
Treatment
- Uncomplicated diverticulitis. If your symptoms are mild, you may be treated at home. ... Antibiotics to treat...
- Complicated diverticulitis. If you have a severe attack or have other health problems, you'll likely need to be...
- Surgery. Primary bowel resection. The surgeon removes diseased segments of your intestine and then reconnects the...
- Antibiotics (for bacterial overgrowth)
- Hospitalization (for complications such as severe bleeding)
- Endoscopic treatment (involving removal of the diverticula during an endoscopic procedure)7
What are foods to eat and not to eat with diverticulitis?
Small bowel diverticulosis is an uncommon condition which is associated with numerous possible complications. While endoscopy is playing an increasingly large role in management, surgical resection remains the treatment of choice for most complications. A high index of suspicion is needed in order to diagnose this entity.
What to eat when recovering from diverticulitis?
Apr 19, 2022 · Treatment Uncomplicated diverticulitis. If your symptoms are mild, you may be treated at home. ... Antibiotics to treat... Complicated diverticulitis. If you have a severe attack or have other health problems, you'll likely need to be... Surgery. Primary bowel resection. The surgeon removes ...
Which home remedies can help treat diverticulitis?
Small bowel diverticulosis is a rare disease of gastrointestinal tract that occurs most frequently in older patients. Since this disease can be asymptomatic, for a long time, the diagnosis rarely is made in the preoperative period. ... [Diverticulosis of the small intestine] Bratisl Lek Listy. 1995 Aug;96(8):442-6. ... The surgical treatment ...

What is the best treatment for diverticulosis?
How do doctors treat diverticulosis?
How do you get rid of diverticulosis?
What causes diverticulitis in small intestine?
What causes diverticulosis to flare up?
What are the two main causes of diverticulosis?
What foods should be avoided with diverticulosis?
- Whole grains.
- Fruits and vegetables with the skin and seeds.
- Nuts and seeds.
- Beans.
- Popcorn.
How long can diverticulosis last?
Does diverticulosis affect bowel movements?
Can you have diverticulosis of small intestine?
What does poop look like with diverticulitis?
Color: The stool may be bright red, maroon, or black and tarry, which indicates the presence of blood. Stools may contain more mucus than normal. Odor: The stool odor may be increasingly foul compared to the typical smell.
Can you have diverticulosis in small bowel?
What is the best treatment for diverticulitis?
Surgery. You'll likely need surgery to treat diverticulitis if: You have a complication, such as a bowel abscess, fistula or obstruction, or a puncture (perforation) in the bowel wall. You have had multiple episodes of uncomplicated diverticulitis. There are two main types of surgery:
How to treat diverticulitis?
Treatment generally involves: Intravenous antibiotics. Insertion of a tube to drain an abdominal abscess, if one has formed.
How long after diverticulitis can you have a colonoscopy?
Your doctor may recommend colonoscopy six weeks after you recover from diverticulitis, especially if you haven't had the test in the previous year. There doesn't appear to be a direct link between diverticular disease and colon or rectal cancer.
What is the opening in the abdominal wall?
An opening (stoma) in your abdominal wall is connected to the healthy part of your colon. Waste passes through the opening into a bag. Once the inflammation has eased, the colostomy may be reversed and the bowel reconnected.
What is the best way to remove a weakened immune system?
You have a weakened immune system. There are two main types of surgery: Primary bowel resection. The surgeon removes diseased segments of your intestine and then reconnects the healthy segments (anastomosis). This allows you to have normal bowel movements.
What tests are done to rule out pelvic disease?
Women generally have a pelvic examination as well to rule out pelvic disease. After that, the following tests are likely: Blood and urine tests, to check for signs of infection. A pregnancy test for women of childbearing age, to rule out pregnancy as a cause of abdominal pain. A liver enzyme test, to rule out liver-related causes of abdominal pain.
Can diverticulitis be diagnosed during an acute attack?
Diverticulitis is usually diagnosed during an acute attack. Because abdominal pain can indicate a number of problems, your doctor will need to rule out other causes for your symptoms.
What is the approach to management of complicated small bowel diverticula?
The approach to management of complicated small bowel diverticula involves initiation of medical and supportive management. Surgical consultation must be performed promptly.
What is the best treatment for diverticulum bleeding?
Laparotomy may be indicated as an emergency therapy for continuing bleeding or as elective treatment if bleeding responds to conservative management. The site of the diverticulum should be identified with angiography and the area should be injected with methylene blue or India ink in order to stain the mesentery involving the bleeding diverticulum.
What is the role of diet in diverticulosis?
The role of diet is not clear. A high-fiber diet that improves bowel motility and is used in colonic diverticulosis may be beneficial.
Why do you need to be hospitalized for diverticulitis?
For diverticulitis, patients often require hospitalization because preoperative diagnosis of small bowel diverticulitis is difficult. Initial interventions include the following:
Where are intraluminal diverticula found?
Intraluminal diverticula are observed in the duodenum and can be complicated by intestinal obstruction and biliary and pancreatic diseases. A higher complication rate is associated with jejunoileal diverticulosis and, as such, may justify a less conservative approach to its management.
When to use push enteroscopy?
Push enteroscopy or double balloon enteroscopy should be used once a lesion amenable to therapeutic intervention has been identified. Inpatient treatment is indicated only in patients presenting with complications. The duration of such admission depends on the nature of the complication and the interventions rendered.
Is asymptomatic diverticula left alone?
The general recommendation favors a conservative approach to the management of asymptomatic diverticula. These lesions are generally left alone unless they can be related to diseases. In certain locations, diverticula are associated with special complications. For example, periampullary diverticula can be associated with pancreatitis, cholangitis, or recurrent choledocholithiasis after cholecystectomy.
Which part of the small intestine is affected by diverticula?
The most common part of the small intestine to be affected by diverticula is the duodenum (the first segment). 1 . The function of the duodenum is to receive food from the stomach, in addition to bile and pancreatic juices from the gallbladder and pancreas.
Where are diverticula located?
Extraluminal diverticula protrude outside the wall of the duodenum. Most of these are located in the periampullary region. 3
What is the condition called when you have a bulging sac in your small intestine?
Symptoms. Causes. Diagnosis. Treatment. Small bowel diverticula (also called small intestine diverticular disease) is a condition involving bulging sacs in the wall of the small bowel. Diverticula can occur in any portion of the gastrointestinal (GI) tract. They are much less common in the small bowel than in the colon (large intestine).
What is the name of the hole in the GI system that can occur anywhere?
Duodenal obstruction (partial or complete blockage of the small bowel, which is very rare) A serious condition that may result from extraluminal diverticula is perforation (a hole that can occur anywhere in the GI system).
How many people have complications from duodenal diverticula?
The rate of complications from duodenal diverticula is high. In fact, according to a 2012 study, 10% to 12% of those with duodenal diverticulum experience complications, and 46% of those with jejunal diverticulum have complications. 6
What are the symptoms of juxtapapillary diverticula?
The primary symptom is abdominal pain. Juxtapapillary diverticula may cause several complications, including: Pancreatitis: Inflammation of the pancreas. Cholangitis: Inflammation of the bile ducts. Choledocholithiasis: Bile duct stones, which can occur even after a gallbladder removal.
What are the different types of duodenal diverticula?
Many are categorized according to where they are located in the gastrointestinal tract. These include extraluminal, intraluminal, and juxtapapillary diverticula.
What antibiotics are prescribed for diverticulitis?
If your diverticulitis is mild, your healthcare provider will prescribe an oral antibiotic, such as metronidazole (Flagyl®), trimethoprim-sulfamethoxazole (Bactrim®), ciprofloxacin (Cipro®) or amoxicillin and clavulanic acid (Augmentin®).
What to do if you have diverticulitis and you have a repeat bout?
If your diverticulitis is severe, you have rectal bleeding or are having a repeat bout of diverticulitis, you may be admitted to the hospital to receive intravenous (IV) antibiotics, IV fluids or possibly be considered for surgery.
How long does it take for diverticulitis to heal?
Most people who have diverticulitis will recover with about a seven to 10-day course of antibiotics and rest. Severe complication of diverticulitis occur in about the following percent of people: perforation of the colon (1% to 2% of patients), obstruction (rare), fistula (14%) or abscess (30%).
What is the name of the disease that occurs in the large intestine?
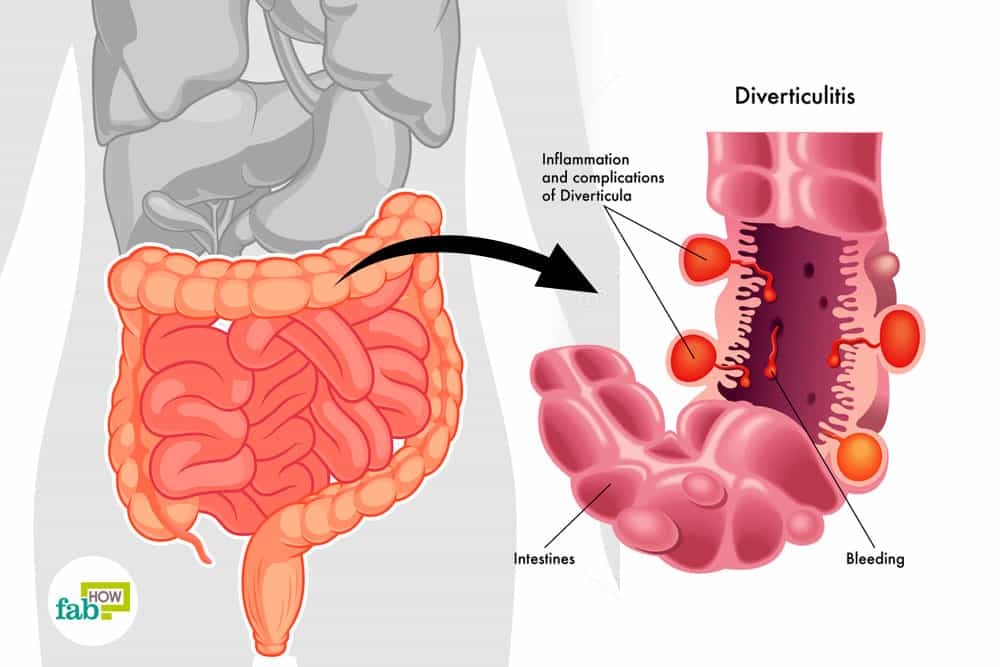
Diverticulosis and diverticulitis are two conditions that occur in your large intestine (also called your colon). Together they are known as diverticular disease. Both share the common feature of diverticula. Diverticula are one or more pockets or bulges that form in the wall of your colon.
What is the difference between diverticulosis and diverticulitis?
Diverticulosis is “the presence of” and diverticulitis is “inflammation and infection of” one or more diverticula (bulges in your colon wall). Diverticulosis is common , doesn’t cause symptoms or need treatment . Mild diverticulitis is treated with antibiotics. Surgery is needed if problems develop. A high fiber diet, exercise and drinking lots of water can help prevent.
Why does diverticulitis start?
Again, scientists aren’t sure what causes diverticulitis, but they think the infection starts due to the bacteria in stool that gets pushed into the diverticula. Another theory is that the walls of the diverticula itself erode from the increased pressure on the colon walls.
How many people with diverticulosis have diverticulitis?
Up to 30% of people with diverticulosis do develop diverticulitis. Between 5% and 15% will develop rectal bleeding.
How to treat diverticulitis?
Mild diverticulitis can be treated with rest, changes in your diet and antibiotics. Severe or recurring diverticulitis may require surgery.
How to reduce the risk of diverticulitis?
Lack of exercise. Vigorous exercise appears to lower your risk of diverticulitis. Diet high in animal fat and low in fiber. A low-fiber diet in combination with a high intake of animal fat seems to increase risk, although the role of low fiber alone isn't clear. Certain medications.
What is the name of the condition where a pouch of intestines is inflamed?
Open pop-up dialog box. Close. Diverticulosis and diverticulitis. Diverticulosis and diverticulitis. Diverti culosis occurs when small, bulging pouches (diverticula) develop in your digestive tract. When one or more of these pouches become inflamed or infected, the condition is called diverticulitis. Diverticula are small, bulging pouches that can ...
What are the complications of diverticulitis?
About 25% of people with acute diverticulitis develop complications, which may include: 1 An abscess, which occurs when pus collects in the pouch. 2 A blockage in your bowel caused by scarring. 3 An abnormal passageway (fistula) between sections of bowel or the bowel and other organs. 4 Peritonitis, which can occur if the infected or inflamed pouch ruptures, spilling intestinal contents into your abdominal cavity. Peritonitis is a medical emergency and requires immediate care.
Where are diverticula found?
Diverticula are small, bulging pouches that can form in the lining of your digestive system. They are found most often in the lower part of the large intestine ( colon). Diverticula are common, especially after age 40, and seldom cause problems. The presence of diverticula is known as diverticulosis (die-vur-tik-yoo-LOE-sis).
What is the term for a bowel infection that occurs when pus collects in the pouch?
An abscess, which occurs when pus collects in the pouch. A blockage in your bowel caused by scarring. An abnormal passageway (fistula) between sections of bowel or the bowel and other organs. Peritonitis, which can occur if the infected or inflamed pouch ruptures, spilling intestinal contents into your abdominal cavity.
What drugs are associated with diverticulitis?
Several drugs are associated with an increased risk of diverticulitis, including steroids, opioids and nonsteroidal anti-inflammatory drugs, such as ibuprofen (Advil, Motrin IB, others) and naproxen sodium (Aleve).
How old do you have diverticulosis?
Diverticulosis is common in people over age 60. It doesn’t happen often to those younger than 30. Experts think the pouches show more with age. Men might get it more than women.
How to get rid of gas in stomach?
This will depend on how much your doctor thinks fiber (or the lack of it) might play into your condition. Fiber-rich foods reduce gas and pain in your stomach.
What is the term for a pouch that forms in the walls of the digestive tract?
What Is Diverticulosis ? Diverticulosis is when pockets called diverticula form in the walls of your digestive tract. The inner layer of your intestine pushes through weak spots in the outer lining. This pressure makes them bulge out, making little pouches.
Can probiotics help with diverticulosis?
Research is still being done on how probiotics -- live bacteria that live in your stomach and intestines -- can help fight diverticulosis symptoms. Yogurt and supplements are good sources. It’s important to check with your doctor before taking supplements of any kind.
Can diverticulosis cause more problems?
Having diverticulosis doesn’t mean you’ll have more problems , but they can happen. For example:
Do people with diverticulosis show signs?
Most people who have diverticulosis don’t show any signs. Those who do might have:
Can a muscle spasm cause diverticulosis?
Doctors aren’t sure. Some think muscle spasms or strain (like when you have a bowel movement) make pressure build in your colon and push against the lining. In the past, most experts thought not eating enough fiber -- which is found in many fruits and vegetables, grains, and beans -- led to diverticulosis.
How to treat diverticulitis with no other symptoms?
If you have diverticulitis with mild symptoms and no other problems, a doctor may recommend that you rest, take oral antibiotics. NIH external link. , and follow a liquid diet for a period of time. If your symptoms ease after a few days, the doctor will recommend gradually adding solid foods back into your diet.
What to do if your large intestine is blocked?
If your large intestine is completely blocked, you will need emergency surgery, with possible colon resection. Partial blockage is not an emergency, so you can schedule the surgery or other corrective procedures.
What is the procedure for a colon resection?
Colon resection. If your bleeding does not stop, a surgeon may perform abdominal surgery with a colon resection. In a colon resection, the surgeon removes the affected part of your colon and joins the remaining ends of your colon together. You will receive general anesthesia.
What is the procedure that stops bleeding?
colonoscopy. During a colonoscopy, a doctor can insert special tools through the colonoscope to stop the bleeding.
What to do if you have a perforation in your colon?
If you have a perforation, you will likely need surgery to repair the tear or hole. Additional surgery may be needed to remove a small part of your colon if the surgeon cannot repair the perforation.
How to rest colon?
a clear liquid diet for a short time to rest the colon. Your doctor may suggest slowly adding solid foods to your diet as your symptoms improve.
Can a colon resection be done right away?
In some cases, during a colon resection, it may not be safe for the surgeon to rejoin the ends of your colon right away. In this case, the surgeon performs a temporary colostomy. Several months later, in a second surgery, the surgeon rejoins the ends of your colon and closes the opening in your abdomen.
Prehospital Care
Medical Management
- Abdominal pain without clinical evidence of diverticulitis or intestinal obstruction requires no specific treatment. Patients benefit from the use of bulk-forming agents, such as fiber, bran, and cellulose products. Intractable pain associated with anemia and jejunal loop dilatation on radiograph should heighten concern for jejunal diverticulosis. ...
Consultations
- Consultation with a general surgeon is indicated for all patients requiring surgical management. A gastroenterologist assists with diagnosis and follow-up strategy and performs both diagnostic and therapeutic endoscopy
Diet and Activity
- The role of diet is not clear. A high-fiber diet that improves bowel motility and is used in colonic diverticulosis may be beneficial. No restriction of activity is indicated.
Management of Complications
- The approach to management of complicated small bowel diverticula involves initiation of medical and supportive management. Surgical consultation must be performed promptly. GI bleeding and/or hemorrhage Note the following: 1. Patient is treated with intravenous (IV) fluid and blood products as necessary. 2. Diagnostic workup is usually completed in the intensive car…
Anatomy and Terminology
Types of Small Intestine Diverticula
Small Bowel Diverticula Symptoms
Causes
Diagnosis
Treatment
- For those with no symptoms, conservative treatment is often recommended for small bowel diverticula.2 Conservative treatment may include encouraging intake of fluids and the use of bulk-forming agents (such as fiber and bran and cellulose supplements). A high-fiber diet may be recommended to improve the motility of the GI system. The condition wi...
A Word from Verywell