
Explore
Ensure your treatment plan for non-small cell lung cancer (NSCLC) is working. Read about treatment options, drug trials, alternative therapies, and what to ask your doctor.
Is NSCLC treatable?
Apr 02, 2019 · Each chemo cycle lasts for three to four weeks. If you have late-stage cancer, you’ll get about four to six cycles of chemo. 3. Radiation treatment is five days a …
What is the survival rate of NSCLC?
Dec 10, 2021 · Nearly two-thirds of people with early-stage lung cancer survive at least 5 years. Advanced NSCLC has a lower survival rate. If the cancer has spread to nearby tissues, the chance of surviving at ...
What is the prognosis of advanced NSCLC with met exon 14 alterations?
Jul 10, 2013 · In advanced stage IIIB/IV or inoperable NSCLC pts, a multidisciplinary treatment should be offered consisted of 4 cycles of cisplatin-based chemotherapy plus a 3 rd generation cytotoxic agent or a cytostatic (anti-EGFR, anti-VEGFR) drug. KEY WORDS : Non-small cell lung cancer (NSCLC), lung cancer, treatment, targeted treatment.
When is surgical resection indicated in the treatment of non-small cell lymphoma (NSCLC)?
Mar 08, 2018 · Results. Among 936 advanced NSCLC patients treated with systemic chemotherapy, 19 patients had N0–1 BOM at presentation. The median overall survival (OS) period of the N0–1 BOM patients was 16.0 months (95% CI, 11.8–20.2 months), while that of the N2–3 BOM + non-BOM patients was 14.5 months (95% CI, 13.2–15.8 months), compared with …
How long can you live with NSCLC without treatment?
What happens when a cancer patient stops treatment?
How long can a person live with Stage 4 NSCLC?
How fast does lung cancer spread without treatment?
When do oncologists stop chemo?
When should cancer treatment be stopped?
How long can immunotherapy keep you alive?
How long can you live with stage 4 adenocarcinoma?
...
What are the survival rates for stage 4 lung cancer?
| Stage | 5-year survival rate |
|---|---|
| all stages combined for non-small cell lung cancer | 25 percent |
What are immunotherapy treatments?
How long can you live with incurable lung cancer?
What are the last stages of lung cancer before death?
- shortness of breath.
- pain.
- cough.
- trouble focusing.
- confusion.
- extreme weakness and tiredness.
- little interest in eating or drinking.
- restlessness.
How often does lung cancer spread to the brain?
What is the best treatment for NSCLC?
Radiation uses high-energy waves to kill cancer cells. It’s sometimes the main treatment for people with NSCLC who can’t have surgery. Radiation is also given before surgery to shrink the tumor, or after surgery to remove any cancer cells that were left behind.
What is the treatment for stage 4 NSCLC?
Treatments include surgery, chemotherapy, radiation, targeted drugs, and immunotherapy.
What percentage of lung cancer is squamous cell carcinoma?
It makes up 40 percent of all lung cancers. This cancer starts in mucus-releasing cells in the lungs. Squamous cell carcinoma accounts for 25 to 30 percent of lung cancers. It grows from thin, flat cells that line the airways. Large cell carcinoma makes up 10 to 15 percent of lung cancers.
How many percent of lung cancer is large cell carcinoma?
Large cell carcinoma makes up 10 to 15 percent of lung cancers. It gets its name from the large size of the cancer cells when viewed under a microscope. This type of NSCLC tends to grow quickly. The stage of your cancer is also important.
How long does chemo last?
You’ll get the drug for one to three days and then stop for a few days to give your body time to recover. Each chemo cycle lasts for three to four weeks.
How many cycles of chemo for NSCLC?
If you have late-stage cancer, you’ll get about four to six cycles of chemo. 3. Radiation treatment is five days a week. Radiation uses high-energy waves to kill cancer cells. It’s sometimes the main treatment for people with NSCLC who can’t have surgery.
How long does it take to get a radiation treatment?
You’ll get radiation treatments five days a week for five to seven weeks. Each treatment only takes a few minutes. Stereotactic body radiation therapy (SBRT) speeds the process. Instead of small doses of radiation over several days, you get a very focused, higher dose. SBRT takes one to five sessions.
How long does lung cancer last?
Survival rates for cancers like non-small cell lung cancer are based on the five-year survival rate. The survival rate is calculated from the percentage of people who survive 5 years or longer after diagnosis.
What is non small cell lung cancer?
Non-small cell lung carcinoma is a type of lung cancer, also commonly referred to as non-small cell lung cancer (NSCLC). NSCLC can cause breathing difficulties and ultimately cause health complications. If diagnosed late or left untreated, it can be life threatening. Non-small cell lung carcinoma occurs when healthy cells form atypically ...
How do you know if you have lung cancer?
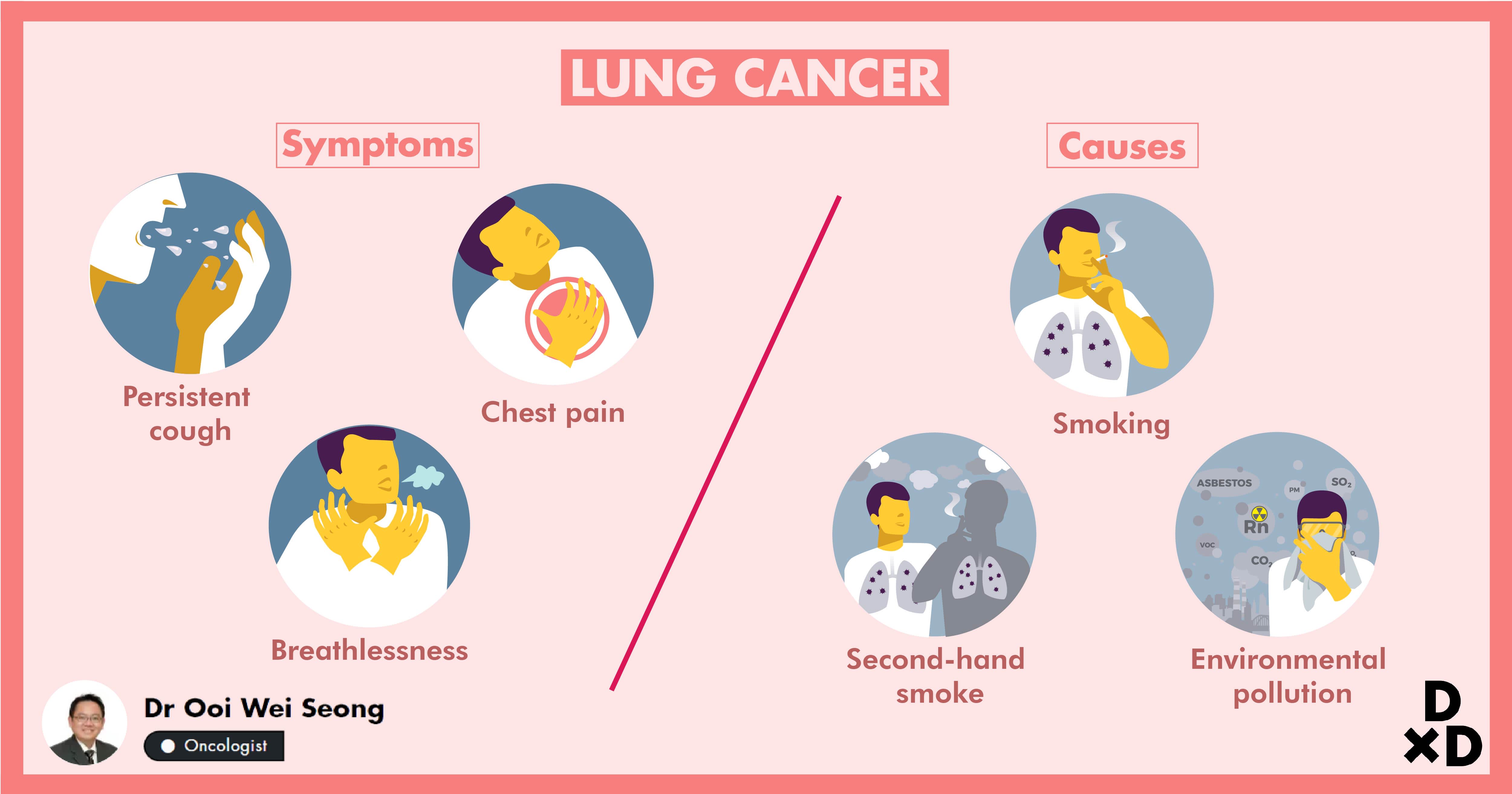
In its early stages, non-small cell lung cancer usually doesn’t cause any symptoms. Contact your doctor promptly if you experience symptoms of lung cancer, including: 1 recurrent cough 2 shortness of breath 3 chest pain 4 coughing up blood 5 unintentional weight loss
What are the different types of lung cancer?
There are three main subtypes of non-small cell lung cancer: 1 adenocarcinoma: starts in the outer part of your lungs 2 squamous cell carcinoma: starts in the middle portion of your lungs 3 undifferentiated carcinoma: starts in any portion of your lungs and involves fast-growing cells
Where does squamous cell carcinoma start?
squamous cell carcinoma: starts in the middle portion of your lungs. undifferentiated carcinoma: starts in any portion of your lungs and involves fast-growing cells. Adenocarcinoma is the most common type of lung cancer seen in nonsmokers. This subtype is more common in women than in men, and more common in younger individuals.
Can lung cancer spread to other parts of the body?
One danger of this cancer is that there’s a high likelihood that the cancer cells will spread from your lungs to other body parts.
Can lung cancer cause shortness of breath?
In its early stages, non-small cell lung cancer usually doesn’t cause any symptoms. Contact your doctor promptly if you experience symptoms of lung cancer, including: recurrent cough. shortness of breath. chest pain.
How many people will die from lung cancer in 2020?
Approximately 247,270 new cases of lung cancer are estimated to occur in 2020, with 130,340 male cases and 116,930 female cases [1]. Prior studies have reported that lung cancer resulted in more deaths than breast cancer, prostate cancer, ...
What is the best way to diagnose lung cancer?
To diagnose and stage lung cancer, imaging tests (such as CT scans) and tissue/pathologic reviews are required. There are multiple approaches for tissue evaluation, such as bronchoscopy with biopsy or fine needle aspiration (FNA), mediastinoscopy, and thoracentesis.
What are the symptoms of lung cancer?
To date, a majority of lung cancer cases are diagnosed in symptomatic individuals with the most common symptoms being cough, fatigue, dyspnea, chest pain, weight loss, and hemoptysis. Hemoptysis has the highest positive predictive value of 2.4%–7.5% but is a feature of only a fifth of lung cancers [7].
Does smoking cause lung cancer?
Secondhand smoking has also been shown to increase the risk of lung cancer by as much as 26% [2]. Other risk factors for lung cancer include asbestos exposure, family history of lung cancer, exposure to toxic substances including polycyclic aromatic hydrocarbons, heavy metals, and radon gas [2].
Does cancer stop working?
If Cancer Treatments Stop Working. Cancer treatments can help stop cancer from growing or spreading. But sometimes treatment does not work well or stops working. Maybe treatment ended a while ago and was successful at first, but cancer has come back. Or maybe one type of cancer treatment has stopped working and the cancer has kept growing.
Can palliative care be used for cancer?
Be sure to ask about and get treatment for any symptoms you might have, such as nausea or pain. Palliative care can be used whether you are getting cancer treatment or not. And it can be used at any stage of your illness. Palliative care is used to help ease symptoms and side effects.
How to talk to your loved ones about cancer?
Talking with your loved ones. Be open with your loved ones about your cancer and the news you've been given. Explore their thoughts, feelings, and suggestions. Talk to them about the options you have been given, along with the decisions you have made or are thinking of making. If you feel you need their input, ask.
Can you get a second opinion on cancer?
When faced with deciding whether to continue cancer treatment, some patients or their loved ones may want to get a second opinion. Even when you place full trust in your doctor and cancer care team, you might wonder if another doctor could offer something else or more information. It's normal to think about talking to someone else, and your doctor should support you if you decide to get another opinion. Remember that your cancer care team wants you to be sure about the decisions you make. You can read more in Seeking a Second Opinion.
Can cancer shrink?
If you have cancer that keeps growing or comes back after one kind of treatment, it’s possible that another treatment might still help shrink the cancer, or at least keep it in check enough to help you live longer and feel better. Clinical trials also might offer chances to try newer treatments that could be helpful.
What does hospice care mean?
Hospice care treats the person rather than the disease; it focuses on the quality of your life rather than its length. While getting hospice care means the end of treatments such as chemo and radiation, it doesn’t mean you can’t have treatment for the problems caused by your cancer or other health conditions.
What are the first two immunomodulators to be approved for NSCLC?
The first two immunomodulators to demonstrate success and gain approval in the treatment of NSCLC were two antibodies targeting PD-1, followed by an anti-PD-L1. These three anti-PD-1/PD-L1 antibodies were approved in advanced NSCLC after progression to platinum-based CT as they demonstrated greater efficacy than docetaxel in this context. All of them were compared against docetaxel in randomized phase III studies with a similar design and with the same primary objective of OS, but with some differences that we will discuss below.
What is the treatment for non-small cell lung carcinoma?
The treatment of non-small-cell lung carcinoma (NSCLC) has changed markedly in recent years as a result of two major treatment milestones: Targeted therapy and immunotherapy. Since 2015, immunotherapy has been changing the paradigm of NSCLC treatment in different settings and has contributed to improve the quality of life of these patients. The most widely used immunotherapy strategy in clinical practice is currently PD-1 and CTLA-4 immune checkpoint inhibition-based immunotherapy. Initial successful results came from an improvement in overall survival for pretreated patients, and immunotherapy subsequently moved to a first-line palliative setting as monotherapy, in combination with chemotherapy or as double-checkpoint inhibition. With regard to earlier stages, consolidation immunotherapy after chemoradiation has also changed the paradigm of unresectable NSCLC, with marked benefits in terms of disease-free and overall survival. During the last few years, efforts have focused on the introduction of immunotherapy in earlier stages as neoadjuvant treatment for potentially resectable tumors and in an adjuvant setting, with some very promising results.
What is immunotherapy for lung cancer?
Immunotherapy has revolutionized the treatment of non-small cell lung cancer patients reaching better survival outcomes in first and second palliative setting and in unresectable stage III tumors. Next year’s immunotherapy will also introduce in earlier stages.
What is the cancer-immunity cycle?
Daniel S Chen was the first to describe the cancer–immunity cycle in his publication “ Oncology meets immunology: The cancer–immunity cycl e.” This process begins with the release of tumor antigens by tumor cells, which can be recognized as foreign by the cells of the host immune system and ends with the destruction of these cells [ 8 ]. The immune response against cancer follows a “pseudomilitary” strategy, with seven differentiated steps: (1) Release and presentation of tumor neoantigens by tumor cells, with uptake of these antigens by antigen-presenting dendritic cells, which process them and reduce them to peptides. These peptides bind to the major histocompatibility complex (MHC); (2) recruitment of T lymphocytes at the peripheral lymphoid organs and presentation of peptides bound to MHC-I and MHC-II to T cells, with subsequent recognition of peptides bound to MHC-II by receptors on the CD4+ T lymphocytes; (3) training: priming; and activation of effector T cells to respond to the tumor antigens presented; and (4) attack with displacement of activated T cells to the region containing the tumor. After the specific activation of T cells in peripheral lymphoid organs, they need to be directed to the tumor through the endothelium and infiltrate the stromal tissue within the tumor, which requires certain phenotypic characteristics in the T cell, such as the expression of chemokine receptors or the expression of cell-adhesion molecules in the vascular endothelium that would allow the endothelial barrier to be overcome and the tumor to be invaded; (5) tumor infiltration; (6) recognition of tumor cells by cytotoxic T lymphocytes (T cell receptors need to come into contact with the MHC peptides on the surface of the tumor cell where, in the case of CD8 lymphocytes, they will release the granules containing cytolytic substances, such as perforin and granzyme, into tumor cells to destroy them); and (7) final destruction of tumor cells and release of new tumor neoantigens. Although it is possible to act on each therapeutic level during these phases, the strategies that have reached the clinic to date and have yielded initially successful results are monoclonal antibodies that block immune checkpoints CTLA-4 and PD-1, which control activation of the immune response at peripheral lymphoid organs and tumor level, respectively [ 9 ]. By blocking these immune checkpoints, the negative autoregulatory signal that blocks activation of the immune response is avoided, ultimately producing a stronger immune response with a greater number of active T lymphocytes ready to attack tumor cells. Although the greatest successes to date have been achieved with monoclonal antibodies that target these sites, other strategies that focus on other phases of the activation of the immune response, and combinations of different strategies, are under development [ 10, 11 ]. Nivolumab, pembrolizumab, and sintilimab are anti-PD1 monoclonal antibodies, and atezolizumab and durvalumab are anti-PD-L1 monoclonal antibodies. Ipilimumab and tremelimumab are anti-CTLA-4 antibodies.
What is CTRT in cancer?
Up until 2017, the definitive treatment in patients with unresectable tumors was definitive chemoradiotherapy (CTRT) based on the platinum doublet, irrespective of the histological subtype, and/or molecular characteristics. Moreover, no improvements had been seen after attempts to use induction and/or consolidation CT, biologics, antiangiogenics or vaccines.
Is immunotherapy a neoadjuvant?
In recent years, immunotherapy has also been rapidly introduced at earlier stages as neoadjuvant or adjuvant treatment for resectable and/or potentially resectable stages. Although generally well tolerated, immunotherapy can sometimes cause serious side effects that we must learn to manage [ 7 ].
Is TMB a continuous variable?
As TMB is also a continuous variable, the different definitions of high/low TMB mean that the results from studies with different cut-off points differ. Smoking patients are known to have higher TMB; therefore, it has been proposed as a clinical surrogate [ 139 ]. In the CheckMate 026 trial, nivolumab was superior to CT in patients with high TMB. There was no relationship between PD-L1 expression and TMB, although patients with both variables elevated had higher PFS [ 57 ]. In a retrospective analysis of the MKS-IPACT study [ 140 ], and in CheckMate 012, TMB was found to be related to efficacy, with higher RR and PFS in patients with high TMB [ 73 ].
/surgeon-with-doctors-operating-patient-at-hospital-823884600-5a70801ac673350037a8e496.jpg)
Survival Rates
How Accurate Are Survival Rates?
Symptoms
- Sometimes you will experience no symptoms with lung cancer, especially if it's in an early stage, or even located in the outer areas of the lungs. Depending upon the size of the tumor and its location, symptoms of lung cancer can include:5 1. Cough that's not getting better 2. Shortness of breath 3. Coughing up blood 4. Wheezing 5. Hoarse voice 6. Weight loss 7. Loss of appetite 8. S…
Subtypes
- The majority of all lung cancers fall under the category of NSCLC, about 85%. The subtypes of NSCLC are listed below in the order of most to least common:6 1. Adenocarcinoma 2. SCC 3. LCLC 4. Large cell neuroendocrine carcinoma (LCNEC) 5. Adenosquamous carcinoma 6. Sarcomatoid carcinoma
Treatment
- The treatmentfor NSCLC is determined based upon the stage of your cancer, but may include one or any combination of the following: 1. Surgery: A small part of the lung or an entire lung can be removed during a surgical procedure. 2. Radiation therapy: High-energy X-ray beams are directed at the cancerous tissue to destroy it or slow its growth. This can be used in attempts to cure can…
Summary
- NSCLC is a cancer that starts in the lungs. If caught at an earlier stage, it's more likely to lead to longer survival. When NSCLC is found at a later, more advanced stage, survival rates decrease. NSCLC can be treated in a variety of ways and combinations depending upon the stage. These treatments can include surgery, radiation, chemotherapy, targ...
A Word from Verywell
- Receiving a diagnosis of NSCLC can be very overwhelming. Looking up survival rates may be one of the first things you do to try to determine your outlook. However, it's important to remember that these rates are averages of groups of people over the years and don't shape your specific story. Staying as healthy as possible, such as by quitting smoking, eating a healthy diet, and gett…