Antibiotics are the mainstay of treatment for acute bacterial prostatitis. Full response and resolution are expected. Radiologic or surgical interventions are usually not required for acute prostatitis unless complicated by abscess formation.
Full Answer
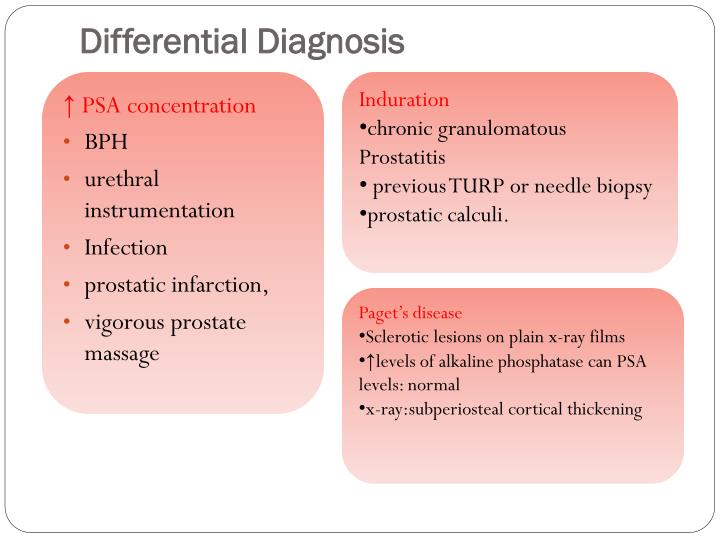
How are peripheral hypoechoic lesions of the prostate evaluated?
Peripheral hypoechoic lesions of the prostate: evaluation with color and power Doppler ultrasound Evaluation of peripheral hypoechoic lesions of the prostate with color and power Doppler may enhance the diagnostic capability of transrectal ultrasound.
What are my treatment options for prostate cancer?
Men with slow-growing prostate cancers may choose active surveillance. With this approach, you can postpone, and sometimes completely forego, treatments. Your healthcare provider can discuss the best treatment option for you based on your Gleason score and Group Grade.
What are the treatment options for prostate calcification?
No medical treatment is required when prostate calcification is asymptomatic. Symptoms may occur in the setting of superimposed infection in which antibiotics are the mainstay of treatment. When obstructive or chronic infective symptoms occur, surgical treatment may be needed. In those who are symptomatic, calculi may be removed transurethrally.
What are the treatment options for prostate abscess?
These findings are consistent with a prostate abscess that was subsequently successfully treated with a combination of antibiotics and percutaneous interventional radiology catheter drainage (C). Magnetic Resonance Imaging.
What is the treatment for hypoechoic lesion?
Surgery. Surgery may be the best option to remove larger hypoechoic masses. Benign growths can cause pain, obstruction, and other complications. In some cases, a benign mass may become cancerous, or rupture and cause bleeding inside the body.
What is hypoechoic lesion in prostate?
Hypoechoic lesions in the peripheral zone of the prostate gland are one of the commonest abnormalities at transrectal ultrasonography (TRUS). 90% of all carcinomas originating in the peripheral zone present as a hypoechoic lesion. Hypoechogenicity though is not specific, as many benign lesions are also hypoechoic.
What does it mean when you have a lesion on your prostate?
Two important histopathological prostatic lesions are benign prostatic hyperplasia and Prostatic carcinoma. These lesions cause enlargement of prostate gland, constricting the urethra and thus causing various urinary symptoms.
How are prostate lesions removed?
A common surgical approach to prostatectomy includes making a surgical incision and removing the prostate gland (or part of it). This may be accomplished with either of two methods, the retropubic or suprapubic incision (lower abdomen), or a perineum incision (through the skin between the scrotum and the rectum).
What does hypoechoic lesion mean?
A hypoechoic nodule, sometimes called a hypoechoic lesion, on the thyroid is a mass that appears darker on the ultrasound than the surrounding tissue. This often indicates that a nodule is full of solid, rather than liquid, components.
What is the normal size of hypoechoic lesion?
Considerable attention is often given toward identifying small hypoechoic (less than 0.2 cm3) lesions at the time of transrectal ultrasound-guided prostate biopsy.
Can a prostate lesion be removed?
Most often, prostatectomy is done to treat localized prostate cancer. It may be used alone, or in conjunction with radiation, chemotherapy and hormone therapy. Radical prostatectomy is surgery to remove the entire prostate gland and surrounding lymph nodes to treat men with localized prostate cancer.
What size prostate lesions are cancerous?
Conclusions: These data indicate that clinically significant prostate cancer in lesions less than 0.65 cm and greater than 1.70 cm may be characterized with a single targeted biopsy core, sparing 33.5% of lesions (21% patients) a double core targeted biopsy.
Does size of prostate lesion matter?
Lesion diameter ≥15 mm was an independent risk factor for adverse prostatectomy pathology. Lesion diameter ≥20 mm, but not ≥15 mm, was a significant risk factor for lymph node metastasis.
Is prostate surgery a major surgery?
Prostate removal is major surgery, so expect some soreness and pain. You'll receive IV pain medications at first, and your doctor may prescribe you pain medication to use at home. You will also have a urinary catheter in place for about the first week, which you might find uncomfortable.
What size of prostate requires surgery?
TURP developed itself to become the gold standard of surgical treatment for medium sized prostates. The EAU guidelines, based on grade A evidence, recommends TURP for prostates between 35 and 80 ml. Over that limit, open surgery seems to remain the only option for treating BPH, according to available clinical evidence.
What is the latest treatment for enlarged prostate 2021?
Physicians at UC San Diego Health are now offering prostate artery embolization (PAE) as a new treatment option for men with benign prostatic hyperplasia (BPH), or an enlarged prostate. The minimally invasive procedure is an alternative to surgery, with no hospital stay, little operative pain and lower cost.
Can Prostate Cancer Be Found Early
Screening tests are available to find prostate cancer early, but government guidelines don’t call for routine testing in men at any age. The tests may find cancers that are so slow-growing that medical treatments would offer no benefit. And the treatments themselves can have serious side effects.
What Are Grade Groups
Grade Groups are a new way to grade prostate cancer to address some of the issues with the Gleason grading system.
How Prostate Cancer Is Diagnosed And Staged
Cancer staging helps you and your doctor understand how advanced your cancer is and how much it has spread at the time of diagnosis. Knowing your cancer stage also helps your doctor determine the best treatment options for you and estimate your chance of survival.
What Does It Mean When There Are Different Core Samples With Different Gleason Scores
Cores may be samples from different areas of the same tumor or different tumors in the prostate. Because the grade may vary within the same tumor or between different tumors, different samples taken from your prostate may have different Gleason scores.
What Are The Stages Of Prostate Cancer
Your healthcare provider uses the Gleason score and Grade Groups to stage prostate cancer based on its projected aggressiveness. To get this information, the pathologist:
How Common Is Prostate Cancer
About one in nine men will receive a prostate cancer diagnosis during his lifetime. Prostate cancer is second only to skin cancer as the most common cancer affecting males. Close to 200,000 American men receive a diagnosis of prostate cancer every year. There are many successful treatments and some men dont need treatment at all.
Features Of Pin Cells
Basal cellspecific monoclonal antibodies directed against highmolecular weight keratin are used to identify HGPIN cells. Normal prostatic epithelial cells are consistently stained with these antibodies, showing a continuous, intact, circumferential basal cell layer. Cancer cells have lost their receptors for these antibodies.
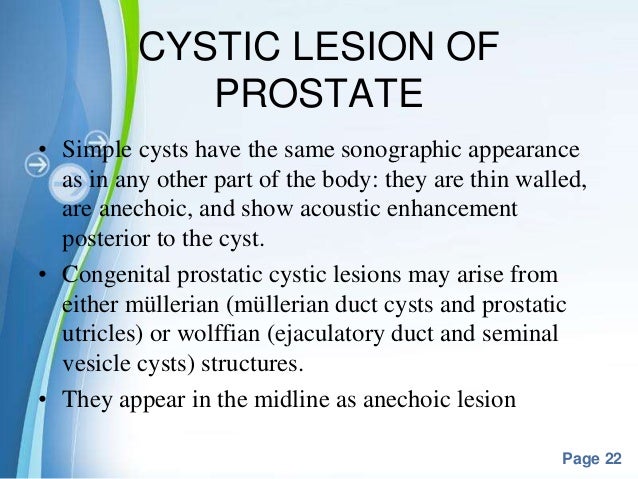
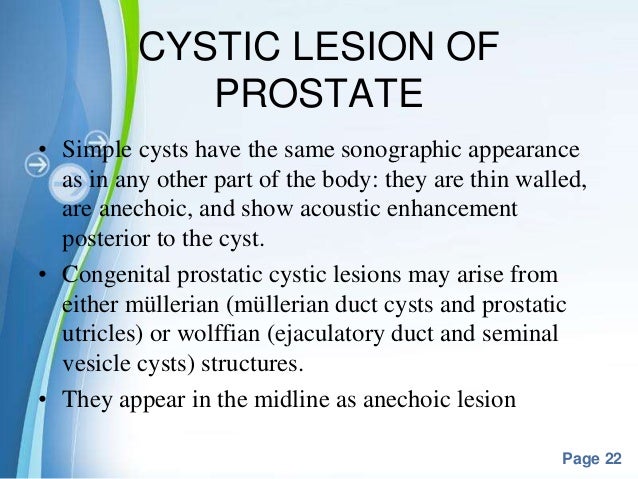
What is the best imaging for prostate?
The most commonly used diagnostic imaging techniques for prostate evaluation are transrectal ultrasound (TRUS) and MRI. Benign findings such as cysts and calcifications are typically incidental, usually found on routine investigation for other conditions; most benign processes such as BPH and prostatitis require little investigation. TRUS can provide high-resolution images of the prostate and real-time guidance for intervention such as biopsy, aspiration, and drainage, without the use of radiation. Magnetic resonance imaging (MRI) accurately delineates the internal prostatic anatomy but is not routinely used for the investigation of benign prostate lesions owing to its high cost and relatively limited availability. Relative to these modalities, radiography and computed tomography (CT) have limited roles in the evaluation of most prostate processes.
Why do you need a CT scan for prostate abscess?
Ultrasound and MRI are preferred to CT because of superior soft tissue contrast resolution.
How does bacteria ascend to the prostate?
Bacteria may ascend to the prostate by reflux of infected urine into the prostatic duct, by lymphatic or hematogenous dissemination, or during interventions such as prostat ic biopsy. Emphysematous prostatitis occurs secondary to infection with gas-forming organisms; while rare, it is associated with high mortality.
What is the purpose of MRI in prostate?
Magnetic resonance imaging (MRI) accurately delineates the internal prostatic anatomy but is not routinely used for the investigation of benign prostate lesions owing to its high cost and relatively limited availability.
What is the diagnosis of acute bacterial prostatitis?
The diagnosis of acute bacterial prostatitis is based primarily on clinical findings, in association with positive results of urinalysis and urine culture.
Where does calcification occur in the prostate?
Prostate calcifications are larger than prostate calculi. Calculi occur in the lumen of prostate acini. Calcification occurs in the parenchyma and may be focal or diffuse, involve a small or large area, and occur periurethrally or at the surgical capsule.
Is the prostate a focal or diffuse?
The prostate may be focally or diffusely involved. In acute infection, the prostate enlarges secondary to infection and inflammation. An increased number of inflammatory cells is seen in prostate biopsy specimens.