Medication
To prepare for the appointment, make a list of:
- Any symptoms your loved one is experiencing, including any that may seem unrelated to the reason for the appointment
- Key personal information, including any major stresses or recent life changes
- Medications, vitamins, herbs and other supplements that he or she is taking, including the dosages
- Questions to ask the doctor
Therapy
- training primary health-care personnel;
- providing access to essential drugs;
- supporting families in providing home care;
- educating the public to decrease stigma and discrimination;
- enhancing independent living skills through recovery-oriented psychosocial interventions (e.g. ...
What are the most effective treatments for schizophrenia?
- Conventional antipsychotics and traditional services. Kane & Lieberman, 1987 ). ...
- New treatments: atypical antipsychotics and psychosocial interventions. ...
- Atypicals first-line drug. ...
- Barriers to progress. ...
- Using atypicals properly. ...
What is the current treatment for schizophrenia?
The main treatments for childhood schizophrenia are:
- Medications
- Psychotherapy
- Life skills training
- Hospitalization
What is the first line treatment for schizophrenia?
What drugs are approved for schizophrenia?

What was the original treatment for schizophrenia?
The early 20th century treatments for schizophrenia included insulin coma, metrazol shock, electro-convulsive therapy, and frontal leukotomy. Neuroleptic medications were first used in the early 1950s.
How was schizophrenia treated in the 1960s?
During the 1950-1960s, two major changes occurred in the way schizophrenia was treated. The first was a shift in treatment focus from long-term custodial to community-based care. The second change was the introduction of efficacious pharmacotherapy.
Which of the following treatments was used in the 1930s to treat schizophrenia?
Insulin coma treatment was introduced during the 1930s. Patients were administered gradually increasing doses of insulin until a coma occurred. After being monitored for an hour the patient was administered glucose, which terminated the coma. Patients were commonly administered as many as 20 comas.
How was psychosis treated in the past?
During the medieval era, patients with psychosis were imprisoned in dungeons alongside criminals or locked up in lunatic asylums. Treatment mainly involved physical punishments and torture. Men and women with psychosis and other mental health disorders were often accused and tried for practicing witchcraft.
How was schizophrenia treat before antipsychotics?
Historical Treatment Treatment of schizophrenia in the 1940s included insulin therapy – which was introduced by Sakel in Vienna in 1933, Metrazol (a convulsant) by Meduna in Budapest in 1934, prefrontal leucotomy by Moniz in Portugal in 1937 and electroconvulsive therapy by Cerletti and Bini in Italy in 1938.
How were the mentally ill treated in the 1950s?
The use of certain treatments for mental illness changed with every medical advance. Although hydrotherapy, metrazol convulsion, and insulin shock therapy were popular in the 1930s, these methods gave way to psychotherapy in the 1940s. By the 1950s, doctors favored artificial fever therapy and electroshock therapy.
What was used before antipsychotics?
Prior to chlorpromazine, the options for treating psychotic patients were electroconvulsive therapy, hydrotherapy, and putting patients in an insulin coma. None of those are antipsychotic in nature. When two psychiatrists, Dr.
How was mental illness treated in the 1960s?
In the 1960s, social revolution brought about major changes for mental health care including a reduction in hospital beds, the growth of community services, improved pharmacological and psychological interventions and the rise of patient activism.
How was mental illness treated in the 1800s?
In early 19th century America, care for the mentally ill was almost non-existent: the afflicted were usually relegated to prisons, almshouses, or inadequate supervision by families. Treatment, if provided, paralleled other medical treatments of the time, including bloodletting and purgatives.
How did they treat schizophrenia in the 1980s?
Between the 1950s and the 1980s, the antipsychotic medications available to treat this devastating mental illness were a double-edged sword. On the one hand, they helped control symptoms like hallucinations and paranoid thoughts.
How were mental patients treated in the 1930s?
In the 1930s, mental illness treatments were in their infancy and convulsions, comas and fever (induced by electroshock, camphor, insulin and malaria injections) were common. Other treatments included removing parts of the brain (lobotomies).
How was mental illness treated in the 1970s?
Abstract. In the treatment of mental disorders, the 1970s was a decade of increasing refinement and specificity of existing treatments. There was increasing focus on the negative effects of various treatments, such as deinstitutionalization, and a stronger scientific basis for some treatments emerged.
How many times more likely is a patient to relapse after discontinuing a medication?
No surprise, this increases the risk of relapse. In fact, patients who discontinued medication are nearly five times more likely to have a relapse within five years compared to patients with continued using their medicine.
Does schizophrenia have fewer dosages?
Some next-generation schizophrenia treatments promise to lessen the risk of symptoms, while others require fewer dosages, which could go a long way towards helping those who suffer maintain a consistent regimen. Here’s a look at the latest options.
Does schizophrenia require lifelong treatment?
From long-lasting Injectables to a whole new drug class, here are the five most important cutting-edge treatments. Symptoms may come and go, but schizophrenia requires lifelong treatment. And because many of the traditional medications used to treat the di ... more. sorder cause major side effects, those with schizophrenia can be reluctant ...
How to treat schizophrenia?
Schizophrenia requires lifelong treatment, even when symptoms have subsided. Treatment with medications and psychosocial therapy can help manage the condition. In some cases, hospitalization may be needed. A psychiatrist experienced in treating schizophrenia usually guides treatment.
What is the most common medication for schizophrenia?
Medications are the cornerstone of schizophrenia treatment, and antipsychotic medications are the most commonly prescribed drugs. They're thought to control symptoms by affecting the brain neurotransmitter dopamine.
Why are people with schizophrenia reluctant to take medication?
Because medications for schizophrenia can cause serious side effects, people with schizophrenia may be reluctant to take them. Willingness to cooperate with treatment may affect drug choice. For example, someone who is resistant to taking medication consistently may need to be given injections instead of taking a pill.
Why are second generation antipsychotics preferred?
These newer, second-generation medications are generally preferred because they pose a lower risk of serious side effects than do first-generation antipsychotics . Second-generation antipsychotics include:
How long does it take for antipsychotics to work?
Other medications also may help, such as antidepressants or anti-anxiety drugs. It can take several weeks to notice an improvement in symptoms.
What is the diagnosis of schizophrenia?
Diagnosis of schizophrenia involves ruling out other mental health disorders and determining that symptoms are not due to substance abuse, medication or a medical condition. Determining a diagnosis of schizophrenia may include:
What is the best way to help people with schizophrenia?
Most individuals with schizophrenia require some form of daily living support. Many communities have programs to help people with schizophrenia with jobs, housing, self-help groups and crisis situations. A case manager or someone on the treatment team can help find resources.
How many patients report favorable treatment outcomes for schizophrenia?
The prognosis for patients with schizophrenia is generally unpredictable.2Only 20% of patients report favorable treatment outcomes.12The remaining patients experience numerous psychotic episodes, chronic symptoms, and a poor response to antipsychotics.2
How to diagnose schizophrenia?
A diagnosis of schizophrenia is reached through an assessment of patient-specific signs and symptoms, as described in the Diagnostic and Statistical Manual of Mental Disorders,Fifth Edition (DSM-5).12The DSM-5states that “the diagnostic criteria [for schizophrenia] include the persistence of two or more of the following active-phase symptoms, each lasting for a significant portion of at least a one-month period: delusions, hallucinations, disorganized speech, grossly disorganized or catatonic behavior, and negative symptoms.”12At least one of the qualifying symptoms must be delusions, hallucinations, or disorganized speech.12
What are the side effects of schizophrenia?
Schizophrenia medications can cause a variety of other adverse effects, including the following: 1 Antipsychotic medications with anticholinergic effects have been shown to worsen narrow-angle glaucoma, and patients should be appropriately monitored.49Chlorpromazine is most commonly associated with opaque deposits in the cornea and lens.2Because of the risk of cataracts, eye examinations are recommended for patients treated with quetiapine.50Those using thioridazine at doses exceeding 800 mg daily are at risk of developing retinitis pigmentosa.2 2 Low-potency FGAs and clozapine have been associated with urinary hesitancy and retention.2The incidence of urinary incontinence among patients taking clozapine can be as high as 44% and can be persistent in 25% of patients.2,51 3 FGAs and risperidone have a greater tendency to cause sexual dysfunction compared with SGAs.2,52 4 Treatment with antipsychotics can cause transient leukopenia.2,53 5 The three antipsychotics with the greatest risk for hematological complications are clozapine, chlorpromazine, and olanzapine.54Clozapine is associated with an especially high risk for the development of neutropenia or agranulocytosis.54 6 On rare occasions, dermatological allergic reactions have occurred at approximately eight weeks after the initiation of antipsychotic therapy.2 7 Both FGAs and SGAS can cause photosensitivity, leading to severe sunburn.2 8 Clozapine has been reported to cause sialorrhea in approximately 54% of patients with schizophrenia.2The mechanism of this effect is unknown.2
How many nonadherence rates are there in schizophrenia?
Not only do nonpharmacological therapies fill in gaps in pharmacological treatments; they can help to ensure that patients remain adherent to their medications.18Nonadherence rates in schizophrenia range from 37% to 74%, depending on the report.19Individuals with mental disorders tend to be less adherent for several reasons. They may deny their illness; they may experience adverse effects that dissuade them from taking more medication; they may not perceive their need for medication; or they may have grandiose symptoms or paranoia.2
What are the factors that contribute to schizophrenia?
Environmental and social factors may also play a role in the development of schizophrenia, especially in individuals who are vulnerable to the disorder.1Environmental stressors linked to schizophrenia include childhood trauma, minority ethnicity, residence in an urban area, and social isolation.1In addition, social stressors, such as discrimination or economic adversity, may predispose individuals toward delusional or paranoid thinking.1
What neurotransmitter is involved in schizophrenia?
Another theory for the symptoms of schizophrenia involves the activity of glutamate, the major excitatory neurotransmitter in the brain. This theory arose in response to the finding that phenylciclidine and ketamine, two noncompetitive NMDA/glutamate antagonists, induce schizophrenia-like symptoms.6This, in turn, suggested that NMDA receptors are inactive in the normal regulation of mesocortical dopamine neurons, and pointed to a possible explanation for why patients with schizophrenia exhibit negative, affective, and cognitive symptoms.7
What is the serotonin hypothesis?
The serotonin hypothesis for the development of schizophrenia emerged as a result of the discovery that lysergic acid diethylamide (LSD) enhanced the effects of serotonin in the brain. 1Subsequent research led to the development of drug compounds that blocked both dopamine and serotonin receptors, in contrast to older medications, which affected only dopamine receptors. The newer compounds were found to be effective in alleviating both the positive and negative symptoms of schizophrenia.1
What is the first antipsychotic to be approved for the treatment of schizophrenia?
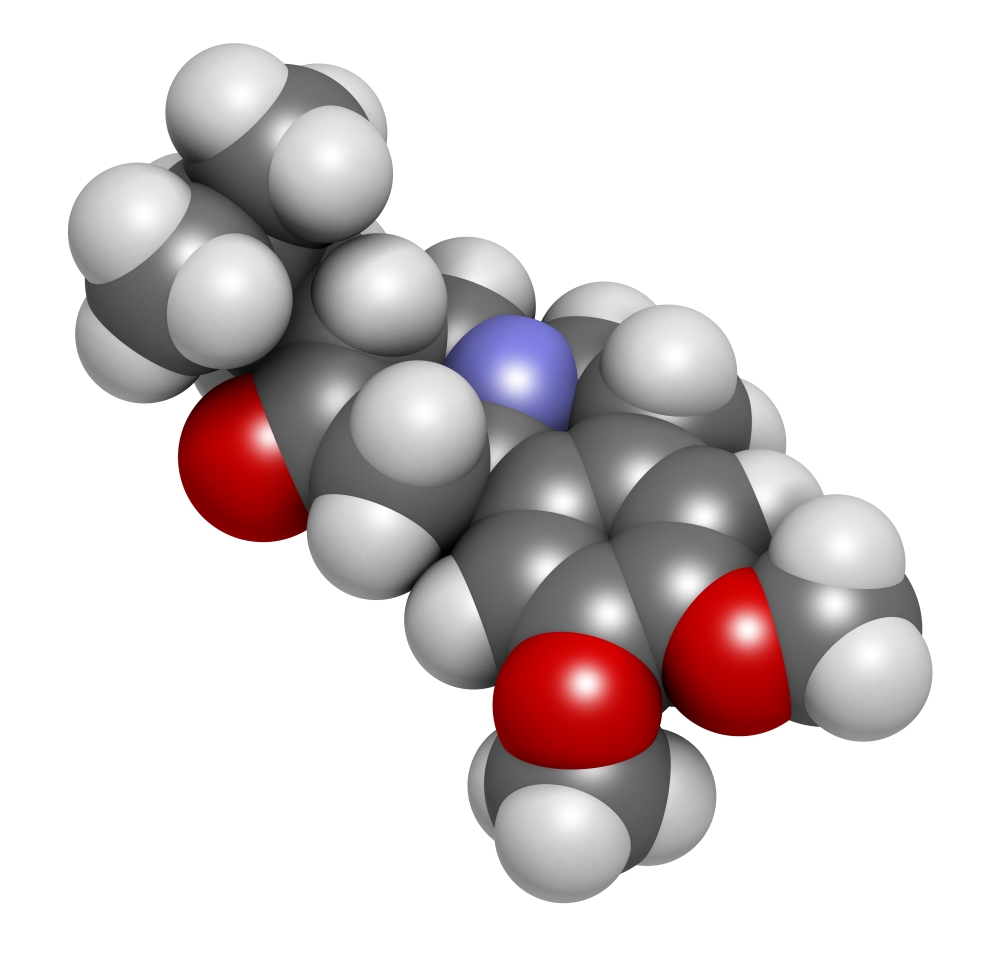
Aripiprazole was the first third-generation antipsychotic to be approved for the treatment of schizophrenia followed by brexpiprazole and then cariprazine. Antipsychotic medicine is effective at relieving positive symptoms like paranoia in about 70% of cases. (Image: I Stock)
What is the role of pharmacogenetics in schizophrenia?
In terms of drug therapy, there is a large arsenal available to medics when encountering first episode schizophrenia and pharmacogenetics aims to help better prescribing by trying to predict which patients will do well on each type of medicine.
What is the third generation of a drug?
The most recent development is the so-called third generation drugs such as aripiprazole, brexpiprazole and cariprazine. These drugs are also known as ‘D2/D3 partial agonists’ or dopamine-serotonin stabilisers’. The novel mode of action of these drugs is that in areas where dopamine and serotonin activity is low, ...
What is the second generation of serotonin?
The second-generation drugs such as olanzapine and quetiapine, expanded the scope of drug therapy to include another type of receptor triggered by the chemical messenger serotonin, in an attempt to affect the negative and cognitive symptoms. The most recent development is the so-called third generation drugs such as aripiprazole, ...
Is antipsychotics good for schizophrenia?
Although there is now better access to the talking therapies in the UK, antipsychotics remain the mainstay of treatment in the NHS. (See our information sheet on Modern Treatments for a broader discussion of the treatments available) This is because we know that they are effective in controlling positive symptoms like hallucinations and delusions. In this piece Rob Foster looks at some recent developments in the use of antipsychotic medicines in schizophrenia and particularly at the new drugs which have come to be known as the third-generation antipsychotics.
Which generation of antipsychotics have better side effects?
Third generation antipsychotics appear to have better side effect profiles particularly with issues like sedation. (Image: Elena Rostunova on Shutterstock)
Do antipsychotics require close monitoring?
There are no major changes in the function of bodily systems that require extremely close monitoring as with some previous generations drugs however, as with any long-term antipsychotic use, annual or six-monthly bloods, baseline observations (pulse, BP, temperature etc) and ECG (trace of the hearts electrical rhythm) is prudent.
Why are twin studies of behavioral characteristics-likethose defining schizophrenia fundamentally flawed?
Journal of Mind andBehavior, 19, 325-358.Joseph points out that all twin studies of behavioral characteristics-likethose defining "schizophrenia" are fundamentally flawed because identicaltwins have been clearly shown to be raised more similarly than are non-identical ones.
Was moral treatment unscientific?
Eventually some physicians claimed “moral treatment” was“unscientific” and “By 1880, moral treatment had been completelyeradicated . Insanity was again labeled a physical disease, and physicaltreatments were reintroduced.” i.e:“Prolonged immersion in very hot or very cold water, needle showers,Being wrapped in wet sheet packs and left to be squeezed like a viceasthey dried, Surgery such as hysterectomy, tonsillectomy, colectomy,cholysytectomy, appendectomy, orchiectomy.
What is the main treatment for schizophrenia?
Medication is currently the main method of treating schizophrenia, and the primary type of medication is a class of drugs called antipsychotics. These are designed to dampen the psychotic, or positive, symptoms of the illness. Many people experience at least some degree of success with the results of their current medications.
What is the new medication for schizophrenia?
New Schizophrenia Medication: Cannabinoids. Cannabinoid (CBD) treatment is a potential new schizophrenia medication. Cannabinoids are part of the marijuana plant but are different than tetrahydrocannabinol (THC), the psychoactive compound responsible for the high that many people associate with marijuana ...
How many new schizophrenia medications are there?
Of the almost three dozen new schizophrenia medications, several are completely new and are progressing through the phases of research, a process that can take years. These new medications offer the promise of improved negative and cognitive symptoms as well as milder side effects. One of the new medications making progress through ...
How do antipsychotics work?
They have very recently discovered how medications “dock” in the brain—how they bind to their targets in the brain .
How long is the early intervention program for schizophrenia?
This early intervention program is typically a two-year program that focuses on: Socialization. Family therapy/family relationships.
What is an antipsychotic program?
Antipsychotic medication when necessary. The program is therapeutic in nature and focuses heavily on counseling for individuals and families. Program developers strive to help adolescents and young adults live well and lead an independent (with support), productive life in spite of schizophrenia.
Does CBS help with schizophrenia?
CBS works in the brain differently than antipsychotics, and it potentially can reduce both positive and negative symptoms of schizophrenia. GW Pharmaceuticals is developing a CBD treatment, one that isn’t medical marijuana but a schizophrenia treatment medication It has been undergoing human trials and has great potential as a new schizophrenia treatment.
ABSTRACT
Although antipsychotics have been available for almost 70 years and greatly improved outcomes for individuals with schizophrenia, all currently available options derive their efficacy from blockade of dopaminergic receptors. However, this mechanism of action leaves many symptoms unresolved and is associated with a significant side effect burden.
A Promising New Treatment Target: Overview of a Randomized Controlled Trial of Ulotaront (SEP-363856) for Acute Exacerbation of Schizophrenia
A lthough several new antipsychotics have become available in the 7 decades since the introduction of chlorpromazine, all of these treatments have relied primarily on the same mechanism—blockade of postsynaptic dopamine D2 receptors.
The Pathophysiology of Schizophrenia: A Brief Overview
S chizophrenia is a chronic disorder in which symptoms typically emerge in late adolescence or early adulthood. For most patients, these symptoms will progress through several clinical stages of worsening severity ( Figure 3 ), 4 and they occur in clusters across multiple functional domains.
Current Paradigm for Schizophrenia Treatment: D2 Receptor Blockade
T he first antipsychotic drug was discovered almost 70 years ago. 35 In the intervening years, more than 20 different antipsychotics have been developed, and this high number would seem to indicate that patients and providers have many treatment options from which to choose.
New Mechanisms of Action for the Treatment of Schizophrenia
T hat only postsynaptic dopamine blockers are available to treat schizophrenia is quite detrimental for this population because of the adverse effects and inefficacy commonly associated with these agents.
Clinical Points
Schizophrenia symptoms typically emerge in late adolescence or early adulthood, but brain changes underlying the symptoms begin during gestation and continue through the lifespan. Many symptoms are thought to involve dysfunction in neural networks that are essential for processing information and controlling behavior.
Additional Resources
See a short video explaining how trace amine–associated receptor 1 (TAAR1) affects neurotransmitters in the brain. This video is a publicly available educational resource provided by Sunovion Pharmaceuticals Inc. It was produced prior to and independent of the JCP InfoPack “Emerging Treatments in Schizophrenia.”
What is the treatment for schizophrenia?
Electrical Convulsive Treatment (ECT) was used as an effective treatment for schizophrenia when scientists realized that by inducing a seizure, psychotic symptoms resolved . ECT continues to be utilized for cases of schizophrenia that do not respond to medications. In fact, catatonic schizophrenia responds best to ECT. In this case, the disease affects cognitive functioning so much that the person may be unable to communicate, eat or drink, or even move.
What was the first antipsychotic for schizophrenia?
With the discovery of antipsychotics, the future of patients with schizophrenia brightened significantly. The first antipsychotic discovered was chlorpromazine (Thorazine). Numerous antipsychotics were derived from its formulation and were aimed to treat primarily the positive symptoms of schizophrenia. Unfortunately, negative symptoms were left untreated or were worsened by the treatment. This greatly affected compliance since feeling slowed, numbed or dulled-down caused many patients to discontinue their treatment. With the discovery of clozapine (Clozaril), patients that did not respond to first generation antipsychotics were given an alternative treatment that is highly effective. One additional advantage of clozapine was and continues to be its protection against suicidal thoughts or tendencies. Treatment with clozapine requires monitoring the body's white blood cells because there’s a risk levels may get too low on this medication.
What are some examples of atypical antipsychotics?
Atypical antipsychotics are more tolerable and have fewer side effects than other treatments. Some examples include risperidone (Risperdal), ziprasidone (Geodon), olanzapine (Zyprexa), aripiprazole (Abilify), asenapine (Saphris), paliperidone (Invega), bexpiprazole (Rexulti), and quetiapine (Seroquel). All of these medications have different side effects; however they all require close monitoring of blood sugars, cholesterol, blood pressure, and weight. This is due to the risk of what we call “metabolic syndrome,” which can lead to hypertension, diabetes, and high cholesterol over time if not monitored and addressed with diet and nutrition.
