Who treatment guidelines for drug- resistant tuberculosis?
Treatment of tuberculosis: guidelines – 4th ed. WHO/HTM/TB/2009.420 1.Antitubercular agents – administration and dosage. 2.Tuberculosis, Pulmonary – drug therapy. 3.National health programs. 4.Patient compliance. 5.Guidelines. I.World Health Organization. Stop TB Dept. ISBN 978 92 4 154783 3 (NLM classification: WF 360)
Who found a cure to TB?
Previous editions had different title : "Treatment of tuberculosis : guidelines for national programmes" WHO/HTM/TB/2009.420 x, 147 p. Bosnian translation version is in Bosnian cyrillic and Bosnian latin respectively
Who guidelines on tuberculosis infection prevention and control?
Networks, committees, advisory groups and taskforces lead by or participated in by WHO. WHO in action. On-the-ground efforts to control disease, promote universal health coverage and develop effective policy on all aspects of health care delivery. Stories from countries and explainers on …
Who launches guidelines on management of latent TB?
NATIONAL TUBERCULOSIS MANAGEMENT GUIDELINES 2009 1 PREFACE Tracking epidemiological trends and the extent to which TB targets have been reached provides an indication of progress in TB control. Two key targets had been set by the World Health Assembly in 1991: to detect 70% and to cure 85% of smear-positive clients by the year 2000.
What is the WHO recommended treatment protocol for TB?
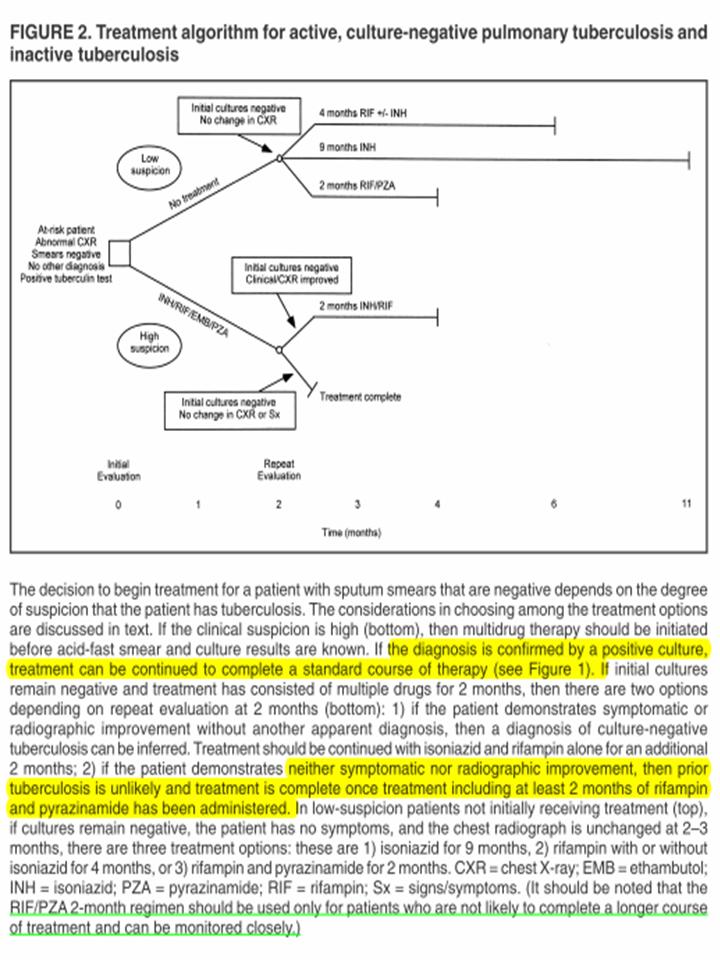
The preferred regimen for treating adults with TB remains a regimen consisting of an intensive phase of 2 months of isoniazid (INH), rifampin (RIF), pyrazinamide (PZA), and ethambutol (EMB) followed by a continuation phase of 4 months of INH and RIF.Aug 11, 2016
WHO TB policy?
WHO/Europe's policy is to end tuberculosis (TB) in all European Member States by 2020 by achieving universal access to high-quality and timely prevention, diagnosis and treatment of all forms of TB.
What is first line treatment for TB?
Of the approved drugs, isoniazid (INH), rifampin (RIF), ethambutol (EMB), and pyrazinamide (PZA) are considered first-line anti-TB drugs and form the core of standard treatment regimens (Figure 6.4) (Table 6.2). Rifabutin (RBT) and rifapentine (RPT) may also be considered first- line drugs under certain circumstances.
WHO TB DOTS program?
What is DOT? DOT means that a trained health care worker or other designated individual (excluding a family member) provides the prescribed TB drugs and watches the patient swallow every dose.
Is TB mandatory?
1. California law requires that school staff and volunteers working with children and community college students be free of infectious tuberculosis (TB) disease.
What is BCG vaccine?
A vaccine used to prevent tuberculosis (TB) in people who are at a high risk of TB or where TB is common. It is rarely given in the U.S. It is made from a weakened form of a bacterium called Mycobacterium bovis (bacillus Calmette-Guérin), which is similar to the bacteria that cause TB.
What is second line treatment?
Second-line treatment is treatment for a disease or condition after the initial treatment (first-line treatment) has failed, stopped working, or has side effects that aren't tolerated. It's important to understand "lines of treatment" and how they differ from first line treatment and can play a role in clinical trials.Jun 9, 2020
What are the 3 types of tuberculosis?
Tuberculosis is a bacterial infection that usually infects the lungs. It may also affect the kidneys, spine, and brain. Being infected with the TB bacterium is not the same as having active tuberculosis disease. There are 3 stages of TB—exposure, latent, and active disease.
WHO latent TB Guidelines 2020?
Key RecommendationsThe first of three preferred regimens is once-weekly isoniazid plus rifapentine, for 3 months. ... The second preferred regimen, daily rifampin for 4 months, is also strongly recommended, especially for HIV-negative persons, and has perhaps the lowest toxicity.More items...•Feb 28, 2020
When did DOTS start in India?
In 1992, the Indian government established a Revised National Tuberculosis Control Programme (RNTCP) using the directly observed treatment, short-course (DOTS) strategy recommended by the World Health Organization (WHO) (3).Mar 22, 2002
Why did the World Health Organization introduce DOTS?
A surge in drug-resistant forms of TB in the former Soviet Union and several other parts of the world requires effective implementation of the DOTS strategy to prevent occurrence of new multidrug-resistant (MDR-TB) cases as well as measures to cure existing MDR-TB cases.
Why is isoniazid called INH?
Isoniazid, also known as isonicotinic acid hydrazide (INH), is an antibiotic used for the treatment of tuberculosis. For active tuberculosis it is often used together with rifampicin, pyrazinamide, and either streptomycin or ethambutol....Isoniazid.Clinical dataPubChem CID3767DrugBankDB00951ChemSpider3635UNIIV83O1VOZ8L33 more rows
What should a tuberculosis treatment plan include?
This plan should include assessment of and referrals for treatment of other illnesses with particular attention to those known to affect treatment outcome , for instance care for diabetes mellitus and malnutrition.
What is the best way to monitor pulmonary TB?
To judge the treatment response of pulmonary TB, the recommended method is sputum smear microscopy. Sputum cultures in quality-assured laboratories should also be performed for monitoring when resources exist.
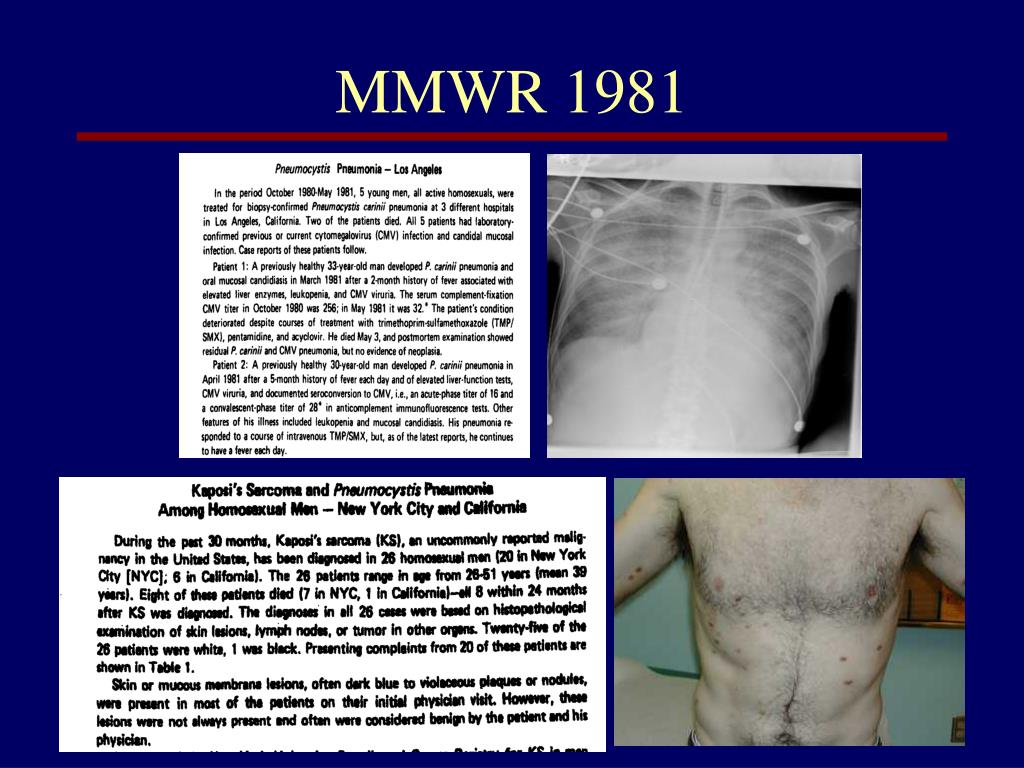
What is the primary cause of death in people living with HIV/AIDS?
Tuberculosis is the primary cause of mortality in people living with HIV/AIDS (PLHIV) worldwide, with 79% of the estimated 1.37 million new cases of TB/HIV in 2007 occurring in sub-Saharan Africa (WHO 2009). Tuberculosis (TB) is highly associated with HIV infection in Zimbabwe, and an estimated 80% of TB cases are co-infected with HIV. The increase in TB in Zimbabwe during the last two decades is largely a result of an escalating HIV epidemic in the context of ongoing operational and resource challenges within the country.
What is TB service?
TB services are a critical entry point for the promotion of HIV prevention, testing and treatment, as well as for adherence support and ARV drug resistance monitoring. Likewise, HIV services are also a critical entry point for TB care. Both HIV/AIDS and TB care require a chronic disease management approach. Ideally, service delivery should be integrated, providing an accessible continuum of care. For collaboration to be effective, the following steps should be taken:
Does HIV affect tuberculosis?
HIV both increases the likelihood of progression from infection with M. tuberculosis to active tuberculosis and changes the clinical presentation of TB disease (PLHIV are more likely to present with extrapulmonary or sputum smear-negative TB than HIV-uninfected TB patients, especially as immunosuppression advances). Knowing a TB patient’s HIV status, therefore, has very important bearing on his or her TB care. Cotrimoxazole prophylaxis and antiretroviral therapy (ART) reduce morbidity and prolong survival following successful TB treatment, but they cannot be provided if the TB patient’s HIV status remains unknown.
What is M&E in HIV?
Monitoring and evaluation (M&E) provide the critical means to assess quality, effectiveness, coverage, and delivery of collaborative TB/HIV activities and is essential to inform planning of new activities and adjustment of ongoing initiatives. Various methods are available for monitoring and evaluating collaborative TB /HIV activities some of which are external reviews of the programme, situation analysis (using country profile checklist), routine monitoring systems, surveillance and surveys, supportive supervision and health management information systems. More details can to be found in the monitoring and evaluation plan.
Is HIV testing recommended for all patients?
HIV testing and counseling should be recommended to all patients of all ages with tuberculosis or suspected of having tuberculosis. Because of the close relationship between tuberculosis and HIV infection, integrated approaches to prevention and treatment of both infections are recommended.
How many people will be treated for TB in 2022?
treat 40 million people for TB disease in the 5-year period 2018–2022; reach at least 30 million people with TB preventive treatment for a latent TB infection in the 5-year period 2018–2022; mobilize at least US$ 13 billion annually for universal access to TB diagnosis, treatment and care by 2022;
How many cases of TB are there in 2019?
Alcohol use disorder and tobacco smoking increase the risk of TB disease by a factor of 3.3 and 1.6, respectively. In 2019, 0.72 million new TB cases worldwide were attributable to alcohol use disorder and 0.70 million were attributable to smoking.
What are the WHO priorities?
WHO is working closely with countries, partners and civil society in scaling up the TB response. Six core functions are being pursued by WHO to contribute to achieving the targets of the UN high-level meeting political declaration, SDGs, End TB Strategy and WHO strategic priorities: 1 Providing global leadership to end TB through strategy development, political and multisectoral engagement, strengthening review and accountability, advocacy, and partnerships, including with civil society; 2 Shaping the TB research and innovation agenda and stimulating the generation, translation and dissemination of knowledge; 3 Setting norms and standards on TB prevention and care and promoting and facilitating their implementation; 4 Developing and promoting ethical and evidence-based policy options for TB prevention and care; 5 Ensuring the provision of specialized technical support to Member States and partners jointly with WHO regional and country offices, catalyzing change, and building sustainable capacity; 6 Monitoring and reporting on the status of the TB epidemic and progress in financing and implementation of the response at global, regional and country levels.
What are the symptoms of lung TB?
Common symptoms of active lung TB are cough with sputum and blood at times, chest pains, weakness, weight loss, fever and night sweats. WHO recommends the use of rapid molecular diagnostic tests as the initial diagnostic test in all persons with signs and symptoms of TB as they have high diagnostic accuracy and will lead to major improvements in the early detection of TB and drug-resistant TB. Rapid tests recommended by WHO are the Xpert MTB/RIF, Xpert Ultra and Truenat assays.
How many countries have TB?
Eight countries account for two thirds of the total, with India leading the count, followed by Indonesia, China, the Philippines, Pakistan, Nigeria, Bangladesh and South Africa. Multidrug-resistant TB (MDR-TB) remains a public health crisis and a health security threat. A global total of 206 030 people with multidrug- or rifampicin-resistant TB ...
Where does TB occur?
TB occurs in every part of the world. In 2019, the largest number of new TB cases occurred in the WHO South-East Asian region, with 44% of new cases, followed by the WHO African region, with 25% of new cases and the WHO Western Pacific with 18%.
What is MDR TB?
Multidrug-resistant tuberculosis (MDR-TB) is a form of TB caused by bacteria that do not respond to isoniazid and rifampicin, the 2 most effective first-line anti-TB drugs. MDR-TB is treatable and curable by using second-line drugs.
What is the objective of the TB guidelines?
The objective of these guidelines is to provide updated, evidence-informed recommendations outlining a public health approach to preventing transmission of M. tuberculosis within the clinical and programmatic management of TB, and to support countries in their efforts to strengthen or build reliable, resilient and effective IPC programmes.
What is the recommendation for TB triage?
Recommendation 1: Triage of people with TB signs and symptoms, or with TB disease, is recommended to reduce M. tuberculosis transmission to health workers (including community health workers), persons attending health care facilities or other persons in settings with a high risk of transmission. (Conditional recommendation based on very low certainty in the estimates of effects)
Why are composite interventions precluded?
precluded because of significant differences between the interventions that were evaluated and potential differences between study populations, which also made it difficult to calculate crude estimates. All studies, apart from the animal study, reported on the effect of composite interventions (i.e. interventions that combine multiple components).
What is a DOI in WHO?
All members of the Guideline Development Group, External Review Group, experts who conducted the systematic reviews, and other technical experts participating in this process completed and submitted a WHO declaration of interest (DOI) form. All experts were instructed to notify the responsible technical officer of any change in relevant interests during this process, in order to review and update conflicts of interest accordingly. As per WHO rules, the objectives of the guideline development process and the composition of the Guideline Development Group, including member biographies, were made public ahead of the meeting.1 This public notice was conducted to allow the public to provide comments pertinent to any competing interests that may have gone unnoticed or that may not have been reported during earlier assessments.
How many people die from tuberculosis in the world?
The World Health Organization (WHO) estimates that close to 54 million TB deaths were averted between 2000 and 2017 because of improved disease prevention and management, and service delivery; nevertheless, up to 10 million people continue to fall ill with TB every year.1
Who are the members of the Guideline Development Group?
The following served as members of the Guideline Development Group: Sujata Baveja, Andra Cīrule, Adrian Roderick (Rod) Escombe, Paul Arthur Jensen, Jun Cheng, Timpiyian Leseni, Shaheen Mehtar, Lindiwe Mvusi, Edward Anthony Nardell, Nguyen Viet Nhung, Isabel Milagros Ochoa-Delgado , Claude Rutanga, Amal Salah Eldin Hassan, Rohit Sarin, Charles Ssonko, Sabira Tahseen, Carrie Tudor and Grigory V. Volchenkov. Special thanks to Holger Schünemann for providing methodological guidance and for chairing both the technical consultations and the in-person Guideline Development Group meeting.
How is GRADE evidence to decision framework developed?
GRADE evidence-to-decision frameworks were developed through the GRADEpro Guideline Development Tool (GDT) software to support the process of moving from evidence to decisions, help Guideline Development Groups structure their discussions, and make the process and the basis for decisions objective and transparent. In the context of global policies, the adoption of evidence-to-decision frameworks facilitates the adaptation of recommendations and decisions to specific contexts, given that these frameworks take into account the prioritization of a public health condition, the balance of desirable and undesirable effects of a given intervention, and other domains such as values, resources, equity, acceptability and feasibility. For each priority question, judgements were made on the impact of the intervention on each domain, to inform and guide the decision-making process.
Screening
- In March 2021, WHO released the WHO consolidated guidelines on tuberculosis. Module 2: Screening – systematic screening for tuberculosis disease (1). These guidelines include 17 new and updated recommendations for the screening of TB disease. Populations identified as priorities for TB screening include contacts of TB patients, people living with HIV, people expose…
Diagnosis
- In July 2021, WHO released the WHO consolidated guidelines on tuberculosis. Module 3: Diagnosis – rapid diagnostics for tuberculosis detection 2021 update (3).Three new classes of nucleic acid amplification test (NAAT) are now endorsed by WHO: 1. moderate complexity automated NAATs, which are recommended for the initial detection of TB and resistance to rifa…
Treatment
- In April 2021, WHO convened a guideline development group (GDG) to review data from a trial conducted in 13 countries that compared 4-month rifapentine-based regimens with a standard 6-month regimen in people with drug-susceptible TB (6). The GDG considereda 4-month regimen composed of rifapentine, isoniazid, pyrazinamide and moxifloxacin that met the non-inferiority c…
Comorbidities, Vulnerable Populations and People-Centred Care
- In May to June 2021, WHO convened a GDG to review updated evidence on the management of TB in children and adolescents (aged 0–9 and 10–19 years, respectively). A rapid communication thatsummarizes the main updates to guidance on the management of TB in children and adolescents was released by WHO in August 2021 (8). The communication includes new inform…
Other Actions to Support TB Policy Guidance
- To exchange views on emerging areas where there is a need for global TB policy guidance, in March 2021, WHO convened a consultation on the translation of TB research into global policy guidelines, attended by scientists, public health experts, partners,civil society and countries (9). In June 2021, WHO launched a TB Knowledge Sharing Platform to bring all WHO TB guidelines, op…