First generation cephalosporins generally cause few side effects. The most common side effects reported include diarrhea, nausea and vomiting, dyspepsia, gastritis and abdominal pain. Transient liver problems have also been reported.
What are first generation cephalosporins used for?
First generation cephalosporins refer to the first group of cephalosporins discovered. Their optimum activity is against gram-positive bacteria such as staphylococci and streptococci. They have little activity against gram-negative bacteria. What are first generation cephalosporins used for?
What bacteria do first-generation cephalosporins kill?
First-generation cephalosporins have active coverage against most gram-positive cocci such as staphylococcispp. and streptococcispp. while having minimal coverage against gram-negative bacteria. Gram-negative bacteria that are more susceptible to first-generation cephalosporins areProteus mirabilis, E. coli, andKlebsiella pneumoniae.
Can first-generation cephalosporins be used for complicated upper urinary tract infection?
Introduction Complicated upper urinary tract infection (UTI) is a significant cause of infectious morbidity and in-hospital antibiotic therapy. However, the use of first-generation cephalosporins in this scenario is not clearly defined.
What do we know about third-generation cephalosporins?
Third-generation cephalosporins have less coverage against most gram-positive organisms but have increase coverage against Enterobacteriaceae, Neisseria spp., and H. influenza.
What is the first generation of cephalosporins?
When was the first cephalosporin discovered?
What is the name of the antibiotic that kills bacteria?
What are the side effects of cephalosporins?
Is cephalosporin safe?
Can you take cephalosporin long term?
Can cephalosporin cause seizures?
See more
About this website

What do first generation cephalosporins treat?
A broad-spectrum cephalosporin antibiotic used for the treatment of serious bacterial infections in various locations, such as the urinary tract, skin, bone, and lower respiratory tract. A first generation cephalosporin used to treat certain susceptible bacterial infections.
What is the effect of cephalosporins?
Cephalosporins are bactericidal (kill bacteria) and work in a similar way to penicillins. They bind to and block the activity of enzymes responsible for making peptidoglycan, an important component of the bacterial cell wall.
When are 1st generation cephalosporins used?
First generation cephalosporins may be used to treat infections caused by susceptible bacteria such as: Bone infections. Ear infections (eg, otitis media) Skin infections.
What does first generation cephalosporin mean?
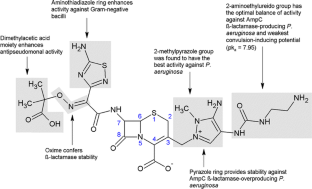
First-generation cephalosporins are a large group of antibiotic agents that work through their beta-lactam rings. Their pharmacokinetics involve the beta-lactam rings binding to the penicillin-binding protein that is found in various bacteria.
Which generation of cephalosporin is more effective?
Third-generation cephalosporins are more effective against Gram-negative bacteria compared to both the first and second generations. They're also more active against bacteria that may be resistant to previous generations of cephalosporins.
What are 1st generation antibiotics?
The natural or "first generation" penicillins are bactericidal antibiotics naturally derived from the mold, Penicillium chrysogenum. Their basic structure includes a thiazolidine ring connected to a beta-lactam ring with a variable side chain.
What is the mode of action of cephalosporins?
Mechanism of action Cephalosporins are bactericidal and, like other β-lactam antibiotics, disrupt the synthesis of the peptidoglycan layer forming the bacterial cell wall. The peptidoglycan layer is important for cell wall structural integrity.
What Are First Generation Cephalosporins Used for?
First generation cephalosporins may be used to treat infections caused by susceptible bacteria such as: 1. Bone infections 2. Ear infections (eg, o...
What Are The Differences Between First Generation Cephalosporins?
Cephalexin and cefadroxil can be given by mouth, whereas cefazolin can only be given by injection (IV/IM). There are also differences with regards...
Are First Generation Cephalosporins Safe?
First generation cephalosporins are generally safe, with low toxicity and good efficacy against susceptible bacteria.Allergic reactions have been r...
What Are The Side Effects of First Generation Cephalosporins?
First generation cephalosporins generally cause few side effects. The most common side effects reported include diarrhea, nausea and vomiting, dysp...
1st and 2nd generation antibiotics - Nursing Student Assistance - allnurses
I find it hard to understand 1st, 2nd generation and so forth and so on of antibiotics! Please ! Desperately need the help of everyone!
List of Cephalosporins + Uses, Types & Side Effects - Drugs.com
Since the first cephalosporin was discovered in 1945, scientists have been improving the structure of cephalosporins to make them more effective against a wider range of bacteria. Each time the structure changes, a new "generation" of cephalosporins are made. So far there are five generations of cephalosporins.
First Generation Cephalosporins - GlobalRPH
First generation Cephalosporins Background: 'Cephalosporins are bactericidal and have the same mode of action as other beta-lactam antibiotics (such as penicillins) but are less susceptible to penicillinases. Cephalosporins disrupt the synthesis of the peptidoglycan layer of bacterial cell walls. The peptidoglycan layer is important for cell wall structural integrity.
What is the first generation of cephalosporins?
First generation cephalospor ins refer to the first group of cephalosporins discovered. Their optimum activity is against gram-positive bacteria such as staphylococci and streptococci. They have little activity against gram-negative bacteria.
When was the first cephalosporin discovered?
Since the first cephalosporin was discovered in 1945 , scientists have been improving the structure of cephalosporins to make them more effective against a wider range of bacteria. Each time the structure changes, a new "generation" of cephalosporins are made. So far there are five generations of cephalosporins.
What is the name of the antibiotic that kills bacteria?
Cephalosporins are a large group of antibiotics derived from the mold Acremonium (previously called Cephalosporium ). Cephalosporins are bactericidal (kill bacteria) and work in a similar way to penicillins.
What are the side effects of cephalosporins?
The most common side effects reported include diarrhea, nausea and vomiting, dyspepsia, gastritis and abdominal pain. Transient liver problems have also been reported.
Is cephalosporin safe?
First generation cephalosporins are generally safe, with low toxicity and good efficacy against susceptible bacteria.
Can you take cephalosporin long term?
People with ki dney or liver disease, nutritionally deprived, taking cephalosporins long-term, or concurrently receiving anticoagulant therapy are more at risk. For a complete list of severe side effects, please refer to the individual drug monographs.
Can cephalosporin cause seizures?
Rarely, seizures have been reported with some cephalosporins; the risk is greatest in those with kidney disease.
What is the first generation of cephalosporins?
First generation Cephalosporins. Background : "Cephalosporins are bactericidal and have the same mode of action as other beta-lactam antibiotics (such as penicillins) but are less susceptible to penicillinases. Cephalosporins disrupt the synthesis of the peptidoglycan layer of bacterial cell walls. The peptidoglycan layer is important ...
What is the difference between first and second generation cephalosporins?
The first cephalosporins were designated first-generation cephalosporins, where as, later , more extended-spectrum cephalosporins were classified as second-generation cephalosporins. Each newer generation has significantly greater gram-negative antimicrobial properties than the preceding generation, in most cases with decreased activity against gram-positive organisms. Fourth-generation cephalosporins, however, have true broad-spectrum activity.
What is the role of cephalosporins in the cell wall?
Cephalosporins disrupt the synthesis of the peptidoglycan layer of bacterial cell walls. The peptidoglycan layer is important for cell wall structural integrity. The final transpeptidation step in the synthesis of the peptidoglycan is facilitated by transpeptidases known as penicillin-binding proteins (PBPs).
How long should you take antibiotics after asymptomatic?
As with antibiotic therapy in general, treatment should be continued for a minimum of 48 to 72 hours after the patient becomes asymptomatic or evidence of bacterial eradication has been obtained.
How much tsp for pharyngitis?
For pharyngitis, tonsillitis, and impetigo, the recommended daily dosage for children is 30 mg/kg/day in a single dose or in equally divided doses every 12 hours.
Can Cefadroxil be administered orally?
DOSAGE AND ADMINISTRATION: Cefadroxil is acid-stable and may be administered orally without regard to meals.
Is cephalosporin bactericidal?
In vitro tests demonstrate that the cephalosporins are bactericidal because of their inhibition of cell-wall synthesis. Cefadroxil has been shown to be active against the following organisms both in vitro and in clinical infections: Beta-hemolytic streptococci. Staphylococci, including penicillinase-producing strains.
What is a cephalosporin?
Cephalosporins are broad-spectrum antibiotics used to manage a wide range of bacterial infections. They are derived from the mold Acremonium (previously called Cephalosporium). Cephalosporins are grouped into five generations based on their spectrum of coverage against gram -positive and gram-negative bacteria. They are administered intravenously or orally depending on the infection.
What is the role of cephalosporins in bacterial cell wall synthesis?
First-generation cephalosporins inhibit bacterial cell wall synthesis and have the same mode of action as other beta-lactam antibiotics (such as penicillins). They disrupt the synthesis of the peptidoglycan layer forming the bacterial cell wall. The peptidoglycan layer is important for cell wall structural integrity.
What are the first generation cephalosporins?
First-generation cephalosporins include cefazolin, cephalothin, cephapirin, cephradine, cefadroxil, and cephalexin. First-generation cephalosporins have active coverage against most gram-positive cocci such as staphylococcispp. and streptococcispp. while having minimal coverage against gram-negative bacteria. Gram-negative bacteria that are more susceptible to first-generation cephalosporins areProteus mirabilis, E. coli, andKlebsiella pneumoniae. Oral first-generation cephalosporins are commonly prescribed to use against uncomplicated skin and soft tissue infections such as cellulitis and abscesses commonly due to a staphylococcispp. or streptococcispp.infection. Additionally, clinicians can use them for bone, respiratory tract, genitourinary tract, biliary tract, bloodstream infection, otitis media, and surgical prophylaxis. In fact, cefazolin is the cephalosporin of choice for surgical prophylaxis. One of the non-FDA-approved indications is to use first-generation cephalosporins for endocarditis prophylaxis for those who are susceptible and undergoing a dental or respiratory procedure. [1][2][3]
What is the purpose of cephalosporins?
Oral first-generation cephalosporins are commonly prescribed to use against uncomplicated skin and soft tissue infections such as cellulitis and abscess es commonly due to a staphylococcispp. or streptococcispp.infection.
What is cephalosporin used for?
Cephalosporins are beta-lactam antimicrobials used to manage a wide range of infections from gram-positive and gram-negative bacteria. The five generations of cephalosporins are useful against skin infection, resistant bacteria, meningitis, and other infections. This activity describes the indications, contraindication, ...
What are the two subgroups of cephalosporins?
Second-generation cephalosporins divide into two subgroups: the second-generation and the cephamycin subgroup. Some of the second-generation subgroups include cefuroxime and cefprozil. The cephamycin subgroup includes cefmetazole, cefotetan, and cefoxitin.
How does Staphylococcus aureus develop resistance to cephalosporins?
Staphylococcus aureusthat is initially susceptible to cephalosporins can develop resistance by changing the structure of the penicillin-binding proteins. S. aureus does this by having a gene that encodes a modified penicillin-binding protein; this prevents the cephalosporin’s beta-lactam rings to inactivate the protein.
Is cefazolin a surgical prophylaxis?
In fact, cefazolin is the cephalosporin of choice for surgical prophylaxis. One of the non-FDA approved indication is to use first-generation cephalosporins for endocarditis prophylaxis for those who are susceptible and undergoing a dental or respiratory procedure. [1][2][3]
Does cefepime cover gram negative bacteria?
Cefepime has an additional quaternary ammonium group, which allows them to penetrate the outer membrane of gram-negative bacteria better. Similar to the activity of cefotaxime and ceftriaxone, cefepime can cover Streptococcus pneumoniaeand methicillin-sensitive Staphylococcus aureus(MSSA).
Where are cephalosporins used?
Use of the most common cephalosporins across Europe, as a proportion of total cephalosporin use in each country, in the year ending August 2013. Countries (from left to right for each agent, arranged by CDI incidence): <1: Bulgaria; 1–4: Belgium, France, Greece, Portugal, Slovakia, Spain, UK; >4–8: Austria, Czech Republic, Italy, Netherlands, Romania; >8–12: Germany, Ireland, Poland; >12–16: Hungary, Sweden; >20: Finland. CDI incidence data from September 2012 to August 2013 from Davies et al.17Prescription data from IMS Health.
What is antibiotic stewardship?
Antibiotic stewardship programmes have been established in an attempt to optimize and sustain the utility of antibiotics; this includes reducing the rates of resistance and hospital-associated CDI. Some policies are focused on the restriction of cephalosporin prescribing.15For example, in 2008, the UK Department of Health and Public Health England recommended that NHS hospitals should develop restrictive antibiotic guidelines specifying the use of narrow-spectrum agents alone or as combination therapy.16The guidelines specifically highlighted that the use of clindamycin and second- and third-generation cephalosporins should be avoided, especially in the elderly; reduced use of fluoroquinolones and carbapenems was also advocated.16
What are the most common antibiotics associated with CDI?
Three recent meta-analyses have evaluated the association between antibiotic use and CDI.10–12They reported that cephalosporins and clindamycin were most strongly associated with hospital-associated CDI,10while for community-associated infection, the strongest association was seen with clindamycin, cephalosporins and quinolones.11,12These analyses may, however, be subject to several potential sources of confounding and bias from the included studies, and so reported associations between CDI and specific antibiotics should be interpreted with caution.13Possible confounding factors that could affect the analyses include the presence of comorbidities, polypharmacy, dose and duration of antibiotic treatment, and the use of multiple antibiotics.13Additional potential sources of bias include sampling bias (meaning that commonly prescribed antibiotics will be more often reported as being associated with cases), selection of inappropriate controls and misclassification of C. difficile. In addition, studies may be open to clinical susceptibility bias, whereby patients with illnesses requiring antibiotics may have inherent increased risks of developing CDI, and cases may therefore be falsely attributed solely to the clinically indicated use of antibiotics.13Furthermore, there were between-study differences in patient populations which, importantly, may have included different levels of exposure to C. difficile.13Notably, most of the data on CDI have been collected from observational studies in the context of outbreaks,14and therefore may not reflect the risk of CDI in the non-epidemic setting. Finally, the assumption that all antibiotics within a given class are equally associated with CDI risk is not well founded. Notably, differences in pharmacokinetics among cephalosporins, particularly the route of excretion, can mean that exposures of the gut microbiome and C. difficilevary markedly.
How does the gut microbiota help with C. difficile?
Gut microbiota provides an important host defence against C. difficileby inhibiting its establishment or proliferation. 23Studie s in patients with CDI have reported that CDI is associated with significant changes in the composition of faecal microbiota, including, in some cases, the depletion of Gram-negative Bacteroidesspp., and reductions in normally abundant butyrate-producing anaerobic bacteria in the Ruminococcaceaeand Lachnospiraceaefamilies (part of the Clostridiaclass), suggesting that they may also be involved in the defence against infection.24Disruption of gut microbiota during antimicrobial use helps to create conditions favourable for C. difficileexpansion.25,26Long or repeated courses of antimicrobial therapy and the use of multiple antimicrobials can increase the risk of CDI.27Some broad-spectrum antimicrobials have been implicated in CDI owing to their wide-ranging effects on the microbiota. Importantly, the impact of an antimicrobial on gut microbiota will depend on the drug's pharmacokinetic distribution and the concentration achieved in the gut, as well as its antimicrobial activity.28
How long after bacteremia is cefazolin effective?
Bacteremia severity at 72 h after bacteremia onset was regarded as the baseline for the initiation of definitive therapy. The primary outcome was assessed as treatment failure of definitive cefazolin therapy at the 3 to 15 day visit after bacteremia onset, and included a composite of antimicrobial escalation to broad-spectrum agents, the development of breakthrough bacteremia, or the need for intensive care during definitive cefazolin therapy and 15-day crude mortality after bacteremia onset. The secondary outcomes, including 30-day crude mortality after bacteremia onset, recurrent infections, and fatal outcomes within 90 days after the end of definitive cefazolin therapy, were assessed during the period between Day 15 of the bacteremia episode and the 90 day visit after the end of definitive cefazolin therapy.
What is community onset bacteremia?
Community-onset bacteremia indicates that the place of bacteremia onset is the community , and includes long-term healthcare, facility-acquired and community-acquired bacteremia, as previously described [4,19]. Since susceptibility data were available approximately three days after bacteremia onset, empirical therapy was arbitrarily defined as the drugs prescribed within three days after bacteremia onset, whereas definitive therapy referred to the drugs prescribed when the susceptibility result became available. As previously described [4,19], antimicrobial therapy was considered to be appropriate when the following two criteria were fulfilled: (i) the route and dosage of antimicrobial administration were as recommended in the Sanford Guide [20]; and (ii) causative pathogens exhibited in vitro susceptibility to the administrated drugs according to the contemporary CLSI breakpoint [12]. The time-to-appropriate antibiotic measured in hours was defined as the period between bacteremia onset (i.e., ED arrival) and administration of the first dose of appropriate antimicrobials. A time-to-appropriate antibiotic of >24 h was considered as inappropriate empirical therapy [4,21].
Is cefazolin a gram positive antibiotic?
Currently, the therapeutic role of cefazolin has been emphasized on surgical prophylaxis [5] and the treatment of infectious diseases due to cefazolin-susceptible, gram-positive organism s [7,8]. Although it was active against common pathogens in the community, such as E. coli, K. pneumoniae, and P. mirabilis, clinical outcome information dealing with these common bacterial infections, except for urinary tract infections [30,31,32], was limited. Recently, numerous investigations focused on those with systemic infections, especially bacteremia or septicemia [14,15,33,34], but the rationale of the revised MIC breakpoint to augment cefazolin administration as definitive therapy remained under debate. Furthermore, antimicrobial resistance in bacterial microorganism is a worldwide challenge, resulting in high morbidity and mortality [35]. To minimize the use of broad-spectrum antibiotics in the era of increasing antimicrobial resistance among the pathogens causing community-acquired or healthcare-associated infections, it is crucial to explore the therapeutic role of intravenous cefazolin for adults with EKP bacteremia. Although patients empirically treated by various active antimicrobials were included, our study showed that definitive cefazolin therapy was safe for those infected by EKP isolates with cefazolin MICs of ≤2 mg/L, if a patient is stable after 72 hours’ empirical antimicrobial therapy.
Is cefazolin MIC related?
The cefazolin-MIC-related trend ( all γ= 1.00, p= 0.01) in primary and secondary outcomes of adults with community-onset monomicrobial Escherichia coli, Klebsiellaspecies, or Proteus mirabilisbacteremia definitively treated by cefazolin. Early treatment failure, i.e., primary outcome, was the composite of antimicrobial escalation to broad-spectrum agents, the development of breakthrough bacteremia, the need for intensive care during definitive cefazolin therapy, and crude mortality within 15 days after bacteremia onset.
Is cefazolin effective against E. coli?
Background: Cefazolin is in vitro active against wild isolates of Escherichia coli, Klebsiellaspecies, and Proteus mirabilis(EKP), but clinical evidence supporting the contemporary susceptibility breakpoint issued by the Clinical and Laboratory Standards Institute (CLSI) are limited. Methods: Between 2010 and 2015, adults with monomicrobial community-onset EKP bacteremia with definitive cefazolin treatment (DCT) at two hospitals were analyzed. Cefazolin minimum inhibitory concentrations (MICs) were correlated with clinical outcomes, including primary (treatment failure of DCT) and secondary (30-day mortality after bacteremia onset, recurrent bacteremia, and mortality within 90 days after the end of DCT) outcomes. Results: Overall, 466 bacteremic episodes, including 340 (76.2%) episodes due to E. coli, 90 (20.2%) Klebsiellaspecies, and 16 (3.6%) P. mirabilisisolates, were analyzed. The mean age of these patients was 67.8 years and female-predominated (68.4%). A crude 15- and 30-day mortality rate was 0.7% and 2.2%, respectively, and 11.2% experienced treatment failure of DCT. A significant linear-by-linear association of cefazolin MICs, with the rate of treatment failure, 30-day crude mortality, recurrent bacteremia or 90-day mortality after the DCT was present (all γ= 1.00, p= 0.01). After adjustment, the significant impact of cefazolin MIC breakpoint on treatment failure and 30-day crude mortality was most evident in 2 mg/L (>2 mg/L vs. ≤2 mg/L; adjusted hazard ratio, 3.69 and 4.79; p< 0.001 and 0.02, respectively). Conclusion: For stabilized patients with community-onset EKP bacteremia after appropriate empirical antimicrobial therapy, cefazolin might be recommended as a definitive therapy for cefazolin-susceptible EKP bacteremia, based on the contemporary CLSI breakpoint.
Is cefazolin a bactericidal drug?
Cefazolin, a parental first-generation cephalosporin, is bactericidal against Staphylococcus aureus, streptococci, Escherichia coli, Klebsiellaspecies, and Proteus mirabilis(EKP) [1]. EKP are the common pathogens that cause varied infections in the community, such as urinary tract infections [2], biliary tract infections [3], and bacteremia [3,4]. However, most published clinical studies have focused on its efficacy in surgical prophylaxis [5] and infections predominately due to staphylococci, such as bloodstream infections [6], bone and joint infections [7], skin and skin structure infections [8], and peritonitis related to continuous ambulatory peritoneal dialysis [9].
Does cefazolin help with bacteremia?
For adults with community-onset bacteremia due to an EKP isolate with cefazolin MIC ≤2 mg/L, definitive cefazolin therapy can result in a favorable prognosis, which is consistent with the contemporary susceptible breakpoint of CLSI. Accordingly, antimicrobial de-escalation to cefazolin can be considered in the treatment of bacteremia caused by “cefazolin-susceptible” EKP isolates in stabilized adults.
What is the first generation of cephalosporins?
First generation cephalospor ins refer to the first group of cephalosporins discovered. Their optimum activity is against gram-positive bacteria such as staphylococci and streptococci. They have little activity against gram-negative bacteria.
When was the first cephalosporin discovered?
Since the first cephalosporin was discovered in 1945 , scientists have been improving the structure of cephalosporins to make them more effective against a wider range of bacteria. Each time the structure changes, a new "generation" of cephalosporins are made. So far there are five generations of cephalosporins.
What is the name of the antibiotic that kills bacteria?
Cephalosporins are a large group of antibiotics derived from the mold Acremonium (previously called Cephalosporium ). Cephalosporins are bactericidal (kill bacteria) and work in a similar way to penicillins.
What are the side effects of cephalosporins?
The most common side effects reported include diarrhea, nausea and vomiting, dyspepsia, gastritis and abdominal pain. Transient liver problems have also been reported.
Is cephalosporin safe?
First generation cephalosporins are generally safe, with low toxicity and good efficacy against susceptible bacteria.
Can you take cephalosporin long term?
People with ki dney or liver disease, nutritionally deprived, taking cephalosporins long-term, or concurrently receiving anticoagulant therapy are more at risk. For a complete list of severe side effects, please refer to the individual drug monographs.
Can cephalosporin cause seizures?
Rarely, seizures have been reported with some cephalosporins; the risk is greatest in those with kidney disease.