
Systemic and ICS are also used in the treatment of acute asthma exacerbations. Several international asthma management guidelines recommend the use of systemic corticosteroids
Corticosteroid
Corticosteroids are a class of steroid hormones that are produced in the adrenal cortex of vertebrates, as well as the synthetic analogues of these hormones. Two main classes of corticosteroids, glucocorticoids and mineralocorticoids, are involved in a wide range …
Full Answer
Which inhaled corticosteroids are used in the treatment of asthma?
These inhaled corticosteroids include: Qvar ® (beclomethasone dipropionate HFA) Beclovent ® (beclomethasone dipropionate) Flovent ® (fluticasone propionate)
How do corticosteroids help COPD?
People with COPD have airways that are irritated and swollen, which can make it hard to breathe. Corticosteroids reduce inflammation, so they can help to reduce the amount of swelling in the airways and make breathing easier.2.
Do corticosteroids prevent relapse following acute exacerbations of asthma?
Corticosteroids for preventing relapse following acute exacerbations of asthma. Cochrane Database Syst Rev. 2001:CD000195. [PubMed] [Google Scholar]
When do you need to take steroids for COPD?
These patients may need to use steroids as part of long-term maintenance therapy for COPD. Acute exacerbations, which are also called COPD attacks or flare-ups, happen when COPD symptoms suddenly get worse. Corticosteroids for COPD may be taken by inhalation or in pill form by mouth.
Are corticosteroids still recommended to treat eligible COVID-19 patients?
Corticosteroids have been advised as a drug to target the host immune response in patients affected with severe lung inflammation due to coronavirus disease 2019 (COVID-19).
Why should COVID-19 patients not take corticosteroids?
The corticosteroids should not be used in the treatment of non-severe COVID-19 patients because corticosteroids suppress the immune response and reduce the symptoms and associated side effects such as slow recovery, bacterial infections, hypokalemia, mucormycosis and finally increase the chances of death.
What is the relationship between COVID-19 and COPD?
COPD puts you at higher risk to get seriously sick if you were to get infected with SARS-CoV-2, the virus that causes COVID-19.
Are patients with COPD at an increased risk of severe disease from COVID-19?
Studies have shown that 2% of patients diagnosed with COVID-19 have also been diagnosed with COPD. While the prevalence of COVID-19 in patients with COPD is relatively low, those who are infected with the virus experience more severe symptoms than those without COPD.
Will a cortisone injection interfere with the COVID-19 vaccine?
Musculoskeletal corticosteroid injections are common procedures which are most often performed in an elective, outpatient setting. These can include intra-articular, bursal, tendon, and neuraxial injections. Currently there is no direct evidence of the impact of corticosteroid injections on vaccine efficacy.
What medications should be avoided before the COVID-19 vaccine?
It is not recommended you take over-the-counter medicine – such as ibuprofen, aspirin, or acetaminophen – before vaccination for the purpose of trying to prevent vaccine-related side effects.
When is the greatest risk of respiratory complications from COVID-19 for older patients?
While every patient is different, doctors say that days five through 10 of the illness are often the most worrisome time for respiratory complications of Covid-19, particularly for older patients and those with underlying conditions like high blood pressure, obesity or diabetes.
Which groups of people are at increased risks of severe illness from COVID-19?
Among adults, the risk for severe illness from COVID-19 increases with age, with older adults at highest risk. Severe illness means that the person with COVID-19 may require hospitalization, intensive care, or a ventilator to help them breathe, or they may even die. People of any age with certain underlying medical conditions are also at increased risk for severe illness from SARS-CoV-2 infection.
Which organ system is most often affected by COVID-19?
COVID-19 is a disease caused by SARS-CoV-2 that can trigger what doctors call a respiratory tract infection. It can affect your upper respiratory tract (sinuses, nose, and throat) or lower respiratory tract (windpipe and lungs).
Who is most at risk for the coronavirus disease?
Older adults are at highest risk of getting very sick from COVID-19. More than 81% of COVID-19 deaths occur in people over age 65. The number of deaths among people over age 65 is 97 times higher than the number of deaths among people ages 18-29 years.
Are smokers more likely to develop severe disease with COVID-19?
Tobacco smoking is a known risk factor for many respiratory infections and increases the severity of respiratory diseases. A review of studies by public health experts convened by WHO on 29 April 2020 found that smokers are more likely to develop severe disease with COVID-19, compared to non-smokers.
Who is at greatest risk of infection from COVID-19?
Currently, those at greatest risk of infection are persons who have had prolonged, unprotected close contact (i.e., within 6 feet for 15 minutes or longer) with a patient with confirmed SARS-CoV-2 infection, regardless of whether the patient has symptoms.
Which corticosteroids are more effective for asthma?
Development of corticosteroids that have less mineralocorticoid activity, like prednisone, and later those that have no mineralocorticoid activity, like dexamethasone, made corticosteroids more attractive therapies to use in asthma.
How long after asthma exacerbation can you take corticosteroids?
Systemic corticosteroids were found to speed resolution of symptoms, decrease the rate of admission and decrease the rate of relapse if administered for 3-5 days after the acute exacerbation. More detailed discussion about the use of systemic corticosteroids in the treatment of acute asthma can be found below.
What causes asthma in children?
The most common cause of acute asthma exacerbation in both adults and children, but more in children, is viral respiratory tract infections. Viruses may be responsible for up to 80% of wheezing episodes in children and 50-75% of episodes in adults.[5] . Many viruses can cause exacerbation of asthma symptoms, the most important ...
What is the most common pathological feature of asthma?
Bronchial airways inflammation is the most prominent pathological feature of asthma. Inhaled corticosteroids (ICS), through their anti-inflammatory effects have been the mainstay of treatment of asthma for many years. Systemic and ICS are also used in the treatment of acute asthma exacerbations. Several international asthma management guidelines ...
What are the most common viruses that cause asthma?
Many viruses can cause exacerbation of asthma symptoms, the most important and most common is rhinovirus. [6] . Respiratory syncycial virus and influenza virus also cause significant proportion of exacerbations. Airway epithelial cells play a major role in the pathology of virally induced asthma exacerbation.
What are the symptoms of asthma?
Examination of patients with acute asthma may reveal increased respiratory rate, retractions (accessory respiratory muscle use), wheezing, oxygen desaturation on pulse oximetry and in more severe cases, inability to speak, silent chest, with reduced respiratory lung volumes, cyanosis, and change in mental status.
Do asthma patients respond to corticosteroids?
Patients tend to have severe, more aggressive, and poorly controlled asthma. They usually do not respond to corticosteroids as well as the eos inophilic type. In the paucigranulocytic phenotype, bronchial neutrophils, and eosinophils are much lower.[4] Asthmatic patients frequently experience acute exacerbations.
Why do you need an oral corticosteroid for asthma?
Oral corticosteroids (OCS) When our asthma is flaring up and our daily maintenance ICS aren’t enough to keep asthma symptoms at bay, your doctor may put you on an oral corticosteroid for a short period of time to decrease the amount of inflammation in the lungs.
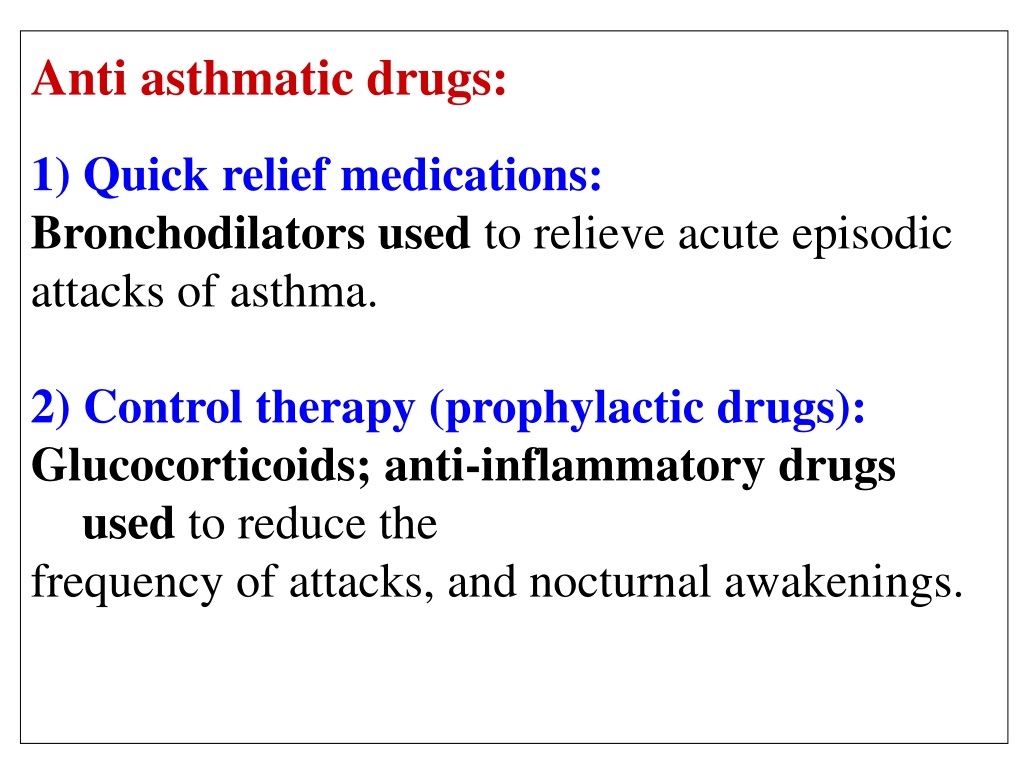
What are the three forms of corticosteroids?
Corticosteroids have become center stage in the treatment and prevention of asthma exacerbations. They come in three forms: oral, inhaled, and intravenous (IV).
What does "set" mean in asthma?
When providing education for asthmatics, in the respiratory field we use the SET mnemonic. SET stands for S welling, E xcess mucus, and T ightness. These are the three main things that happen during an asthma flare-up or asthma attack. Inflammation in the lungs is what causes the swelling which makes it difficult to breathe. Mucus production is increased and when combined with the swelling and tightness, causes wheezing. Tightness happens from both the swelling and bronchospasm. These three things create a perfect storm when you are exposed to a trigger.
Can asthma be controlled without breathing?
Not everyone will experience the same side effects and some might not experience any at all. You will have to weigh the options with your doctor and decide what is the best course of action for your specific asthma. While the side effects may be unpleasant, not being able to breathe is far worse. Being able to keep your asthma controlled without ...
Do corticosteroids cause inflammation?
Corticosteroids mimic the hormones that are produced naturally in the body (more specifically the adrenal glands). When the dose is more than what the body naturally makes, it suppresses inflammation.
Can you use OCS for asthma?
Being able to keep your asthma controlled without excessive use of OCS is ideal. However in rare cases, there is a need for long term daily OCS due to asthma severity. Long term use of OCS can lead to some serious problems including decreased bone density, diabetes, and adrenal fatigue.
What steroid is used to treat COPD?
1,2. Oral steroids that are used to treat people with COPD include: Prelone ® (prednisolone) Deltasone ® (prednisone) Medrol ® (methylprednisolone)
What is the name of the medication that is used to treat COPD?
April 7, 2015. Corticosteroids are a type of medicine commonly used as part of a treatment plan for chronic obstructive pulmonary disease (COPD). Corticosteroids are also called steroids or glucocorticosteroids. They are similar to hormones produced naturally in the adrenal glands, which sit on top of the kidneys.
What is flovent used for?
Flovent ® (fluticasone propionate) Azmacort ® (triamcinolone acetonide) For people with a more advanced stage of COPD, inhaled steroids can help them to: Manage COPD symptoms. Have improved lung function. Have a better quality of life. Reduce the number of COPD flare-ups that they have 1,2.
What is a flare up of COPD?
Acute exacerbations, which are also called COPD attacks or flare-ups, happen when COPD symptoms suddenly get worse. People who have a moderate or severe COPD flare-up may need corticosteroid treatment to help bring the attack under control and keep it from getting worse. 1,2. Corticosteroids for COPD may be taken by inhalation or in pill form by ...
Why do people with COPD have a hard time breathing?
Corticosteroids reduce inflammation, so they can help to reduce the amount of swelling in the airways and make breathing easier. 2.
Why do you need bronchodilators for COPD?
Bronchodilators are medicines commonly used to treat COPD symptoms. Because of the swelling in the airways, the band of muscles surrounding the airways can tighten up . This causes the airway to become too narrow for enough air to pass through to the lungs.
How long does it take for steroids to work?
It can take days or weeks of treatment for inhaled steroids to start working at full strength in a person's body. Some patients need treatment that takes effect more quickly than that. For this reason, some people need to take steroids by mouth, in pill, tablet or liquid form. 1,2
