Besides counseling for avoidance of exogenous steroids (like inhaled steroids for lung diseases) and enrollment to physical therapy, they were referred to weight loss programs and neurosurgery consultations (weight loss of 15 kg or more required [ 3 ]), decompressive laminectomy A laminectomy is a surgical procedure that removes a portion of the vertebral bone called the lamina, which is the roof of the spinal canal. It is a major spine operation with residual scar tissue and may result in postlaminectomy syndrome. Depending on the problem, smaller alternatives, …Laminectomy
How long does an epidural last for spinal stenosis?
You should feel the full effects of the steroids about 3 to 5 days after your procedure. If they work properly, epidural injections provide pain relief for up to six months. If you do not experience pain relief within the first two weeks of the procedure, your doctor may recommend an additional injection.
Can spinal decompression help the effects of spinal stenosis?
Decompression is a surgery that aims to give nerves more room and alleviate the pressure on them. Spinal stenosis can be caused by: Spinal stenosis decompression surgery is usually an option when nonsurgical management techniques have not produced results.
What are the symptoms of spinal epidural hematoma?
Spinal Subdural or Epidural Hematoma
- Symptoms and Signs. Symptoms of a spinal subdural or epidural hematoma begin with local or radicular back pain and percussion tenderness; they are often severe.
- Diagnosis. ...
- Treatment. ...
- Key Points. ...
Is Spinal decompression safe for the Osteoporosis Patient?
Spinal decompression therapy is not only safe but also highly recommended for some patients. Formation of hernias is often to blame for lower back pain, followed by bulging of discs and degeneration of the vertebrae. Some of the situations that can be catalysts of lower back pain include:

Can epidural lipomatosis go away?
The prognosis of idiopathic spinal epidural lipomatosis is favorable after surgical intervention and no cases of recurrence have been reported following surgery.
What causes epidural lipomatosis?
Exogenous steroid use is the most common cause of epidural lipomatosis (non-neoplastic overgrowth of adipose tissue within the epidural space of spinal canal[1]) and accounts for about 55% of cases. [2] The less common causes are obesity (25%), Cushing's syndrome (3%) and idiopathic (17%).
Is epidural lipomatosis progressive?
Spinal epidural lipomatosis is a rare and complex disor- der that can present with progressive neurological deficits. Hypertrophy of adipose tissue located in the spinal epidu- ral space is most commonly associated with long-term steroid use but can be observed in patients with a number of other conditions.
Is epidural lipomatosis rare?
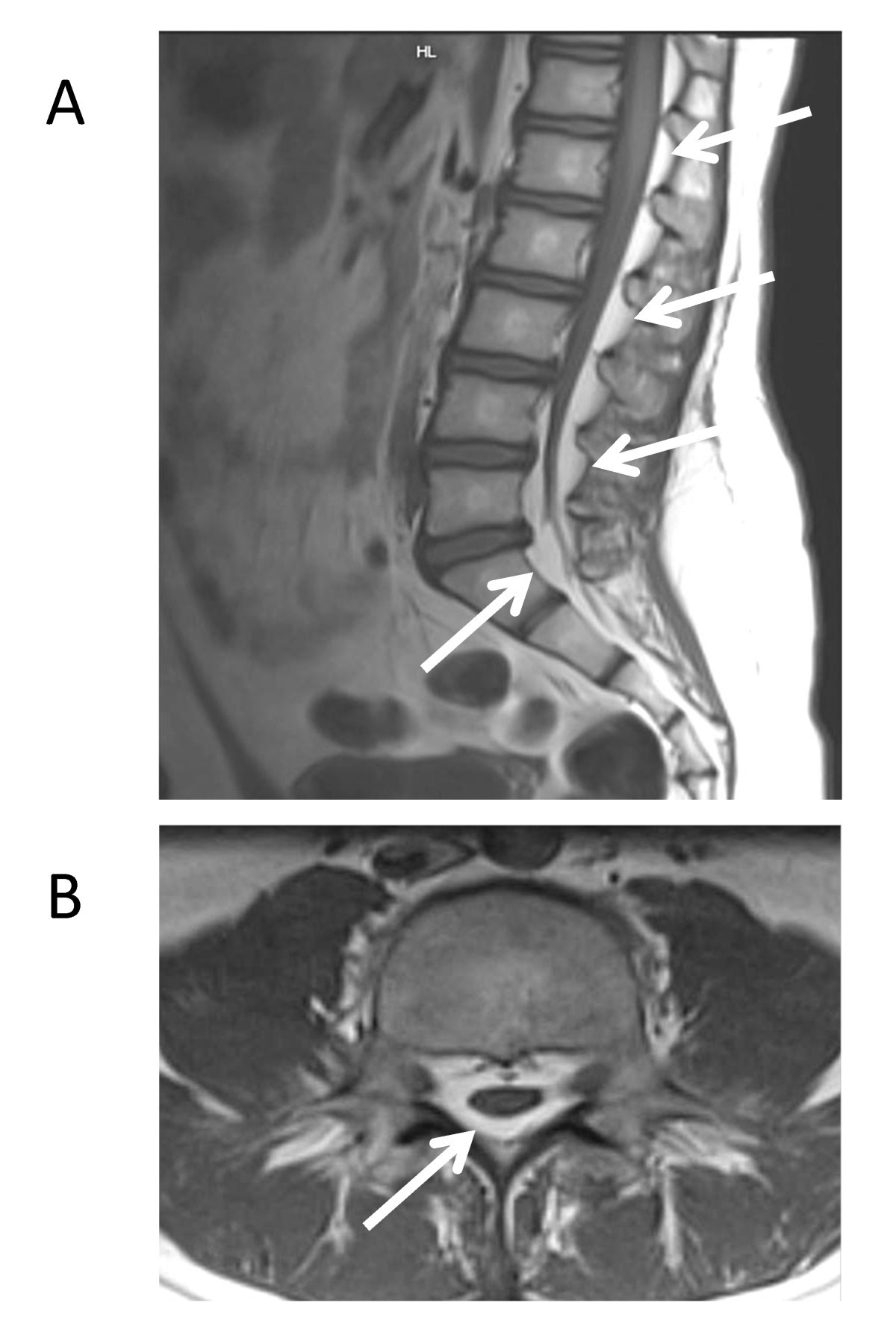
Spinal epidural lipomatosis (SEL) is a relatively rare but well-known condition characterized by the overgrowth of epidural adipose tissue within the spinal canal (Figure 1).
How many people have epidural lipomatosis?
Idiopathic epidural lipomatosis is extremely rare (7.6%) and the precise etiopathogenesis is still not known [4, 14, 17]. Borre et al.
Is epidural lipomatosis common?
Epidural lipomatosis is a rare disorder in which an abnormal amount of fat is deposited on or outside the lining of the spine. It may press on the spinal cord and nerves.
How is epidural lipomatosis diagnosed?
The most sensitive test is advanced imaging, specifically T1-weighted magnetic resonance imaging (MRI). Historically, the “Y” sign or polygonal deformations of the dural sac have been specific for SEL. These pathognomonic signs on MRI are caused by thecal sac compression due to excess epidural fat.
What is thoracic epidural lipomatosis?
Thoracic spinal epidural lipomatosis (SEL) involves the pathological overgrowth of histologically normal, unencapsulated adipose tissue that can compress the spinal cord and cause myelopathy. SEL has been associated with multiple medical conditions, including Scheuermann kyphosis (SK).
Is laminectomy the same as decompression?
Cervical laminectomy Laminectomy is surgery that creates space by removing the lamina — the back part of a vertebra that covers your spinal canal. Also known as decompression surgery, laminectomy enlarges your spinal canal to relieve pressure on the spinal cord or nerves.
What is the meaning of lipomatosis?
A lipoma is a slow-growing, fatty lump that's most often situated between your skin and the underlying muscle layer. A lipoma, which feels doughy and usually isn't tender, moves readily with slight finger pressure. Lipomas are usually detected in middle age. Some people have more than one lipoma.
How serious is stenosis of the spine?
Spinal stenosis is a condition that results in the narrowing of the spinal column, often accompanied by painful, debilitating compression of the spinal cord as well as nerve roots. For some people, the pain can be so severe it is incapacitating, making even everyday activities nearly impossible.
What is the ICD 10 code for epidural lipomatosis?
Lipomatosis, not elsewhere classified E88. 2 is a billable/specific ICD-10-CM code that can be used to indicate a diagnosis for reimbursement purposes. The 2022 edition of ICD-10-CM E88. 2 became effective on October 1, 2021.
What is the condition where fat is deposited on the spine?
Epidural lipomatosis is a rare disorder in which an abnormal amount of fat is deposited on or outside the lining of the spine. It may press on the spinal cord and nerves.
Can epidural lipomatosis cause a loss of sensation?
Other possible signs may be a loss of sensation or reflexes that are too slow or too fast. Epidural lipomatosis affects men more than women. Patients who have used steroids for many years as treatments for conditions like asthma are more likely to get this condition. Being overweight may contribute to it.
What is epidural lipomatosis?
ONSET: Epidural lipomatosis is a rare disorder defined as a pathological overgrowth of normal epidural fat. It is more often associated with administration of exogenous steroid with variable duration and doses. Furthermore, it may occur in some patients in the absence of exposure to steroids but generally associated with obesity.
What is the best imaging for lipomatosis?
MRI is considered the imaging procedure of choice, allowing an assessment of the extent of lipomatosis and, as well as CT, an identification of the lipomatous tissue. Most cases of epidural lipomatosis with corticosteroid use occur in the thoracic region, while most idiopathic cases occur in the lumbar region. ...
Is epidural lipomatosis a metabolic disorder?
The pathogenesis of epidural lipomatosis remains unknown but different suggested hypotheses may lead to a metabolic disorder as the underlying cause.
What is the best treatment for lumbar SEL?
Lumbar laminotomy and replantation provide an ideal option to treat lumbar SEL because it can achieve sufficient and effective decompression, simultaneously reconstruct the anatomy of the spinal canal, and reduce the risk of iatrogenic lumbar instability.
What is SEL in spinal surgery?
Spinal epidural lipomatosis (SEL), a rare space-occupying lesion in the spinal canal, is defined as the diffuse overgrowth of epidural adipose tissue causing spinal canal compression and neurologic deficits. [1,2]The symptoms are similar to those caused by lumbar disc herniation or lumbar spinal stenosis, such as lower back pain, numbness, pain, weakness, and cauda equina syndrome.[3] Surgical interventions will be suggested when patients exhibit acute neurological deterioration or when conservative treatment is ineffective. Fenestration or laminectomy with epidural fat debulking is a routine surgical procedure according to the literature,[4,5]which damages the structure of the posterior spine and affects stability. In the current report, we present a case of lumbar SEL (L3–L5); lamina osteotomy and replantation in situ were performed, and the patient showed significant improvement in neurological symptoms and low back pain postoperatively.
Is lumbar SEL surgery safe?
At present, there is no uniform consensus on the surgical treatment of symptomatic lumbar SEL, and the surgical approach depends on the specific situation of the patient. The technology of laminotomy and replantation for lumbar SEL can achieve a sufficient and effective decompression, and at the same time, reconstruct the anatomy of the spinal canal. It has the advantages of better maintenance of lumbar stability, preservation of mobility, and reduction of adjacent segment degeneration. Therefore, it is an effective and safe treatment option.