerging of a spectrum of TB disease activity, and new approaches attempt to predict asymptomatic individuals who will progress to active TB disease (incipient TB infection).
Does XDR-TB have a control arm?
Of the three XDR-TB trials, however, only endTB-Q has a concurrent WHO standard control arm. Both Nix-TB and ZeNix only include experimental arms with no concurrent SOC control arm, with the primary outcome being relapse or failure at 12 months after enrollment.
Is DS TB decreasing?
Although global rates of DS-TB are slowly decreasing, rates of MDR-TB are decreasing less quickly, affecting 3.4% of new TB cases and 18% of previously treated cases. Even more challenging to treat is XDR-TB: MDR-TB with additional resistance to fluoroquinolones and injectable aminoglycosides.
Can you treat tuberculosis for months?
Treating all M tuberculosis latently infected individuals for months is not feasible in most areas of the world. Rather, evidence is emerging of a spectrum of TB disease activity, and new approaches attempt to predict asymptomatic individuals who will progress to active TB disease (incipient TB infection).