Monoclonal antibody therapy
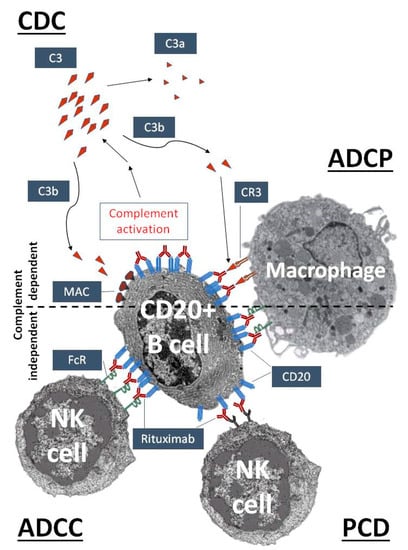
Monoclonal antibody therapy is a form of immunotherapy that uses monoclonal antibodies (mAb) to bind monospecifically to certain cells or proteins. This may then stimulate the patient's immune system to attack those cells. Alternatively, in radioimmunotherapy a radioactive dose localiz…
How soon should you get monoclonal antibodies?
May 27, 2021 · An allergic reaction may happen as a side effect of monoclonal antibody treatment. These reactions usually only happen during or shortly after the treatment, and your Care Team will be on the lookout for any signs of an allergic reaction in the post-treatment observation time.
Are there side effects of monoclonal antibody treatment?
Jan 06, 2022 · Monoclonal antibody therapy is a way of treating COVID-19 for people who have tested positive, have had mild symptoms for seven days or less, and are at high risk for developing more serious symptoms. The goal of this therapy is to help prevent hospitalizations, reduce viral loads, and lessen symptom severity.
How often can you get monoclonal antibodies?
Monoclonal antibodies, or mAbs, are made in a laboratory to fight a particular infection (in this case, SARS-CoV-2) and are given to you directly in an infusion. So the mAb treatment may help if you are at high risk for serious symptoms or a hospital stay. The mAb treatment for COVID-19 is different from a COVID-19 vaccine.
What are monoclonal antibodies and how do they work?
Feb 06, 2022 · Monoclonal antibodies used for the treatment of COVID-19 target the viral spike protein, which prevents viral entry. Monoclonal antibody therapy reduces deaths and hospitalizations in non-hospitalized patients with risk factors for severe disease progression.
How do monoclonal antibodies work against COVID-19?
Monoclonal antibodies for COVID-19 may block the virus that causes COVID-19 from attaching to human cells, making it more difficult for the virus to reproduce and cause harm. Monoclonal antibodies may also neutralize a virus.Mar 31, 2022
How long do COVID-19 antibodies last?
At this time, it is unknown for how long antibodies persist following infection and if the presence of antibodies confers protective immunity.Jan 31, 2022
What is the difference between monoclonal antibodies and the COVID-19 vaccine?
COVID-19 vaccines help stimulate and prepare a person's immune system to respond if they are exposed to the virus. However, monoclonal antibodies boost the immune system only after a person is already sick, speeding up their immune response to prevent COVID-19 from getting worse.Nov 8, 2021
Can I get the COVID-19 vaccine if I was treated with monoclonal antibodies or convalescent plasma?
If you were treated for COVID-19 symptoms with monoclonal antibodies or convalescent plasma, you should wait 90 days before getting a COVID-19 vaccine.
Can you get COVID-19 if you already had it and have antibodies?
It is important to remember that some people with antibodies to SARS-CoV-2 may become infected after vaccination (vaccine breakthrough infection) or after recovering from a past infection (reinfected).Nov 10, 2021
How long do antibodies last in people who have mild COVID-19 cases?
A UCLA study shows that in people with mild cases of COVID-19, antibodies against SARS-CoV-2 — the virus that causes the disease — drop sharply over the first three months after infection, decreasing by roughly half every 36 days. If sustained at that rate, the antibodies would disappear within about a year.
Should you still get the COVID-19 vaccine if you were treated with monoclonal antibodies?
If you were treated for COVID-19 with monoclonal antibodies or convalescent plasma, there is no need to delay getting a COVID-19 vaccine.Feb 17, 2022
Do I need the COVID-19 vaccine if I still have antibodies?
Yes, the COVID-19 vaccines are recommended, even if you had COVID-19.Nov 23, 2021
How many types of monoclonal antibody COVID-19 treatments are there in the US?
In the United States, there are three anti-SARS-CoV-2 monoclonal antibody treatments with FDA Emergency Use Authorization (EUA) for the treatment of COVID-19: bamlanivimab plus etesevimab, casirivimab plus imdevimab,, and sotrovimab.
What medication is not recommended before vaccinations for COVID-19?
It is not recommended you take over-the-counter medicine – such as ibuprofen, aspirin, or acetaminophen – before vaccination for the purpose of trying to prevent vaccine-related side effects. It is not known how these medications might affect how well the vaccine works.
Who should not take the Pfizer-BioNTech COVID-19 vaccine?
If you have had a severe allergic reaction to any ingredient in the Pfizer-BioNTech COVID-19 vaccine (such as polyethylene glycol), you should not get this vaccine. If you had a severe allergic reaction after getting a dose of the Pfizer-BioNTech COVID-19 vaccine, you should not get another dose of an mRNA vaccine.
What are the contraindications to the COVID-19 vaccine?
Contraindications to COVID-19 vaccination include: Severe allergic reaction (e.g., anaphylaxis) after a previous dose or to a component of the COVID-19 vaccine. Known diagnosed allergy to a component of the COVID-19 vaccine (see Appendix C for a list of vaccine components).
What are monoclonal antibodies?
Our bodies naturally make antibodies to fight infections. However, if you haven’t received the COVID-19 vaccine or had a previous COVID-19 infection, your body will not have antibodies designed to recognize a new virus like SARS-CoV-2.
How does monoclonal antibody therapy help?
Monoclonal antibody therapy is a way of treating COVID-19 for people who have tested positive, have had mild symptoms for seven days or less, and are at high risk for developing more serious symptoms.
Who is eligible for monoclonal antibody therapy?
Given that COVID-19 vaccination provides strong protection against severe disease and need for hospitalization, monoclonal antibody therapy is an option for certain high-risk patients with COVID-19.
WHAT IS A MONOCLONAL ANTIBODY?
Your body naturally makes antibodies to fight infection. However, your body may not have antibodies designed to recognize a novel (or new) virus like SARS-CoV-2, the virus that causes COVID-19.
How Can I Get Monoclonal Antibodies?
To receive a mAb you should be referred for treatment by your healthcare professional and directed to available infusion locations. If you do not have a healthcare provider, call the Combat COVID Monoclonal Antibodies Call Center at 1-877-332-6585 to find out who to talk with about your symptoms and treatment.
WHAT IF I DO NOT QUALIFY FOR MONOCLONAL ANTIBODY TREATMENT?
Your healthcare professional may decide you do not qualify for mAb treatment. There could be several reasons for this. You may not meet all eligibility criteria or you may have an underlying health condition that disqualifies you for mAb treatment.
WHAT CAN I EXPECT FROM TREATMENT (INFUSION)?
The mAb treatment is usually offered at an infusion center because the treatment is given through an intravenous (IV) infusion or shots. Depending on the mAb treatment you receive, the whole process takes about 1-3 hours, depending on the treatment..
CAN MONOCLONAL ANTIBODY TREATMENT MAKE ME SICK?
Antibody treatments do not contain any live SARS-CoV-2, so there is no risk you will get COVID-19 from mAb treatment. However, the antibody treatment may have side effects:
What is the function of antibodies?
Antibodies are proteins that exist in our bodies as part of our immune system to recognize and defend against harmful viruses and bacteria. Monoclonal antibodies are made in a laboratory and designed to target a specific virus or bacteria.
What antibody is used to block the virus?
Monoclonal antibodies against COVID-19 attach to the virus to block it from entering human cells. The monoclonal antibody protein also “marks” the virus to be broken down by the immune system and cleared from the body.
Can monoclonal antibodies cause nausea?
Most people tolerate monoclonal antibody infusions very well. Some people may experience infusion-related side effects, such as nausea and dizziness, that are short-lived and go away on their own. As with any medication, there is the potential for mild or more severe allergic reactions, which are uncommon.
Overview
Monoclonal antibodies (also called moAbs or mAbs) are proteins made in laboratories that act like proteins called antibodies in our bodies. Antibodies are parts of your immune system. They seek out the antigens (foreign materials) and stick to them in order to destroy them.
Procedure Details
In most cases, monoclonal antibodies are given mostly as intravenous (IV) solution injected right into your vein (sometimes referred to as an infusion). They’re often given in an infusion center where there are several people getting treatment at one time.
Recovery and Outlook
Infusion times can vary. As an example, though, monoclonal antibody treatment for COVID-19 under Emergency Use Authorization took about an hour for infusion and then another hour or so to watch for any reaction to the infusion.
When to Call the Doctor
If you’ve had a monoclonal antibody treatment, and you’re having an expected reaction, call your healthcare provider or go to an emergency room.
How long does it take for monoclonal antibodies to be administered?
The IV infusion involves placing a needle in a vein and gradually sending the medicine through the IV and into the body. The infusion takes about an hour.
What is the effect of monoclonal antibodies on the virus?
When monoclonal antibodies attach to the spike protein, they can block the virus's ability to enter cells — and slow down the infection. In 2020, the FDA authorized several different monoclonal antibodies to treat COVID-19. UPMC received two monoclonal antibody infusion treatment products.
What are the side effects of bamlanivimab?
The most common reported side effects for bamlanivimab/etesevimab are: The most common reported side effects for casirivimab/imdevimab are: IV infusions can also cause brief pain, bleeding, skin bruising, soreness, swelling, and infection at the infusion site. Monoclonal antibodies may cause other side effects.
What is monoclonal antibody?
Monoclonal antibodies are just like your body's antibodies but selected for their strong ability to resist the virus. They are produced like a medication and help your body fight illness. In 2020, the Food and Drug Administration issued an emergency use authorization to permit monoclonal antibodies as a treatment option for COVID-19.
Can IV infusions cause bruising?
Pneumonia. IV infusions can also cause brief pain, bleeding, skin bruising, soreness, swelling, and infection at the infusion site. Monoclonal antibodies may cause other side effects. Talk to your doctor if you experience any side effect that bothers you or does not go away quickly.
Does monoclonal antibody reduce the risk of death?
An analysis of UPMC patients who received monoclonal antibodies found the treatment has significantly cut the risk of hospitalization and death from COVID-19. Read more about this study.
What exactly is in a monoclonal antibody treatment and how do they work?
In the United States, there are three monoclonal antibody treatments with FDA emergency use authorization for the treatment of COVID-19: bamlanivimab plus etesevimab, developed by Eli Lilly; casirivimab plus imdevimab, made by Regeneron Pharmaceuticals; and sotrovimab, which is manufactured by GlaxoSmithKline.
Who is eligible for monoclonal antibody treatment?
If you believe you are at high risk for progression of severe COVID-19, including hospitalization or death, you may be eligible for the the COVID-19 antibody cocktails.
How effective is it?
Ginde said it can be a life-saving treatment when administered in time. Numerous trials have shown that the treatment can be effective at reducing the risk of hospitalization and death for people at risk of severe COVID.
When do I need to get the treatment in order for it to work?
The monoclonal antibody treatments are meant for mild to moderate COVID cases in adults and children over 12 to prevent the progression of severe COVID.
How can I get a monoclonal antibody treatment for COVID-19?
The ease of access varies state by state, as the Department of Health and Human Services determines how much of the national supply gets distributed on a weekly basis. Then, different state and territorial health departments decide which areas receive it and how much.
Are there side effects?
It’s rare but possible to have side effects. At least 1% of subjects receiving Regeneron’s antibody cocktail in a Phase 3 trial got skin redness and itchiness at the injection site, according to the FDA.
How much does it cost?
The federal government is covering the cost of the monoclonal antibody therapies, so it is free to get, but there might be an administration cost billed to your insurance if you have one.